Update: Memantine as an Adjunct to Lamotrigine for Bipolar Depression
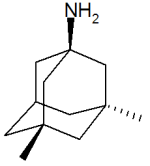
Memantine (Namenda), which is approved by the Federal Drug Administration (FDA) for use in Alzheimer’s Dementia, is increasingly being used for other conditions. Some doctors prescribe memantine for hyperactivity and attention problems in attention deficit hyperactivity disorder (ADHD), for obsessive compulsive disorder (OCD), and most recently as an adjunct to lamotrigine in bipolar depression. We wrote about the findings of Amit Anand et al. on the use of memantine and lamotrigine in January. These findings have just been published in Bipolar Disorders. The study indicates that the combination of lamotrigine with memantine brought about a rapid onset and greater magnitude of antidepressant effects than the combination of lamotrigine and placebo. The initial dose of memantine was 5mg/day, which was increased to 20mg/day during the study.
Editor’s Note: The potential mechanism of this effect makes sense. Lamotrigine decreases release of glutamate, and memantine blocks glutamate’s actions at the NMDA receptor. Thus the two together would more efficiently decrease glutamate’s effects.
It is possible that memantine could be effective without effecting the normal functions of glutamate. The drug blocks NMDA glutamate receptors that are situated away from the synapse, while allowing NMDA glutamate receptors at the synapse to fulfill their normal functions that support learning and memory. The blocking of only those receptors outside the synapse (extra-synaptic) could explain why memantine has relatively few side effects.
Thyroid Augmentation May Improve Depression in Women with Treatment-Resistant Bipolar Depression
 We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
Overall, T4 had no statistically significant effect that differentiated it from placebo, but among women, there was a significantly greater degree of improvement in the Hamilton Rating Scale for Depression scores for those on T4 (-42.4%) than for those on placebo (-16.6%), p= .018.
Editor’s note: This study is the first randomized, placebo-controlled trial of supra-physiological doses of T4. A small series of reports in the literature from several different investigative groups had previously suggested efficacy of this compound in rapid cycling and treatment-resistant patients. Read more
Lamotrigine plus Valproate: Better than Lamotrigine Alone for Bipolar Depression
In a study comparing valproate monotherapy with the combination of lamotrigine and divalproex (Valproate) extended release (ER), the combination appeared more effective in bipolar depression. At the American College of Neuropsychopharmacology meeting in December 2009, Vivek Singh, Charles Bowen, Richard Weisler, and colleagues from The University of California, San Diego reported on the randomized, double-blind, eight-month maintenance study of bipolar depressed patients.
Patients who could be stabilized for two consecutive weeks on the combination treatment of both lamotrigine and divalproex were then randomized to either lamotrigine alone or the combination for the duration of the study. Most of the data collected about these 87 subjects favored the treatment with the combination (lamotrigine plus divalproex) compared with lamotrigine alone. Combination therapy was superior for manic symptomatology and resulted in lower rates of unanticipated worsening of depression (greater than 20 points on the Montgomery-Asberg depression rating scale (MADRS)) that led to termination from the study than lamotrigine monotherapy did.
Read more
High Response Rate to Psilocybin in Bipolar II Depression
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Scott Aaronson gave 15 medication-free BP II patients (off all medications) 25mg of psilocybin with extensive therapeutic support. He saw rapid onset and persistent AD effects, such that at the end of 12 weeks 12 of the 15 patients were still in remission. Quality of life increased and suicidal ideation decreased. He indicated that others found that serum BDNF increased 1000 fold greater than baseline.
Lumateperone for Bipolar I or Bipolar II Depression: Few Extrapyramidal and Motor Symptoms
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Tobie Escher of Intra-Cellular Therapies, Inc. reported on the excellent tolerability of lumateperone (42mg/day) in a “short-term population comprised 746 patients in pooled monotherapy trials (placebo, 374; lumateperone, 372) and 352 patients in the adjunctive study (adjunctive placebo, 175; adjunctive lumateperone, 177). Reported EPS [extrapyramidal symptom]-related TEAEs [treatment-emergent adverse events] were 1 patient (0.3%) with mild dyskinesia (lumateperone monotherapy), 1 (0.6%) with mild akathisia (adjunctive lumateperone), and 1 (0.3%) with severe akathisia (placebo monotherapy).”
Greater Severity of Depression in Youth With Bipolar Disorder versus Unipolar Depression
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Aaron Silverman of the University of Toronto, CAMH found that “youth (age 13-21) with [Bipolar Disorders] compared to those with [unipolar] depression had significantly higher (more severe) ratings on depressed mood (p = .001), irritability (p = .037), anhedonia (p = .004), negative self-image (p < .001), hopelessness (p = .04), fatigue (p = .001), hypersomnia (p = .001), suicidal ideation (p = .04), and recurrent thoughts of death (p < .001).”
