BNN Editor Robert M. Post Wins Mogens Schou Award for Research from the International Society for Bipolar Disorder
On May 4, 2017, at the annual conference of the International Society for Bipolar Disorders (ISBD) in Arlington, Virginia, Dr. Robert M. Post, Editor-in-Chief of Bipolar Network News, was presented the Mogens Schou Award for Research. It is one of the most prestigious honors in the field of research on bipolar disorder.
Mogens Schou was a Danish psychiatrist and researcher whose research in the 1950s led to lithium’s use in the treatment of bipolar disorder.
Upon the announcement of the award by Dr. Marion Leboyer, who received the Schou research award in 2011, Dr. Post received a standing ovation. The following comments are adapted from Dr. Post’s acceptance speech.
“It is the highest honor I could imagine to receive an award from the ISBD in the name of Mogens Schou. Not only did Schou pioneer the development of lithium for the recurrent mood disorders, but he beat back the British naysayers and critics (Michael Shepherd and Harry Blackwood) by conducting the definitive long-term controlled studies of lithium, and then continued to promote its benefits.
In Schou’s obituary, fellow researcher Dr. Paul Grof wrote,”What was most striking and profound about him was his love and compassion for people.” Schou himself said upon receiving an award, “For me every single patient whose life was changed radically by lithium outweighs honors and awards.”
Thus, it is only appropriate that I relay some of the new data on the broad clinical effects of lithium, especially since lithium today is used way too infrequently, particularly in the United States. This list is a bit too condensed, but LITHIUM: increases neuroprotective factors and neurogenesis (adults like me in the room are happy to know that we are still making new neurons). Lithium increases the volume of the hippocampus and cortex, and blocks cell death.
Lithium prevents mania, depression, and even recurrent unipolar depression, and reduces suicides 10-fold.
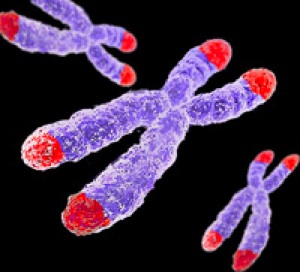
Lithium lengthens telomeres [bits on the ends of DNA that protect it during cell replication] back to normal, enhances health and longevity, decreases the incidence of some neurological diseases (including dementia), and half a pill a day for one year prevents the progression of mild cognitive impairment.
Remarkably, higher trace amounts of lithium in drinking water prevent suicide in the general population. This has now been shown in more than a half dozen studies that compare naturally occurring levels of lithium in the water in different geographic areas.
No other drug comes close to having this range of benefits. So I can only reiterate a message Schou was determined to spread in his final years: “We need to use lithium more often.”
If Schou had seen the excess of childhood-onset bipolar disorder in the United States, he would surely have lobbied for better treatment of these young people and more treatment research.
I thank the ISBD for this great honor and the opportunity to try to foster Schou’s ideals.”
Preventative Treatment Should Begin After First Manic Episode
Evidence from multiple studies has indicated the importance of beginning preventative treatment, particularly with lithium, early in the course of bipolar disorder. A 2016 comprehensive literature review by researcher Katie Joyce and colleagues in the International Journal of Bipolar Disorders concluded that psychoeducation and medication are more effective in bipolar disorder when applied in earlier stages of the illness rather than later stages.
Several studies suggest that treatment for bipolar disorder should be started specifically after the first manic episode.
A 2014 study by researcher Lars Kessing and colleagues in the British Journal of Psychiatry examined 4,700 patients treated with lithium in Denmark. Kessing and colleagues found that those who started treatment after one manic episode were less likely to find lithium ineffective than those who started later.
Another study by researcher Michael Berk and colleagues presented at the International Society for Bipolar Disorders found that after a first manic episode, a year of treatment with lithium was much more effective on all measures of outcome, including mania and depression ratings, brain imaging, and neuropsychological functioning, than a year when patients were randomized to quetiapine (Seroquel).
