Study Examines Comorbidity of ADHD and Bipolar Disorder

In a 2021 review and meta-analysis in the journal Neuroscience and Biobehavioral Reviews, researcher Carmen Schiweck and colleagues described the comorbidity of attention-deficit hyperactivity disorder (ADHD) and bipolar disorder in adults. This was the first review and meta-analysis to quantify the comorbidity of the two fairly prevalent disorders. The meta-analysis included 71 studies with a combined total of 646,766 participants from 18 countries.
The review found that among people with ADHD, about 1 in 13 also have bipolar disorder, while among people with bipolar disorder, 1 in 6 have comorbid ADHD. The prevalence differed depending on the continent where patients lived and the diagnostic systems used there, with greater prevalence of both disorders in the US, where the Diagnostic and Statistical Manual of Mental Disorders is used, than in Europe, where the International Classification of Diseases is typically used. (Other parts of the world were less represented in the meta-analysis.) Schiweck and colleagues found that bipolar disorder had an onset about 4 years earlier in patients who had comorbid ADHD.
Insomnia Plays Critical Role in Bipolar Disorder

In a 2021 article in the Journal of Psychiatric Research, researcher Laura Palagini and colleagues reported that insomnia symptoms can affect the course of bipolar illness. In a helpful summary and interview in the Psychiatry & Behavioral Health Learning Network’s Psych Focus, she stated that:
“1) BD patients in a depressive phase with clinically significant insomnia met a greater severity not only of depressive symptoms and suicidal risk, but also of early life stressors and the cognitive part of hopelessness, compared with patients without insomnia
“2) insomnia symptoms could predict mood symptoms, suicidal ideation and plans, and the cognitive component of hopelessness
“3) insomnia symptoms might mediate the effect of early life stressors on mood symptoms, hopelessness, and suicidal ideation and behaviors.”
Palagini suggested that “Insomnia symptoms should be easily addressed in clinical practice with 1–2 questions. Insomnia treatment should be considered as a treatment to prevent …relapse and recurrence [of bipolar disorder] and to prevent suicide and the effect of early life stress on [bipolar disorder].”
Editor’s Note: Regular nightly rating of mood, functioning, hours of sleep, medications, life events, side effects, and other comorbid symptoms on the Monthly Mood Chart Personal Calendar (pdf) is an easy way for patients with bipolar disorder to carefully track their illness trajectory and the completeness of their response to medications.
A decrease in the hours of sleep should be used as a possible early warning sign of impending difficulties, or even a new episode. Patients should discuss with their physician the threshold of insomnia (such as the loss of 2 hours of sleep for two days in a row) that should trigger a call to the physician, and what interventions the patient might initiate for lesser amounts of sleep loss and/or changes in mood. Heading these off early may prevent the breakthrough of a full-blown manic or depressive episode.
Early Precursors of Mood Disorders in Young Children of Parents with Bipolar or Unipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Caroline Vandeleur presented findings from a 13-year study of children in Switzerland who have a parent with bipolar disorder or major depressive disorder. In contrast to findings from the US presented by Danella Hafeman, Vandeleur and colleagues found no evidence of psychopathology in 4 year-olds. They did find that in 7-year-olds, children of a parent with major depressive disorder were four times more likely to have a separation anxiety disorder. In an overall sample of 449 children with a mean age of 10 who were followed up for 13 years, major depression tended to be preceded by anxiety disorders. Participants who went on to be diagnosed with bipolar disorder had earlier symptoms of depression, subthreshold hypomania, conduct disorders, and drug abuse. These were especially common in those who had a parent with bipolar disorder.
Editor’s Note: These data indirectly confirm other observations in which children at high risk for mood disorders in the US showed earlier signs of psychopathology than those in other countries including the Netherlands and Canada.
Danish Population-Based Study Identifies New Drug Candidates for Bipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, Lars Kessing of the Psychiatric Center Copenhagen described a study that examined incidence of bipolar disorder among a total of 1,605,365 participants who purchased one of six common medications over a ten-year-period, with the goal of identifying drugs that might be repurposed to prevent or treat bipolar illness. The drugs were non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen), low-dose aspirin, high-dose aspirin, statins, allopurinol, and angiotensin.
Because Denmark has population-based healthcare data, the researchers were able to identify participants who purchased these medications between 2005 and 2015, and could also assess these participants for two outcome measures: 1) whether they had received a diagnosis of mania or bipolar disorder as an inpatient or outpatient at a psychiatric hospital, and 2) a combined measure of whether they had received a diagnosis for mania or bipolar disorder in any setting or initiated lithium use. The data on these participants were compared to a random sample of 30% of the population of Demark.
Kessing and colleagues found that among those with steady use of low-dose aspirin, statins (used to lower blood cholesterol), and angiotensin agents (which can lower blood pressure), there was a significant decreased incidence of mania/bipolar disorder on both outcome measures.
In contrast, among those taking non-aspirin NSAIDs and high-dose aspirin, there was an increased incidence of bipolar disorder. (There were no statistically significant findings with regard to allopurinol, which is used to treat gout and kidney stones.)
