Three Experts’ Different Approaches to Treating PTSD in Veterans
 In the BNN we have previously described some experts’ preferred treatment algorithms for patients with treatment-resistant post-traumatic stress disorder (PTSD), which is often complicated by traumatic brain injury (TBI). In this article, we update and expand upon these expert views.
In the BNN we have previously described some experts’ preferred treatment algorithms for patients with treatment-resistant post-traumatic stress disorder (PTSD), which is often complicated by traumatic brain injury (TBI). In this article, we update and expand upon these expert views.
David Bakish has worked as Medical Director at the Ottawa Psychopharmacology Clinic and is a former professor of psychiatry at the University of Ottawa in Ottawa, Ontario. In addition, he works with the Canadian military seeing patients with PTSD, substance abuse, and traumatic brain injuries. He uses a symptom-driven approach to PTSD, including 6 to 7 targeted medications added in sequence.
Albert Sattin is a professor of psychiatry and biobehavioral sciences at UCLA, belongs to their Brain Research Institute, and is affiliated with both the Ronald Reagan UCLA Medical Center and the Veterans Affairs Greater Los Angeles Healthcare System. He prefers to treat PTSD with a three-part combination of the blood pressure–lowering drug prazosin, a selective serotonin reuptake inhibitor (SSRI) antidepressant, and the atypical antidepressant mirtazapine.
Murray Raskind pioneered placebo-controlled studies of prazosin for PTSD and served as director of the Veterans Affairs Puget Sound Health Care System Mental Health Service, in addition to serving in the Department of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine. Raskind’s approach to PTSD includes prazosin, the tricyclic antidepressant amitriptyline, and if needed for sleep, the sedative zolpidem.
Only SSRIs are approved by the US Food and Drug Administration (FDA) for the treatment of PTSD, but these on their own are rarely sufficient to handle the insomnia and other symptoms that accompany PTSD. Exposure therapy, in which patients are gradually led to approach trauma-related memories, feelings, and situations they previously avoided, is the most recommended type of therapy, but it too is often insufficient to treat all the complexities of the illness. Read on for more on each doctor’s approach to treating PTSD. Read more
Deep TMS May Improve Treatment-Resistant Bipolar Depression
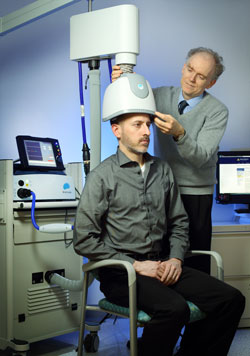 Deep transcranial magnetic stimulation (dTMS) is a non-invasive treatment that has been shown to be effective in unipolar depression. It consists of a helmet fitted to the head, which uses magnetic coils to create an electric field in a desired brain region.
Deep transcranial magnetic stimulation (dTMS) is a non-invasive treatment that has been shown to be effective in unipolar depression. It consists of a helmet fitted to the head, which uses magnetic coils to create an electric field in a desired brain region.
A 2017 double-blind randomized study by Diego F. Taveres and colleagues in the journal Neuropsychopharmacology found that 20 sessions of dTMS targeting the left dorsolateral prefrontal cortex produced greater improvement in bipolar depression over 4 weeks of treatment than the same number of sham sessions in which participants wore a helmet that delivered similar sounds and scalp sensations without the electrical effects to the brain. The participants had treatment-resistant bipolar depression that was being treated with medication.
However, dTMS’ effects were not significantly different from those of the sham over four additional weeks of follow-up, nor were remission rates significantly different across the two groups. Out of 50 participants, seven dropped out of the study—two from the sham group, and five from the active dTMS group. But there were no occasions on which a participant switched into mania following treatment.
This study suggests that dTMS has the potential to more rapidly improve treatment-resistant bipolar depression as well as unipolar depression.