Researcher Lakshmi Yatham and colleagues presented research at the International Society for Bipolar Disorders showing that patients recovered from the neuropsychological deficits associated with a first episode of mania if they were well treated and had no further episodes, while those who had new episodes did not return to their baseline capabilities. This suggests that early treatment that prevents future episodes helps maintain a healthy brain.
Kessing and colleagues previously reported in the British Journal of Psychiatry in 2013 that patients randomized to two years of treatment in an outpatient clinic specializing in mood disorders following a first hospitalization for mania had 40% fewer recurrences of bipolar episodes over the next six years than those who received treatment as usual. These data indicate that early treatment, which may include psychotherapy, medications, mood charting (i.e. keeping a daily record of symptoms) and illness education, can improve the long-term course of illness. Lithium is often a key component of such treatment.
Editor’s Note: This type of intensive, ongoing treatment is not the norm after a first manic hospitalization in the United States, but it should be. Given the new data on the impact of starting lithium after a first episode of mania, and lithium’s superiority over quetiapine in the year following a first episode, lithium treatment should be standard following a diagnosis of bipolar disorder.
In the past, sometimes doctors have recommended waiting until a patient has had multiple episodes of mania before beginning preventative treatment with lithium. This now appears to be a mistake.
Lithium protects against depressive as well as manic recurrences, and there is also evidence that it increases hippocampal and cortical volume, helping prevent cognitive deterioration in those with mild cognitive impairment. Lithium is also the most effective mood stabilizer for preventing suicide, and it increases the length of telomeres (caps on the end of DNA strands), thus preventing a wide range of medical and psychiatric illnesses. Lithium may need to be combined with other drugs to achieve a complete remission, but using it after a first mania is a good place to start.
DNA Repair Plays Role in Brain Development, Cancer, and Aging
DNA has several ways of repairing itself. Serious damage, including breaks to both strands of the double helix and problems with replication, prompt a process known as DNA damage repair, or DDR. Researcher Stephen J. Elledge of Harvard Medical School won the 2015 Albert Lasker Basic Medical Research Award for his findings about DDR. He summarized these findings in a September article in the journal JAMA.
DDR occurs because of DNA’s remarkable self-awareness. Through the DDR process, DNA can detect when it has been damaged and prompt the right kind of repair. When damage occurs, DDR allows for the activation of enzymes that can remodel DNA to maintain the integrity of the genome.
When DDR pathways are activated, they can alter more than 1000 different proteins. DDR can affect immune function, blood and bone marrow, viral response, cancer, aging, and brain development.
Mutations in components of the DDR pathway can lead to problems with brain development, including Seckel syndrome (characterized by dwarfism, brain and facial abnormalities, and mental retardation) and ataxia telangiectasia (loss of control of bodily movements along with weakened immune system).
DDR is particularly relevant to cancer, since properly functioning DDR promotes a stable genome. Classic cancer treatments such as radiation and chemotherapy also rely on DDR to prompt cell death.
DDR also plays a role in aging. When we get older or have certain illnesses, telomeres, bits of material at the end of DNA strands that protect the DNA during replication, get shorter. This prompts DDR to engage in tumor prevention measures, either killing off the cells or changing them into what’s called senescent cells. Senescent cells prevent tumors, but their accumulation is associated with chronic inflammation, aging, and age-related diseases.
Editor’s Note: You can protect your telomeres and possibly hold off the age-related effects of DDR. Healthy diet, exercise, meditation, goal setting, and making positive contributions to society all help maintain telomere length. Lithium treatment also directly increases telomere length.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
Lithium Improves Medical Outcomes
Lithium is one of the most effective medications for bipolar disorder, but it has other benefits as well. At a 2015 scientific meeting, Ronald Fieve reported that among 1021 psychiatric outpatients, 570 who received long-term lithium treatment for their psychiatric illnesses had a significantly lower likelihood of certain medical conditions compared to the other outpatients who did not receive lithium therapy. The medical conditions that lithium made less likely were seizures, amyotrophic lateral sclerosis (ALS) or Lou Gehrig’s disease, dementia, and heart attack.
