Scopolamine Produces Larger Antidepressant and Antianxiety Effects in Women Than in Men
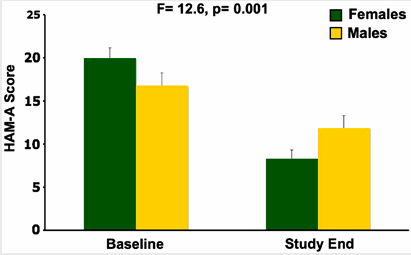
In a study published in Neuropscyhopharmacology, three sessions of intravenous scopolamine (4µg/kg over 15 minutes) led to rapid antidepressant response in both men and women, but the magnitude of response was larger in women. Women also experienced significant reduction in anxiety, as seen below:
Editor’s Note: Scopolamine is a potent blocker of acetylcholine receptors of the muscarinic type. This can cause side effects such as dry mouth and constipation. However, when given intravenously, scopolamine produces rapid onset of antidepressant effects in both bipolar and unipolar depressed patients. This study suggests that the drug may be even more effective in women.
Thyroid Augmentation May Improve Depression in Women with Treatment-Resistant Bipolar Depression
 We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
Overall, T4 had no statistically significant effect that differentiated it from placebo, but among women, there was a significantly greater degree of improvement in the Hamilton Rating Scale for Depression scores for those on T4 (-42.4%) than for those on placebo (-16.6%), p= .018.
Editor’s note: This study is the first randomized, placebo-controlled trial of supra-physiological doses of T4. A small series of reports in the literature from several different investigative groups had previously suggested efficacy of this compound in rapid cycling and treatment-resistant patients. Read more
Depression More Likely Among Perimenopausal Women with Bipolar Disorder
Researchers found that among women with bipolar disorder, those in the menopausal transition period were significantly more likely to be depressed than premenopausal women in the sample, and that the increased proclivity for depression continued in post-menopausal women as well. Wendy Marsh, Terrence Ketter, Sybil Crawford, Julia Johnson and Anthony Rothschild studied 521 women of reproductive age, 107 women in the menopausal transition period, and 145 post-menopausal women in a multi-site treatment enhancement program for bipolar disorder (STEP-BD).
The women of reproductive age ranged from 28-38 years old, and the women in the menopausal transition period averaged 42 years old and 365 days past their last menstrual period.
Women in the menopausal transition were less likely to experience a manic episode compared with reproductive aged women, and those who were post-menopausal had the least likelihood of experiencing a manic episode. These data are consistent with others in the literature that suggest that the menopausal transition may be associated with an increased proclivity to depressive episodes.
These data also raise the question of whether hormone replacement therapy in the late menopausal transition phase may be a useful adjunct for treatment-resistant depression.
Thyroid Augmentation Helps Depression (And Bipolar Disorder in Women)
Low dose thyroid replacement treatment with T3 (Cytomel) (25-37.5 µg) is typically recommended for acute antidepressant augmentation in unipolar and bipolar depression. This approach has few side effects and works even in those with normal thyroid function at baseline.
Some data also supports the use of relatively high (supraphysiological) doses of T4 (Synthroid) late in the treatment of highly treatment-resistant patients with unipolar and bipolar disorder. These supra-physiological doses of T4 typically ranged from 300-500 µg/day, producing a free thyroxine index of 150% of normal. This is usually moderately well tolerated, although minor degrees of sweating, tachycardia (fast heartbeat), and other signs of hyperthyroidism can accompany this regimen. If this approach is employed, it is particularly important to increase the dose of T4 (Synthroid) very slowly because of its relatively long half-life—about 12 days. (That is, if a patient takes a high dose of T4 and then stops their medication completely, 12 days later blood levels will only have decreased to half of what they originally were.)
Findings about high-dose T4 for women with treatment-resistant bipolar illness after the jump. Read more
Inflammation in the Affective Disorders
Bipolar children exhibit more inflammation than healthy children, according to a paper presented by Pandey, Dwivedi, and Pavuluri from the University of Illinois at the American College of Neuropsychopharmacology in December 2009.
In “Pro-inflammatory cytokines in plasma of patients with pediatric bipolar disorder,” the researchers described their study in which 21 normal controls were compared with 22 children with pediatric bipolar disorder who were unmedicated for a period of at least two weeks. The level of the inflammatory cytokine interleukin-1b (IL-1b) was significantly higher in the pediatric bipolar patients compared with controls, and levels of TNF alpha, another inflammatory marker, were significantly higher as well. Not only is this evidence of increased inflammatory processes in pediatric bipolar disorder, but TNF alpha is associated with activation of transcription factors and the initiation of preprogrammed cell death, or apoptosis.