An Open Label Study of Synthetic Psilocybin in Bipolar Type II Depression
Highlights from Posters Presented at the Society of Biological Psychiatry Meeting, April 27-29, 2023 in San Diego
Scott Aaronson reported on patients receiving a single dose of synthetic psilocybin. All subjects had three preparatory sessions prior to dosing and three integration sessions post dosing and were followed for 12 weeks.
“At the three week primary outcome measure, 11 of 14 participants (78.6%) met remission criteria.” They concluded: “Most subjects reported significant improvement in chronic depressive symptoms without hypomania or suicidality and durability lasting for three months follow-up.”
Cannabis Use Disorder Increases Risk of Subsequent Unipolar Depression and Bipolar Disorder
Jefsen et al report in JAMA Psychiatry. that in “[6,651,765] individuals in Demark, cannabis use disorder was associated with an increased risk of (subsequent) both psychotic and nonpsychotic unipolar depression and bipolar disorder….Associations between CUD and subsequent affective disorders were estimated as hazard ratios (HRs) using Cox proportional hazards regression with time-varying information on CUD, adjusting for sex; alcohol use disorder; substance use disorder; having been born in Denmark; calendar year; parental educational level (highest attained); parental cannabis, alcohol, or substance use disorders; and parental affective disorders….Cannabis use was associated with an increased risk of bipolar disorder in men (HR, 2.96; ) and women (HR, 2.54; )”, and was highest for psychotic bipolar disorder (HR, 4.05; 95% CI, 3.52-4.65).
Editors Note: Marijuana is not a benign substance. “In all, 60,?696 individuals received a diagnosis of (cannabis use disorder) during follow-up, and 260,?746 (3.9%) developed an affective disorder.”
Fish Oil Monotherapy on Depression in Adolescents at High Risk for Bipolar I Disorder: Ambiguity Persists

Researcher Robert K. McNamara and colleagues reported in the Journal of Child and Adolescent Psychopharmacology in a 2020 article that 12 weeks of treatment with omega-3 fatty acids in the form of fish oil did not reduce depression symptoms in adolescents at risk for bipolar disorder when compared to placebo. The primary outcome measured was the results of the Childhood Depression Rating Scale-Revised (CDRS-R).
Fish oil did perform better than placebo on two parts of the rating scale: symptom severity and symptom improvement, especially in weeks 11 and 12 of the study. Omega-3 fatty acids increased creatine and choline in the anterior cingulate, and also increased polyunsaturated fatty acids in red blood cells. The treatment was safe and well-tolerated.
A total of 42 patients between the ages of 9 and 21 who had been diagnosed with depression and had at least one parent with bipolar I disorder received either placebo or 3 fish oil capsules per day. Each capsule contained 450?mg EPA, 40?mg docosapentaenoic acid (DPA), and 260?mg DHA for a total daily dose of 2130?mg EPA + DHA.
Editor’s Note: Ambiguity persists about whether omega-3 fatty acids can improve unipolar or bipolar depression, attention-deficit hyperactivity disorder (ADHD), or prevent the progression of schizophrenia symptoms to the full syndrome. Given the lack of side effects, and the documented effects on red blood cells and brain choline, clinical use of these compounds could be considered in some circumstances.
Recent Birth Cohorts May Have More Depression and Bipolar Disorder
In medicine, the ‘cohort effect’ describes the idea that more recent birth cohorts have an increased incidence and younger age of onset of their illness. A 2016 article by this editor (Robert M. Post) and colleagues in the Journal of Clinical Psychiatry presented evidence that younger patients with bipolar disorder have an earlier age of onset of bipolar disorder and more relatives with mood disorders than older patients with bipolar disorder.
The research was carried out by the Bipolar Collaborative Network in four US cities (Dallas, Cincinatti, Los Angeles, and Bethesda) and three northern European ones (Utrecht, Freiburg, and Munich). On both continents, patients born more recently had an earlier age of onset of their bipolar disorder. Younger patients also had parents and grandparents with a greater incidence of depression, bipolar disorder, and alcohol and substance abuse compared to older patients.
Editor’s Note: Other researchers have found evidence of a cohort effect for unipolar depression, substance abuse, and attention-deficit hyperactivity disorder (ADHD). The data indicate that childhood onset of psychiatric illnesses may be becoming more common. Research aimed at earlier detection and treatment is needed to reverse these trends.