Lithium-Induced Hypercalcemia
In a poster at the 5th Biennial Conference of the International Society for Bipolar Disorders, researchers from the Netherlands including E.J. Regeer described the prevalence of hypercalcemia (high calcium levels) in patients with bipolar disorder who are treated with lithium. In a study of 314 patients taking lithium, Regeer and colleagues found that calcium levels were elevated in 15.6% of the patients, and the length of time patients had been treated with lithium was significantly related to the degree of hypercalcemia. It is recommended that blood levels of calcium be monitored in patients on lithium.
The researchers recommended testing for parathyroid hormone in blood in order to exclude other causes of hypercalcemia. They also suggested that when lithium cannot safely be discontinued or when its discontinuation does not resolve the hypercalcemia, other treatment for high blood calcium, including removal of the parathyroid, may be necessary.
Lithium Discontinuation Results in Only Modest Improvement in Renal Function Compared to Continued Treatment
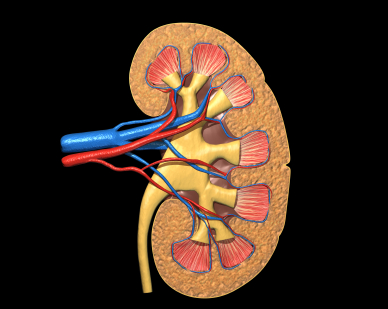 Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Editor’s Note: This study addresses one of the important unanswered questions about what to do when kidney function starts to diminish (observed as high levels of creatinine (Cr) or low Cr clearance) in patients on chronic lithium treatment.
The findings of Rej et al. suggest that the advantages of discontinuing lithium are not huge. Renal function may deteriorate a bit less (or not at all) in those who stop lithium. However, if someone is highly responsive to lithium and the “creatinine creep” upwards is slow, that patient might be able to proceed with careful monitoring and lithium continuation. Where other treatment options are readily available, the discontinuation route might be a good choice.
This study brings some much-needed randomized longitudinal data (if not a definitive recommendation) to bear on a difficult clinical decision that may have to be addressed when lithium is used in long-term approaches to bipolar disorder.
Acquired Lithium Resistance
Lithium is one of the most important treatments available for bipolar disorder. A small percentage of patients who initially respond well to lithium may develop resistance to the drug over time. Some develop tolerance to the drug’s therapeutic effects over a period of years, seen as a gradual breaking through of manic or depressive episodes that increase in severity or frequency. Others who are good long-term responders to lithium, but stop taking lithium and then suffer relapses, fail to respond as well as they had before. In a few instances, the drug no longer helps at all. This latter form of acquired lithium resistance is called lithium discontinuation-induced refractoriness.
In a review article published in the Journal of Affective Disorders in 2011, this editor (Robert Post) analyzed case series and case reports that depicted these two different types of acquired lithium resistance and reported that each must be addressed in a different way. In the case of tolerance development, a temporary break from lithium may theoretically restore its effectiveness, but the typical way to treat this situation is to add additional drugs with different mechanisms of action that are not affected by the tolerance.
In those who stop effective lithium treatment and experience relapses that are no longer responsive when lithium is re-instituted, it is not clear what the best treatment approaches are. Therefore the most conservative approach to preventive treatment with lithium is to avoid discontinuing the drug. This would appear to be a generally sound principle for the treatment of recurrent unipolar or bipolar illness. When things are going well, do not change the regimen; leave well-enough alone. Conversely, when treatment is not optimal, as in the case of loss of drug responsiveness via tolerance, a more aggressive exploration of treatment options would be warranted.
Patients should be aware of the multiple dangers of stopping effective treatment with lithium. These include: likely relapse, perhaps the necessity of hospitalization, an increased risk of suicide, and the loss of responsiveness to lithium that appears to occur in approximately 15% of patients who stop lithium when it is working effectively.
Lithium Extends Telomeres
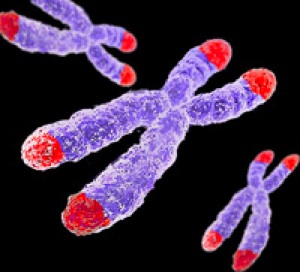 Telomeres sit at the ends of strands of DNA at each chromosome. Various events make telomeres decrease in length: cell division/replication, stress, aging, and depressive episodes in Bipolar II disorder.
Telomeres sit at the ends of strands of DNA at each chromosome. Various events make telomeres decrease in length: cell division/replication, stress, aging, and depressive episodes in Bipolar II disorder.
Martin Schalling, a professor of medical genetics at the Karolinska Institutet in Sweden, has found that lithium treatment lengthens telomeres.