The researchers concluded that population-based studies such as these can be used to identify drugs that may have secondary benefits, in this case low-dose aspirin, statins, and angiotensin agents, which have already been identified as potentially therapeutic in other research.
Cognitive Abnormalities in Patients Recently Diagnosed with Bipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Kamilla Miskowiak described a study in which she and her colleagues grouped 158 patients in remission from recently diagnosed bipolar disorder into groups based on their neurocognitive functioning and particularly their emotional processing, and also observed cognitive function in 52 first-degree relatives of those with bipolar disorder. These groups were compared to 110 healthy control participants.
Miskowiak and colleagues identified three clusters among the patients with bipolar disorder: 23% were globally impaired, 31% were selectively impaired, and 46% had normal cognition. Those who were globally impaired had problems recognizing facial expressions in social scenarios. Cognitive impairment has previously been documented in patients who have had a longer duration or more episodes of bipolar illness.
First-degree relatives of cognitively impaired patients had impaired recognition of facial expressions, but their cognition in non-emotional areas was normal. Miskowiak and colleagues concluded that the impaired affective cognition in relatives of patients with neurocognitive impairment was an indication of inherited risk for bipolar disorder.
Editor’s Note: Children with bipolar disorder also have this deficit in facial emotion recognition. That 23% of recently diagnosed patients with bipolar disorder were globally impaired indicates that some cognitive impairments can emerge early in the course of bipolar disorder. Researcher Lakshmi Yatham has previously found that cognition improves after a first episode of mania only if no further episodes occur in the one year following, indicating that episode prevention is crucial even after a patient’s first episode.
White Matter Disturbances in Bipolar Disorder
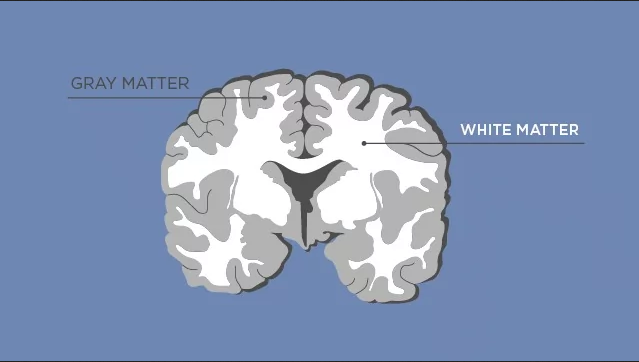
At the 2020 meeting of the International Society for Bipolar Disorders, researcher Clare Beasley described the cellular and molecular underpinnings of the white matter abnormalities typically seen in children and adults with bipolar disorder. Researchers consistently see white matter abnormalities in neuroimaging studies of bipolar disorder, but not much is understood about what creates these deficits.
Beasley and colleagues studied autopsy specimens and found that compared to controls, people with bipolar disorder had a number of abnormalities affecting glial cells, lipid composition, and axons.
The researchers found increased density of oligodendrocytes (glial cells that produce the myelin that wraps around axons, the long fibers of nerve cells where impulses travel out to other cells) and an associated protein called CNP in the prefrontal cortex. The myelin is what makes up white matter, while gray matter consists of cell bodies of neurons and glial cells.
People with bipolar disorder also had differently-shaped astrocytes, another type of glial cell that abuts synapses. The researchers found changes in lipid composition, including phospholipid and fatty acid levels, in the white matter of people with bipolar disorder. There were also problems with axons. Beasley and colleagues noted lower density of axon-associated proteins, which are involved in transport of substances along the axons in people with bipolar disorder.
The authors conclude that these data implicate specific disturbances in oligodendrocytes and axonal function associated with the white matter alterations usually seen in neuroimages of people with bipolar disorder.
Bipolar Disorder in Pregnancy and the Postpartum Period

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Veerle Bergink reported several findings from a recent meta-analysis of articles on pregnancy and bipolar disorder. Bergink and colleagues found that pregnant women with bipolar disorder have a 37% risk of a postpartum relapse, more than twice the risk of postpartum mental disorders in the general population.
Using lithium as a treatment in the first trimester of pregnancy increased risk of congenital malformations in the fetus, but the risk was much smaller than previously thought and could be monitored by ultrasound.
Bergink and colleagues also reported that in a sample of 645 women with first-onset postpartum psychosis who received followup over a period of 7 to 25 years, 43% had no subsequent severe episodes outside of the postpartum period.
Another finding was that women with postpartum severe depression or mania had abnormalities in T cells, which are important in immune response.
Childbirth and Bipolar Disorder

In an abstract for virtual presentation at the 2020 meeting of the International Society for Bipolar Disorders, researcher Ian Jones presented evidence that childbirth may trigger onset of bipolar disorder.
Jones found that 15% of women who experience postpartum mood disorders shortly after childbirth will go on to develop bipolar disorder over time. A previous diagnosis of bipolar affective disorder is the biggest predictor that a woman will be readmitted for treatment of postpartum mental illness.
In addition, one of the biggest risk factors for postpartum mental disorders is a family history of bipolar disorder in first-degree relatives. The risk of postpartum mental disorders also increases when first-degree relatives have a psychiatric illness of any kind.
