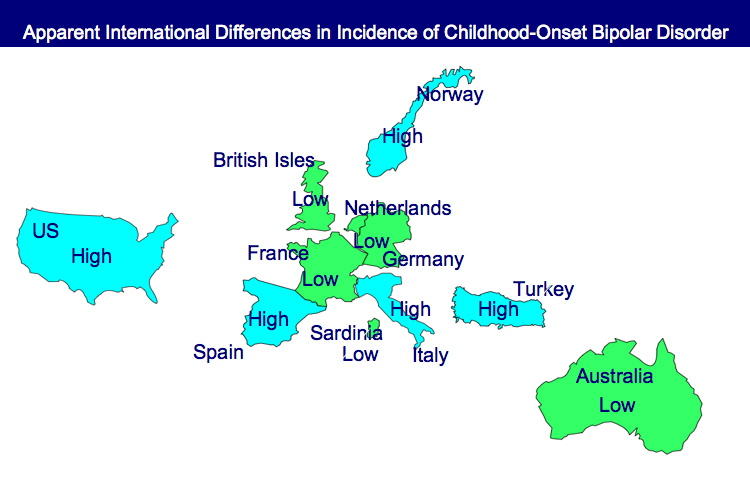
Incidence of Childhood Onset Bipolar Disorder Varies Geographically: More in US than Europe
A poster by Aditya Sharma of Newcastle University and colleagues at the Pediatric Bipolar Conference assessed the incidence of childhood-onset bipolar illness based on monthly letters sent to approximately 750 consultants in child and adolescent psychiatry in the British Isles. Only five confirmed cases were reported, with the youngest child being 11 years old.
EDITOR’S NOTE: These data are of particular interest in relationship to earlier data indicating that childhood-onset bipolar disorder may be relatively rare in some European countries, including the British Isles, France, the Netherlands, and Germany, as well as in Australia, South Korea, and New Zealand.
In contrast, childhood-onset bipolar illness with an onset prior to age 13 appears to be prevalent in the US, with one-fifth to one-quarter of adult outpatients reporting onsets of either depression with dysfunction or mania prior to age 13. Another substantial group of patients report onsets in adolescence, indicating that some 50-66% of bipolar illness in the US begins in either childhood or adolescence.
Similarly higher amounts of childhood-onset bipolar illness are reported in Italy, Turkey, and Norway, indicating some heterogeneity of vulnerability factors and course of illness outcomes among different European countries.
In the treatment network in which this editor is an investigator, we have found that this younger age of onset in the US is associated with more genetic/familial vulnerability and more experiential vulnerability in the form of more psychosocial adversity compared to that seen in the Netherlands and Germany. We published these results in the British Journal of Psychiatry in 2008 and will publish more detailed data in a paper that will be published soon in the International Journal of Clinical Psychopharmacology. These genetic, psychosocial, and early onset vulnerability factors are associated with a more adverse course of illness in the US compared with Germany and the Netherlands, in terms of increased comorbid anxiety disorder, substance abuse, experiencing more than 20 episodes prior to network entry, and experiencing rapid cycling in the year prior to network entry.
In addition, these individuals from the U.S. compared with the Netherlands and Germany did less well in naturalistic followup treatment, as rated by clinicians in the network. While early onset illness is a risk factor for poor outcome, we also found that the time delay to first treatment of mania and depression from the onset of illness was itself an independent risk factor for a poorer outcome in adults averaging age 42. This duration of lag to first treatment (which averaged 15 years in those with childhood onsets) was associated with prospective ratings of increased severity and duration of depression, fewer days euthymic, more episodes, and more days of ultradian cycling. This research will be published soon in the Journal of Clinical Psychiatry.
The origin and mechanisms of these transcontinental differences, with better outcomes in Europe than in the US, deserve further study and clarification, because they may reveal clinical and public health measures of therapeutic importance.
Comments
Leave a Reply