Lithium May Slow or Prevent Dementia
Lithium inhibits the enzyme glycogen synthase kinase 3, which has been implicated in dementia. To study whether lithium may prevent cognitive decline, researchers led by Tobias Gerhard looked at the medication histories of patients with bipolar disorder who were 50 years of age or older. In their article published in the British Journal of Psychiatry, those patients who had taken lithium 301–365 days out of the previous year had substantially lower risk of dementia than those who had not taken lithium during that time. Patients who had 300 or fewer days of lithium use did not have a significant reduction in dementia risk, nor did patients who were prescribed anticonvulsant drugs.
Editor’s Note: These data are consistent with those of Lars Kessing and colleagues, which suggest that patients in Denmark who renewed their lithium prescriptions were less likely to receive a diagnosis of dementia in old age.
In 2011, Orestes V. Forlenza and colleagues also reported in the British Journal of Psychiatry that compared to placebo, a very small dose of lithium, 150 mg/day, slowed the progression of mild cognitive impairment over one year.
Long-Term Lithium Treatment Has Risks for Kidney Function, Even with Precautions
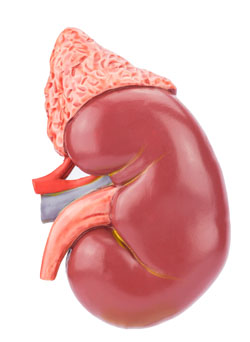 Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
The researchers, led by Harald Aiff, published the study in the Journal of Psychopharmacology in 2015. They identified 4,879 patients who had been prescribed lithium, and narrowed this list down to 630 adult patients who had taken lithium for at least 10 cumulative years, who had normal levels of creatinine when they began taking lithium, and on whom good data existed. About one-third of these patients had evidence of chronic renal impairment, and in 5% of these the impairment was severe or very severe.
Aiff and colleagues’ findings show that lithium treatment requires careful monitoring, especially over the long term. Patients must consider the risk/benefit ratio of lithium treatment. Since prevention of mood episodes can preserve an average ten years of life expectancy, and lithium has the best data for efficacy in preventing manic and depressive episodes, patients must weigh the risks of insufficiently treated bipolar illness against the possibility for long-term decreases in kidney function.
Vitamin B6 May Reduce Restless Legs in Patients Taking Antipsychotics
The atypical antipsychotic lurasidone (Latuda) is one of only a few drugs effective at treating bipolar depression. But 5–10% of patients who take lurasidone experience akathisia, or restless legs.
At a recent meeting, psychiatrist Cynthia Turner-Graham told this editor (Robert Post) of her success in treating a patient with lurasidone-related akathisia that had been resistant to all the standard treatments, including dose reduction, anticholinergic drugs, benzodiazepines, beta-blockers, etc. Vitamin B6 at a dose of 600mg twice a day gave the patient complete relief.
Dr. Turner-Graham was kind enough to direct me to a small double-blind study supporting this clinical observation in patients with schizophrenia who experienced akathisia from treatment with antipsychotics. The study by V. Lerner and colleagues was published in the Journal of Clinical Psychiatry in 2004.