Editor’s Note: These data are consistent with research on sensitization/kindling, the idea that while early mood episodes may be triggered by psychosocial stress and other endocrine factors, later episodes may emerge more spontaneously. In this case, the stress associated with childbirth can lead to a subsequent bipolar diagnosis (with or without a precipitating stressor) in the future.
The psychosocial stress of childbirth and subsequent sleep deprivation can be severe, and those with a history of a mood disorder should seek additional support during such a time.
Environment Can Leave “Molecular Scars” Via Epigenetic Processes
A 2020 review article by researchers Julia Richetto and Urs Meyer in the journal Biological Psychiatry provides a good overview of the role epigenetic modifications play in schizophrenia and related disorders.
The article provides a powerful understanding of how the environment can induce long-lasting changes in the structure of DNA (not only in schizophrenia, but also in bipolar disorder). This process, known as epigenetics, can have life-long influences on brain chemistry and behavior, and remarkably, some of these epigenetic changes can even be transmitted to the next generation.
While the sequence of DNA that one inherits from one’s parents does not change over the course of one’s life, what can change is how loosely or tightly the DNA is wound around proteins called histones, making it easier or harder to transcribe the genetic material held there. The addition of a methyl group to DNA usually inhibits transcription, while the addition of an acetyl group to histones usually facilitates transcription. These alterations in the shape of the DNA that result from environmental exposures or behavior can be passed on through generations.
Richetto and Meyer describe these chemical changes to DNA as “molecular scars,” which are left when environmental stress occurs during sensitive developmental periods. For example, patients with schizophrenia who experienced stressors in early life have higher levels of the enzyme histone deacetylase than patients who had stress or trauma later in life. Histone deacetylase would remove the acetyl groups on histones, which would inhibit gene transcription.
Other factors that have been implicated in epigenetic modifications in schizophrenia, such as DNA methylation of key developmental pathways, include pre- or post-natal stress, a challenge to a mother’s immune system during pregnancy, pre- and post-natal nutrition, exposure to drugs or toxic substances, and cannabis use in adolescence.
Richetto and Meyer suggest that epigenetics may explain why schizophrenia (and we would add bipolar disorder) can differ so much across individuals, and may help researchers and clinicians determine how best to treat different individuals.
Editor’s Note: This editor has written about how epigenetic changes can mediate sensitization to the recurrence of life stressors, episodes of mood disorder, and bouts of substance abuse, each of which can drive illness exacerbation and progression in bipolar disorder (see the 2016 article by Robert M. Post in the journal Bipolar Disorders, “Epigenetic basis of sensitization to stress, affective episodes, and stimulants: implications for illness progression and prevention”).
The chemical changes to our DNA, histones, and microRNA emphasize how important it is to begin long-term preventative treatment starting after a first episode of mania. This not only helps limit episode recurrence and the accumulation of stressors and bouts of substance use that can cause illness deterioration, but also limit the placement of these “molecular scars” on our DNA. The key to treating bipolar disorder is: prevent episodes, protect the person and the brain.
Predicting Onset of Bipolar Disorder in Children at High Risk: Part I
 At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
Symptom Progression
In offspring of parents with bipolar disorder, researcher Anne Cecilia Duffy found that symptoms in the children tended to progress in a typical sequence. Childhood sleep and anxiety disorders were first to appear, then depressive symptoms, then bipolar disorder.
Different Types of Illness May Respond Best to Different Medications
Duffy’s research also suggested links between illness features and a good response to specific medications. Those offspring who developed a psychotic spectrum disorder responded best to atypical antipsychotic medication. Those with classical episodic bipolar I disorder responded well to lithium, especially if there was a family history of lithium responsiveness. Those offspring with bipolar II (and anxiety and substance abuse) responded well to anticonvulsant medications.
If parents with bipolar disorder had experienced early onset of their illness, their children were more likely to receive a diagnosis of bipolar disorder.
The offspring of lithium-responsive parents tended to be gifted students, while those from lithium non-responders tended to be poorer students.
Comparing Risk Factors for Bipolar Disorder and Unipolar Depression
Researcher Martin Preisig and colleagues also showed that parental early onset of bipolar disorder (before age 21) was a risk factor for the offspring receiving a diagnosis of bipolar disorder. Parental oppositional defiant disorder (ODD) was also a risk factor for bipolar disorder in the offspring. The emergence of depression, conduct disorder, drug use, and sub-syndromal hypomanic symptoms also predicted the onset of mania during childhood.
Conversely, sexual abuse and witnessing violence were strong risk factors associated with a diagnosis of major (unipolar) depressive disorder. Being female and experiencing separation anxiety were also factors that predicted unipolar depression.
Predicting Conversion to Mania
Researcher Danella M. Hafeman reported that mood swings (referred to in the literature as “affective lability”), depression/anxiety, and having a parent who had an early onset of bipolar disorder were linked to later diagnoses of mania. Immediate risk factors that predicted an imminent onset of mania included affective lability, substance abuse, and the presence of sub-threshold manic symptoms.