It is not yet know how lithium decreases these medical conditions. It may be by increasing the length of telomeres. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with stressors or psychiatric illnesses. Lithium directly increases the enzyme telomerase, which maintains telomere length. This may be one reason lithium use provides some protection from seizures, heart attacks, and other conditions.
Resilience Important for Mental Health
A symposium at the 2014 meeting of the American Psychiatric Association suggested that resilience may hold the key to healthy aging, and overcoming trauma and stress.
Resilience in Aging
Former APA president Dilip Jeste began the symposium with a discussion of successful aging. He noted the importance of optimism, social engagement, and wisdom (or healthy social attitudes) in aging. In a group of 83-year-olds, those with an optimistic attitude had fewer cardiovascular illnesses, less cancer, fewer pain syndromes, and lived longer. Those with high degrees of social engagement had a 50% increase in survival rate. Wisdom comprises skills such as seeing aging in a positive light, and having a memory that is biased toward the positive (the opposite of what happens in depression, where negatives are selectively recalled and remembered). Jeste encouraged psychiatrists to focus not just on the treatment of mental illness, but on behavioral change and the enhancement of wellbeing. He suggested asking patients not just, “How do you feel?” but instead, “How do you want to feel?”
Resilience in the Military
Researcher Dennis Charney gave a talk on resilience based on his work with people in the military, some of whom experienced post-traumatic stress disorder (PTSD). He cited a series of important principles that could enhance resilience. The first principle was to reframe adversity—assimilating, accepting and recovering from it. The second principle was that failure is essential to growth. The third principle was that altruism helps, as does a mission for the survivor of trauma. Charney suggested that a personal moral compass is also critical, whether this is based on religion or general moral principles. Other factors that are important for resilience include having a role model, facing one’s fears, developing coping skills, having a support network, increasing physical well-being, and training regularly and rigorously in multiple areas.
Charney and colleagues studied Navy SEALS who went through SERE (Survival, Evasion, Resistance, Escape) training. Those SEALS who had the highest resilience during this severe training exercise had the highest levels of the neurotransmitter norepinephrine and NPY (an antianxiety neuropeptide). NPY levels are low in people with PTSD. Charney and colleagues reasoned that giving a peptide that acted on the NPY-1 receptors intranasally (so that it could cross the blood brain barrier) might be therapeutic. In a rodent model of PTSD, the peptide prevented and reversed PTSD-like behaviors. Further clinical development of the peptide is now planned.
The Effects of Stress
Researcher Owen Wolkowitz described how stress accelerates the mental and physical aspects of aging. Telomeres are strands of DNA at the end of each chromosome that protect the DNA during each cell replication. Telomere length decreases with stress and aging. Read more
Traditional Antidepressants Are Not Effective in Bipolar Depression
 Bipolar illness affects 4.5% of the US population. According to researcher Kathleen Merikangas, 1.0% have bipolar I disorder, 1.1% have bipolar II disorder, and the remainder have subthreshold symptoms. Mark Frye, Chairman of the Department of Psychiatry at the Mayo Clinic, gave a lecture on antidepressants in bipolar illness at the 2014 meeting of the American Psychiatric Association.
Bipolar illness affects 4.5% of the US population. According to researcher Kathleen Merikangas, 1.0% have bipolar I disorder, 1.1% have bipolar II disorder, and the remainder have subthreshold symptoms. Mark Frye, Chairman of the Department of Psychiatry at the Mayo Clinic, gave a lecture on antidepressants in bipolar illness at the 2014 meeting of the American Psychiatric Association.
The newest data from meta-analyses indicate that traditional antidepressants that are effective in unipolar depression are not effective in bipolar depression. Some patient groups, especially those with very early onset depression and mixed depression, are at increased risk of switching into mania and making a suicide attempt while taking antidepressants.
