“Pharmacotherapy of Bipolar Depression”
Roger McIntyre gave a talk on the “Pharmacotherapy of Bipolar Depression” at the International Society for Bipolar Disorders Conference in Chicago, June 22-25, 2023
He pointed out that, contrary to the many approved agents for mania, there were few FDA-approved drugs for depression in patients with Bipolar Disorders. These approved drugs included: cariprazine (Vraylar); lumateperone (Caplyta); lurasidone (Latuda); quetiapine (Seroquel); and the olanzapine-fluoxetine combination (Symbyax). Other non-approved agents include: lithium, lamotrigine, antidepressants, MAOIs, pramipexole, carbamazepine, ketamine, bupropion+dextromethorphan, amantadine, memantine, and possibly minocycline and celecoxib. Surprisingly, more than 3,000 bipolar depressed patients have been reported to be taking ketamine and that this was not associated with the induction of hypomania or mania.
McIntyre reported on the antidepressant (AD) effects of intra-nasal (i.n.) insulin. The insulin receptor sensitizer metformin had AD effects, but only in those who converted to insulin sensitivity.
McIntyre reported on the mixed effects of the GLP-1 agonists in the prevention of depression (Cooper et al J. Psychiatric Res, 2023). This is of interest in relationship to the bidirectional relationship of diabetes mellitus and depression.
Liraglutide appeared to have an anti-anhedonia effect. Semaglutide had AD and antianxiety effects in animal models of depression.
Recent studies have explored the antidepressant effect of psilocybin. Small studies have indicated that it has rapid onset of AD effects, and, in contrast to ketamine where rapid onset AD and anti-suicidal effects are short lived, the AD effect of psilocybin may be more prolonged.
Ketamine repairs structure and function of prefrontal cortical neurons via glutamate NMDA receptor blocking action, while psilocybin and other psychedelics act via stimulating 5HT2A receptors. One single case study suggested that blocking 5HT2A receptors with trazodone could achieve a rapid onset of AD effects of psilocybin without the psychedelic effects, a very interesting finding that requires replication.
Vortioxetine Improves Cognition, Major Depression in Early Dementia
Vortioxetine (5mg then 10mg) significantly improves depressive symptoms, cognitive performance, functioning, and quality of life at 12 weeks in patients with both major depressive disorder (MDD) and early-stage dementia. In addition to blocking 5HT (serotonin) reuptake vortioxetine antagonizes 5 serotonin receptors with 5HT3 and 5HT7 likely accounting for the positive effects on processing speed and cognitive functioning.
Serotonin is Back
A review by Moncrieff et al in Molecular Psychiatry 2022 concluded that : “there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.” This was widely reported in the news media.
A new analysis by 26 experts in the field finds many faults with this analysis (Jauhar et al 2023). Instead, they conclude “A more accurate, constructive conclusion would be that acute tryptophan depletion and decreased plasma tryptophan in depression indicate a role for 5-HT in those vulnerable to or suffering from depression, and that molecular imaging suggests the system is perturbed. The proven efficacy of SSRIs in a proportion of people with depression lends credibility to this position.” Long live serotonin’s role in depression.
New Type of Antipsychotic Drug for Schizophrenia Looks Promising
In a 2020 article in the New England Journal of Medicine, researcher Kenneth S. Koblan and colleagues described a new type of antipsychotic drug treatment for schizophrenia. Almost all other antipsychotic drugs block dopamine D2 receptors, while atypical antipsychotics also block the serotonin 5HT2 receptor. They are described as antagonists at these receptors.
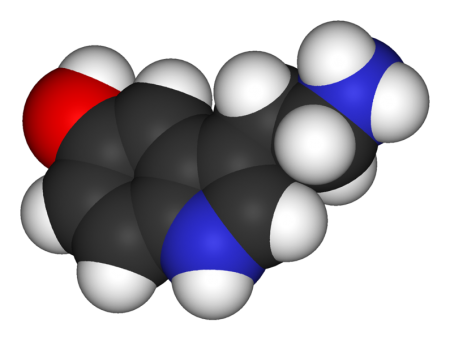
In contrast, the new drug is an agonist or activator of two different receptors. The drug SEP-363856 (also called SEP-856) activates the trace amine–associated receptor 1 (TAAR1) and 5-hydroxytryptamine (or serotonin) type 1A (5-HT1A) receptors.
