Lithium Increases the Volume of the Prefrontal Cortex in Responders
 Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
This study reported that patients whose illness failed to respond to lithium had smaller right amygdalas than euthymic bipolar I patients or healthy controls. After treatment with lithium, those who responded well to the drug showed significant enlargement of the left prefrontal cortex and the left dorsolateral prefrontal cortex, while those who responded poorly to lithium showed decreases in the volume of their left hippocampus and right anterior cingulate cortex.
Editor’s Note: This is one of several studies that suggest a relationship between volume of brain regions and degree of response to lithium. These data add to the remarkably consistent literature suggesting that lithium may have neurotrophic and neuro-protective effects, potentially because of the drug’s ability to increase neuroprotective factors such as BDNF and Bcl-2 while decreasing cell death factors such as BAX and p53.
How Illness Progresses In The Recurrent Affective Disorders
This editor (RM Post) in collaboration with Jacqueline Fleming and Flavio Kapczinski published the article “Neurobiological mechanisms of illness progression in the recurrent affective disorders” in the Journal of Psychiatric Research this year. The article built on several themes about the progression of bipolar illness that had been explored in previous research.
These themes include:
- The likely acceleration of repeated episodes as a function of the number of prior episodes (episode sensitization)
- The increased responsivity of the illness to repeated stressors (stress sensitization)
- The increased behavioral reactivity to repeated use of psychomotor stimulants such as cocaine (stimulant-induced behavioral sensitization)
Not only are these observations well documented in the scientific literature, but recent observations also suggest that each type of sensitization can show cross-sensitization to the other two types. That is, individuals exposed to repeated stressors are more likely both to experience affective illness episodes and to adopt comorbid substance abuse. In a similar way, episodes of an affective disorder and stressors may also be associated with the relapse into drug administration in those who have been abstinent.
In addition to these mechanisms of illness progression in the recurrent affective disorders, the new article reviews the literature showing that the number of affective episodes or the duration of the illness appear to be associated with a variety of other clinical and neurobiological variables.
The number of affective episodes a patient experiences is associated with the degree of cognitive dysfunction present in their bipolar illness, and experiencing more than 4 episodes of unipolar or bipolar depression is a risk factor for dementia in late life. A relative lack of response to most treatments is also correlated with the number of prior episodes, and this holds true for response to naturalistic treatment in general. While most of these data are correlational and the direction of causality cannot be ascertained for certain, it is likely that the number of affective episodes and/or their duration could account for and drive difficulties with treatment and with cognitive function.
If this were the case, one would expect to see a variety of neurobiological correlates with the number of prior episodes or duration of illness, and in the article we summarize those that have been found in unipolar and bipolar disorder. Considerable data indicate that cortical volume and degrees of prefrontal cortical dysfunction can vary as a function of number of prior episodes. There is evidence that increased activity of the amygdala and the nucleus accumbens are also related to episodes or duration of illness. In those with unipolar depression, the volume of the hippocampus is decreased with longer duration of illness. Read more
Cortex Shrinks and Amygdala Grows in Childhood Bipolar Disorder
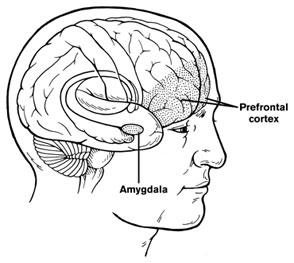 At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
Chang cited the study of Singh et al. (2010) who found that the subgenual anterior cingulate volume early in the course of illness was smaller in adolescent-onset bipolar disorder compared to controls. Given this evidence of prefrontal cortical and anterior cingulate deficits, Dr. Chang raised the possibility that treatment with lithium and other agents with potential neurotrophic and neuroprotective effects might be able to prevent these neurobiological aspects of illness progression in young patients.