Unipolar depressed patients with a genetic variation that produces a short form of the serotonin transporter (5HT-LPRs/s) are at increased risk for depression in adulthood following a history of childhood adversity, and tend to respond less well to antidepressants. Frye found that 5HT-LPRs/s is weakly associated with switching into mania when antidepressants are given to patients with bipolar depression.
At the same symposium, researcher Mike Gitlin reviewed data on combination therapy, which is rapidly becoming the norm, indicating that in most circumstances, it is superior to monotherapy.
Researcher David Miklowitz reviewed the impressive data on the superiority of most forms of targeted psychotherapy or psychoeducation compared to treatment as usual for bipolar depression. He noted his own finding that Family Focused Therapy (FFT) not only is effective in adolescents and adults with bipolar disorder, but also in reducing illness and dysfunction in those with prodromal disorders (such as depression, cyclothymia, and bipolar not otherwise specified) in situations where there is a family history of bipolar disorder.
Eight components of FFT are:
- Recognition of prodromal symptoms and development of treatment strategies for them.
- Recognition and management of stress and triggers using cognitive restructuring.
- Development of a relapse prevention plan and rehearsal of what to do.
- Regularization of sleep.
- Encouragement of treatment adherence with an eye to a good future.
- Enhancement of emotional self-regulation skills, including cognitive restructuring.
- Improvement of family relationships and communication.
- Education about substance abuse avoidance and treatment for that and other comorbidities.
Many of these are also key components of group psychoeducation, cognitive-behavioral therapy, and interpersonal and social rhythms therapy, and all of these are effective in treating and preventing bipolar depression compared to treatment as usual. It is noteworthy that in the research of Francesc Colom, 90% of patients randomized to treatment as usual relapsed within 24 months, while psychoeducation was highly effective in preventing relapses over the next five years.
This editor (Robert M. Post), the discussant for the symposium, emphasized that the main take-away messages of the speakers were: use more lithium, use more caution and fewer antidepressants in treating bipolar depression, use more combination therapy for acute illness and for maintenance, and definitely use more psychotherapy. Read more
Cynicism Linked to Dementia
A decades-long study called Cardiovascular Risk Factors, Aging and Dementia (CAIDE) observed older participants for signs of dementia, and collected data on participants’ levels of cynical distrust, for example, the belief that others will lie or cheat for personal gain and that it’s safer not to trust anyone.
A 2014 study by Elisa Neuvonen et al. in the journal Neurology reported that after adjusting for demographic and other factors, those participants with the highest levels of cynical distrust of others were at higher risk for dementia as they aged. This relationship was not explained by depressive symptoms. The authors suggest that a positive attitude may protect the brain.
The researchers acknowledge that it is possible the distrust may be a result of brain changes leading to dementia, rather than the cause of it.
Those with the highest levels of cynical distrust were also at higher risk for death, but this association disappeared when the researchers controlled for socioeconomic factors and health behaviors such as smoking.
The researchers hope to investigate whether having a cynical attitude early in life is more robustly linked to mortality. It would be exciting to determine whether a shift to a more positive attitude earlier in life could prevent dementia.
Editor’s Note: A high level of chronic anger is associated with shorter telomeres. Telomeres sit at the end of DNA strands and shorten with each cell replication. Shorter telomeres are linked to multiple medical and psychiatric disorders. It may be that cynical distrust shortens telomeres, and is thus associated with dementia.
High CRP Predicts Early Onset Of A Mood Episode
Barbara Gracious of Ohio State University became interested in the inflammatory marker CRP through studying vitamin D3 deficiency. Vitamin D is a neurosteroid, and low levels of it have been associated with risk of schizophrenia, cardiovascular disease (heart attack), diabetes, mood disorders, cognitive deficits, autoimmune disease, and obesity. High CRP levels are related to low vitamin D, to obesity, and to other inflammatory markers such as IL-6 and TNF alpha.