Blocking D2 receptors can cause Parkinson’s-like symptoms (such as tremor, masked faces, and impaired movement or speech) and other extrapyramidal side effects (such as slurred speech, slow movements, or restless legs.) In contrast, SEP-856 seems to have a better side effects profile than these types of drugs while also being highly effective.
Patients with an acute exacerbation of schizophrenia were assigned to receive either placebo or once-daily treatment with SEP-856 (either 50mg or 75mg) for four weeks. A total of 120 patients received SEP-856 while 125 received placebo.
Compared to the placebo group, the SEP-856 group showed significantly greater reductions on a scale of positive and negative symptoms of schizophrenia by the end of the four weeks. Side effects included some sleepiness and gastrointestinal symptoms, but the incidence of extrapyramidal symptoms and changes in the levels of lipids, glycated hemoglobin, and prolactin were similar in both groups. There was one sudden death from cardiac causes in the SEP-856 group, which was not thought to be drug-related.
Editor’s Note: This drug acting on trace amine–associated receptor 1 (TAAR1) and 5HT1A receptors could herald a new and better tolerated type of antipsychotic. It is also being studied for psychosis in Parkinson’s disease. Since all of the antipsychotics that treat schizophrenia have also shown antimanic efficacy, we look forward to future studies of this unique drug in patients with mania.
Serotonin 5-HT7 Receptors: Why Should We Care About Them?
5-HT7 is a type of receptor activated by the neurotransmitter serotonin. Some of the most potent effects of lurasidone (Latuda), an atypical antipsychotic with antidepressant effects in bipolar depression, and vortioxetine (Brintellix), a unique antidepressant for unipolar depression that also has positive effects on cognition, occur through the blockade of 5-HT7 receptors. The atypical antipsychotics aripiprazole and sulpiride also act on 5-HT7 receptors.
Researcher Agnieszka Nikiforuk summarized the research to date on 5-HT7 receptors in the journal CNS Drugs in 2015.
The receptors play a role in regulating sleep and circadian rhythms, which may explain why drugs that target them can be helpful in depression. Drugs that target 5-HT7 receptors have also improved learning and memory.
One subject of research into 5-HT7 receptors is whether better results come from blocking the receptors or stimulating them.
Blockade of 5-HT7 receptors has improved depression-like symptoms in animals and enhances the effects of sub-therapeutic doses of antidepressants. In other animal studies, stimulation of the receptors has appeared promising for the prevention of age-related cognitive decline.
Antidepressant Vilazodone Superior to Placebo, Plus No Sexual Side Effects
Vilazodone (Viibryd) was approved by the Federal Drug Administration (FDA) as an antidepressant in 2011. The drug is a serotonin 5-HT reuptake inhibitor and a partial agonist of the serotonin 5-HT1A receptor like the anti-anxiety drug buspirone (Buspar). Neither buspirone nor vilazodone is associated with significant sexual dysfunction, unlike most of the antidepressants that only inhibit the serotonin transporter (selective serotonin reuptake inhibitors or SSRIs). Researcher Leslie Citrome et al. reported at the 2014 meeting of the American Psychiatric Association that at 40mg/day, the rate of remission was 32% on vilazodone versus 20% on placebo.
At the same meeting, researcher Carl Gommoll et al. reported on vilazodone’s side effects. The drug was generally well-tolerated. Side effects that occurred in 5% or more of the patients taking vilazodone and half as many taking placebo included diarrhea, nausea, vomiting, and insomnia.
New Antidepressant Vortioxetine May Improve Cognition and Treatment-Resistant Depression
Vortioxetine (Brintellix) is a new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), the most common type of antidepressants, which work only on the serotonin transporter. Researcher Johan Areberg et al. reported at the 2014 meeting of the American Psychiatric Association that the drug is an antagonist at receptors 5-HT3, 5-HT7, and 5-HT1D; a partial agonist at 5-HT1B; a full agonist at 5-HT1A; and an inhibitor of the 5-HT transporter. The researchers suggested that at doses of 5mg/day, vortioxetine occupies the 5-HT3 receptors and 50% of the serotonin transporter. As dosage increases to 20mg/day, vortioxetine is believed to occupy all of the serotonin targets at clinically relevant levels. Doses of 20mg/day were found to be effective in nine studies. Researcher Gennady Smagin et al. also reported that vortioxetine activates central histamine receptors.
Vortioxetine appears to be useful in patients who have previously failed to respond to antidepressants. Researcher George I. Papakostas et al. reported that in a cohort of about 500 patients who responded inadequately to previous prescriptions of selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs), the 252 taking vortioxetine improved more than the 241 taking the antidepressant agomelatine.