Editor’s Note: This finding by Schalling, which will soon be published, adds to the list of beneficial neurobiological effects of lithium, including increasing cell survival factors BDNF and Bcl-2, decreasing cell death factors BAX and p53, increasing marker of neuronal integrity NAA, and possibly increasing hippocampal and cortical grey matter volumes.
Clinically, lithium decreases recurrence of manic and depressive episodes (mania more than depression), decreases suicidality, and may slow cognitive deterioration in those with mild cognitive impairment.
These clinical and neurobiological benefits to lithium treatment should be factored in to calculations of the risk/benefit ratio for lithium use in long-term preventative treatment of bipolar disorder.
Lithium Increases the Volume of the Prefrontal Cortex in Responders
 Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
This study reported that patients whose illness failed to respond to lithium had smaller right amygdalas than euthymic bipolar I patients or healthy controls. After treatment with lithium, those who responded well to the drug showed significant enlargement of the left prefrontal cortex and the left dorsolateral prefrontal cortex, while those who responded poorly to lithium showed decreases in the volume of their left hippocampus and right anterior cingulate cortex.
Editor’s Note: This is one of several studies that suggest a relationship between volume of brain regions and degree of response to lithium. These data add to the remarkably consistent literature suggesting that lithium may have neurotrophic and neuro-protective effects, potentially because of the drug’s ability to increase neuroprotective factors such as BDNF and Bcl-2 while decreasing cell death factors such as BAX and p53.
Minute Levels of Lithium in Public Water Supply Decrease Suicide
 Blüml et al. reported in the Journal of Psychiatric Research in 2013 that among 226 counties in Texas, the ones with higher trace levels of lithium in the public water supply had lower rates of completed suicide in the general population than did the counties with lower lithium levels. The naturally occurring lithium levels in public water supplies in the geographic regions described in this study ranged from 2.8 to 219 ?g/l or 0.00043 to 0.0315 mmol/l (much lower than the levels used to treat bipolar disorder).
Blüml et al. reported in the Journal of Psychiatric Research in 2013 that among 226 counties in Texas, the ones with higher trace levels of lithium in the public water supply had lower rates of completed suicide in the general population than did the counties with lower lithium levels. The naturally occurring lithium levels in public water supplies in the geographic regions described in this study ranged from 2.8 to 219 ?g/l or 0.00043 to 0.0315 mmol/l (much lower than the levels used to treat bipolar disorder).
This is the fourth positive study describing this effect, including two in Texas, one in Japan, and one in Austria. (One study from part of England failed to show this relationship, though levels measured in that study had a much lower and restricted range, from less than 1 to 21 ?g/l.) The most recent studies have collected more water samples and used more sophisticated statistical analyses to control for socioeconomic and a variety of other demographic effects on suicide.
Editor’s Note: Why higher trace levels of lithium occurring naturally in the water supply should have this anti-suicide effect in the general population is unknown, but it is a fascinating finding. It also gives indirect credence to the clinical findings in patients with unipolar and bipolar disorder that lithium (albeit in the much higher levels achieved with medication) has anti-suicide effects.
Lithium Reduces Suicide Rate and Increases Longevity
 Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Editor’s Note: These data are consistent with a variety of other studies and raise the question why lithium is used less frequently in the US than in many European countries and Canada. Given its neuroprotective effects, its prevention of suicide and dementia, and its positive effects on longevity, it is hard to see why lithium is not included in the treatment regimens of more patients (at whatever dosage is well-tolerated), even if it alone is not sufficient for treating their manic and depressive episodes.
Research (by this editor Robert Post and colleagues) shows that bipolar disorder is a more pernicious illness in almost all respects in the US compared to the Netherlands and Germany (International Journal of Neuropsychopharmacology, 2011). Whether bipolar illness would be less severe in the US if it were more often treated with lithium is an unanswered question. The field cannot provide an answer with systematic prospective controlled data, as most study designs would be unethical (i.e. would deny useful treatment to suffering patients), although one large randomized comparative study called BALANCE did show the superiority of lithium over valproate. However, individual patients in consultation with their physician could evaluate the evidence and request that lithium be considered in their treatment regimen.
If a patient has some clinical predictors of a likely good response to lithium, the decision to include lithium should be a slam-dunk. Some of these include: a positive family history of mood disorder, especially bipolar disorder; a classic course with distinct episodes and clear periods of wellness; manic episodes that are euphoric as opposed to dysphoric (i.e. anxious/irritable); lack of an anxiety disorder or substance abuse comorbidity; the absence of mood-incongruent delusions; and a sequence of episodes of mania followed by a depression and then a well interval (MDI) rather than the sequence of DMI.