Gracious measured these levels of CRP in 621 children participating in the Longitudinal Study of Manic Symptoms (LAMS), who were followed up for many years. She found that those with higher levels of CRP developed a mood episode approximately two years earlier than those with normal levels. CRP binds phosphocholine, which activates complement, a kind of protein that induces inflammation. CRP is elevated in 14% to 53% of patients with depression and anxiety.
Copeland et al. reported in the American Journal of Psychiatry in 2012 that after a first depression, high CRP was associated with relapse. CRP also increases in adolescent females (who are at increased risk for depression).
Editor’s Note: These findings suggest the potential importance not only of using CRP as an indicator of depression risk, but also of targeting CRP levels in the hopes of reducing risk of a mood episode in children with elevated inflammatory markers. Supplementing vitamin D3 in those with low levels would be a good place to start, as would preventing or treating obesity and promoting good sleep hygiene and exercise. The potential role of medications with direct anti-inflammatory effects such as aspirin (acetylsalicylic acid) or minocycline deserves further study.
Balanced diet, exercise, and good sleep habits may be easier said (or recommended) than done. Such lifestyle advice must be delivered with motivational interviewing, and instilled through practice, positive feedback, encouragement, and more practice. In children in general, and especially in those at high risk for a mood episode due to a family history of a unipolar or bipolar mood disorder, starting things off right from the outset with good diet, exercise, and sleep routines would be highly recommended. The benefits for long-term health and wellbeing could be enormous.
The results of good health behaviors may be mediated through several pathways. They could lessen inflammation and obesity, increase brain-derived neurotrophic factor (BDNF, which is important for new synapses and long-term memory) and neurogenesis (both of which are increased by exercise), and even lengthen the telomeres that cap the ends of each strand of DNA (short ones are associated with a variety of medical and psychiatric illnesses).
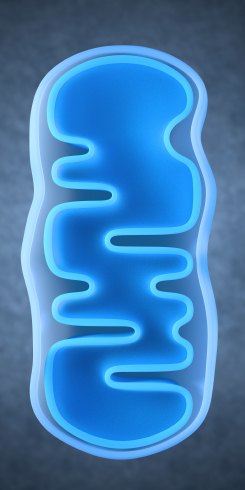
Lithium Reverses Effects of Oxidative Stress on Mitochondrial Function
Oxidative stress has been implicated in a wide range of illnesses, but what is it exactly? Our bodies use the oxygen we breathe to burn the fuel we get from food, and while this is a natural process, it produces byproducts known as free radicals, which are unstable molecules that can strip electrons from other molecules in a process called oxidation. Antioxidants (such as vitamin C) act as a source of electrons, helping keep other cells stable and healthy. Oxidative stress refers to the stress on our bodies from the normal effects of free radicals combined with environmental stressors like tobacco smoke or radiation.
In work presented at the 2013 meeting of the Society of Biological Psychiatry, Anna Andreason showed that over-activity of neurons increases oxidative stress through the production of reactive oxygen species (ROS). These are a type of free radicals that can damage cells in two ways: nitrosylation of proteins (adding nitric oxide to a thiol molecule), and oxidation, which results in more lasting effects on synaptic structures. The chemical compound rotenone damages mitochondria by producing ROS, and Andreason found that lithium was able to reverse this production and reverse the adverse effects of oxidative stress.
Lithium Has an Amazing Array of Positive Effects
Editor’s Note: The ability of lithium to protect mitochondria (the energy storehouse of a cell) adds to an increasingly long list of lithium’s neurotropic and neuroprotective benefits. Lithium increases cell survival factors BDNF and Bcl-2, increases markers of neuronal integrity such as N-Acetylaspartic acid (NAA), increases the volume of the hippocampus and cortex, and now helps protect mitochondria from oxidative stress. Lithium also increases the length of telomeres, which cap the ends of chromosome and protect them from damage during the DNA replication that occurs each time a cell divides. Short telomeres are associated with many kinds of medical and psychiatric diseases, as well as shorter life spans. No wonder that in addition to preventing mania and depression it has other clinical benefits, such as preventing memory deterioration, medical mortality, and suicide.