Editor’s Note: Vortioxetine’s superior effects are impressive, as agomelatine, which is approved for use in at least 41 countries including the UK, Canada, and Australia, but is not available in the US, has previously been shown to be more effective than a number of SSRIs in head-to-head comparisons. Agomelatine improves sleep and circadian rhythms via its dual effects as an agonist at melatonin M1 and M2 receptors and an inhibitor of 5HT2C receptors, which results in the release of norepinephrine and dopamine in the frontal cortex.
Vortioxetine may be unique among antidepressants in that it appears to improve cognition. Researcher John E. Harrison et al. reported that patients saw increases in executive function, attention, speed of processing, and memory while taking vortioxetine. This is consistent with studies in aged mice, whose cognition improves more on vortioxetine than on the SSRI fluoxetine, according to researcher Yan Li and colleagues.
Exercise Helpful for Mood Disorders
 While past research on mood disorders has targeted structural and functional abnormalities in the brain, newer research has considered targets such as inflammation, metabolism, and cell resilience. Exercise can have positive effects on systems that regulate metabolism, immune function, and cellular respiration, and therefore improve affective and cognitive difficulties.
While past research on mood disorders has targeted structural and functional abnormalities in the brain, newer research has considered targets such as inflammation, metabolism, and cell resilience. Exercise can have positive effects on systems that regulate metabolism, immune function, and cellular respiration, and therefore improve affective and cognitive difficulties.
At the 2014 meeting of the International Society for Bipolar Disorders, Mohammad Alsuwaidan presented a meta-analysis of the effects of exercise in mood disorders gleaned from English-language studies between 1966 and July 2008. Exercise increased brain norepinephrine, serotonin, and phenylethanolamine (PEA).
Alsuwaidan believes runner’s high, the feelings of euphoria people often experience after strenuous exercise, may not be linked to opiate (or endorphin) release, as most people believe, but instead to release of PEA or the cannabinoid anandamide, which activates CB 1 cannabinoid receptors, decreases GABA, and increases dopamine in the nucleus accumbens, the reward center of the brain.
Exercise also increases neurogenesis and the production of brain-derived neurotrophic factor (BDNF), which supports the growth of neurons and synapses. Marathon runners also have a post-race elevation in the anti-inflammatory cytokines IL-10 and IL-1Ra.
In people who are out of shape, exercise increases oxidative stress and other toxicities that do not occur with in those who exercise more regularly. Alsuwaidan extolls the benefits of high impact exercise five to seven times per week, and engaging a trainer to encourage exercise. Four minutes of intense exercise (such that you sweat and are not able to talk) is about equal to 45 minutes of mild exercise.
Ecstasy Use Increases Serotonin Receptors in Women
MDMA, better known as the drug ecstasy, has been found to reduce serotonin axons in animals. A small study by Di Iorio et al. published in the Archives of General Psychiatry in 2012 suggests that the drug also has detrimental effects on serotonin signaling in humans.
The researchers used positron emission tomography (PET) scans to identify serotonin receptors in the brains of 10 women who had never used ecstasy and 14 who had used the drug at least five times before and then abstained for at least 90 days. The team found significantly greater cortical serotonin2A receptor nondisplaceable binding potential (serotonin2ABPND, an indicator of serotonin receptors) in abstaining MDMA users than in those women who had never used the drug.
The increase in serotonin receptors observed in these ecstasy users could be a sign of chronic serotonin neurotoxicity. Loss of serotonin nerve terminals decreases serotonin levels and secondarily results in the production of more serotonin receptors. Thus, one explanation for the receptor increase is that it is prompted by the decrease in serotonin transmission that MDMA is known to cause.
The higher levels of serotonin2ABPND were found in several regions of the MDMA users’ brains: occipital-parietal, temporal, occipito-temporal-parietal, frontal, and frontoparietal. Lifetime use of the drug was associated with serotonin2ABPND in the frontoparietal, occipitotemporal, frontolimbic, and frontal regions. There were no regions in which the MDMA users had lower levels of receptors than women in the control group. The duration of the ecstasy users’ abstinence from using the drug had no effect on levels of serotonin2ABPND observed, suggesting that the effects might be long-lasting, if not permanent.
Editor’s Note: Given serotonin’s importance in brain function and the drug’s popularity for recreational use, this finding has implications both for ecstasy users and for research on serotonin signaling. Ecstasy is supposed to be a “love drug,” but people should show their serotonin nerve terminals some love and look after them by avoiding the drug.
The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more