Exercise Helps Residual Depression
Many patients with depression require two or more treatments in order to achieve remission. In a 2011 study by Trivedi et al. published in the Journal of Clinical Psychiatry, patients with major depressive disorder who had not responded adequately to selective serotonin reuptake inhibitor (SSRI) antidepressants improved when an exercise regimen was added to their regular treatment.
The patients, aged 18-70 years old, were all sedentary at the start of the trial. They were randomized to one of two exercise regimens: a high dose regimen (16 kcal/kg per week, equivalent to walking at about 4 mph for 210 minutes per week) or the low dose (4 kcal/kg per week, equivalent to walking at 3 mph for about 75 minutes per week). Both groups improved significantly by the end of the study. Remission rates (adjusted for differences between groups) were 28.3% for the high dose group and 15.5% for the low dose group.
The rates of improvement with exercise were similar or better to those commonly seen with other augmenting agents such as lithium, T3, buspirone, and atypical antipsychotics, but without side effects and other inconveniences such as blood monitoring.
Other studies have indicated that exercise by itself and in combination with other treatments has efficacy in depression. Exercise can change serotonin and norepinephrine function and can increase brain-derived neurotrophic factor (BDNF), a, and neurogenesis in the hippocampus.
The researchers looked for moderating variables that may have affected the outcomes of various participants. Men, regardless of family history of mental illness, had better remission rates in the high dose group. Women without a family history of mental illness also improved more in the high dose group, while women with a family history of mental illness improved more in the low dose group, though this finding was statistically nonsignificant.
While the researchers observed that those in the high-dose group did exercise more than those in the low-dose group, participants in the high-dose group had more difficulty sticking to their exercise regimen. It may be that even though high doses of exercise offer slightly higher rates of remission, lower doses may be more effective clinically if patients can stick to the low-dose regimen better.
Good Weight Loss With Bupropion Plus Naltrexone
 A 2013 article by Smith et al. in the journal Diabetes, Obesity, and Metabolism reports that obese patients treated with the combination of bupropion (Wellbutrin) and naltrexone (Revia) had excellent weight loss and reduction in body fat compared to those treated with either drug alone or with placebo. The combination resulted in about a 14% reduction in body fat, while placebo, bupropion alone, and naltrexone alone each brought about only a 3-4% reduction.
A 2013 article by Smith et al. in the journal Diabetes, Obesity, and Metabolism reports that obese patients treated with the combination of bupropion (Wellbutrin) and naltrexone (Revia) had excellent weight loss and reduction in body fat compared to those treated with either drug alone or with placebo. The combination resulted in about a 14% reduction in body fat, while placebo, bupropion alone, and naltrexone alone each brought about only a 3-4% reduction.
Editor’s Note: Researcher Roger McIntyre is an expert on the metabolic syndrome in patients with bipolar illness and has been using this combination with success in patients with mood disorders. He finds the combination of bupropion and naltrexone more helpful than the anticonvulsants topiramate (Topomax) or zonisamide (Zonegran) or the anti-diabetes drug metformin.
Since obesity and the metabolic syndrome occur in approximately 40 to 50% of bipolar patients and significantly increases cardiovascular risks such as heart attack and stroke, and since bupropion is widely used in the treatment of bipolar depression, this combination appears worthy of consideration for those with obesity. Its use should be accompanied by a good diet and an exercise regimen. Decreasing cardiovascular risk is a very important component of the treatment of bipolar disorder, and the combination of bupropion and naltrexone could have substantial benefits.
Intermittent SSRI Treatment Helps PMS
Research has shown that serotonin-selective reuptake inhibitor (SSRI) antidepressants can be useful for severe premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD). According to a 2006 article by Steiner et al. in the Journal of Women’s Health, there are various ways that SSRIs can be used to treat PMS symptoms such as irritability, depressed mood, dysphoria, bloating, breast tenderness, appetite changes, and psychosocial function, including intermittent dosing just in the two weeks prior to PMS. Usually doses for PMS are lower than those used to treat depression.
For those with mood symptoms that continue throughout the month, continuous (daily) dosing may improve PMS symptoms. For those whose mood symptoms worsen during PMS, continuous dosing can be intermittently increased from around the time of ovulation to a few days after the period begins. For those women with mood symptoms only during PMS, intermittent dosing only during those weeks between ovulation and the period seems to be helpful and minimizes side effects of the SSRIs.
Editor’s Note: While SSRIs sometimes take weeks to reach maximum benefit for those with depression, intermittent dosing for women with severe PMS seems to be helpful. This may be because SSRIs acutely increase the neurosteroid allopregnanolone, which enhances GABA-A receptor activity, associated with improvement in mood and anxiety.





