Children of Bipolar Parents in US More Ill than Those in the Netherlands
New research shows that bipolar disorder risk is higher in the US than in the Netherlands. At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researchers Manon Hillegers and Esther Mesman described a study in which they compared the offspring of mothers with bipolar disorder in the US to those in the Netherlands. The offspring ranged in age from 10–18.
In the US, the mothers had, on average, an earlier age of onset, more substance abuse comorbidity, and were more likely to have been diagnosed with bipolar II disorder. Among the US offspring, 66% had been diagnosed with a psychiatric illness compared to 44% of the Dutch offspring. This included significantly higher rates of anxiety, ADHD, and disruptive behavior disorders in the US offspring. Among the offspring who had been diagnosed with a mood disorder, 80% of those in the US had other additional psychiatric disorders, but only 34% of the Dutch did. Bipolar disorder is more rare among children under the age of 12 in the Netherlands compared to the US.
Dutch children and adolescents were typically treated with lithium and with only one drug at a time. In the US, lithium is less widely used, and simultaneous treatment with several medications (usually including atypical antipsychotics) is common.
Editor’s Note: The research by Hillegers and Mesman replicates research by this editor (Robert M. Post) and colleagues that compared bipolar disorder incidence and severity in the US, Germany, and the Netherlands. Other comparisons have been made between the US and Europe. A 2014 article by Frank Bellivier and colleagues in the World Journal of Biological Psychiatry also showed that bipolar disorder onset occurs earlier in the US than in 10 different European countries, while Bruno Etain and colleagues found that bipolar disorder onset occurs earlier in the US than in France in a 2012 article in the Journal of Clinical Psychiatry.
Together this research shows that bipolar disorder is more serious in the US than in a number of European countries. Two-thirds of adults with bipolar disorder report that their illness began in childhood or adolescence. Most of these cases are not properly diagnosed or treated. A concerted effort must be made by the medical establishment and healthcare policymakers in the US to provide better and earlier treatment of bipolar illness.
U.S. Patients with Bipolar Disorder Have More Stressors in Childhood and Prior to Illness Onset
In research published since 2008, our Editor-in-Chief Robert M. Post and colleagues in the Bipolar Collaborative Network have compared patients with bipolar disorder in the United States to those in Germany and the Netherlands. Compared to the European sample, patients in the US have more genetic vulnerability to bipolar disorder (by having a parent with bipolar disorder), earlier onsets of their illness, more complicated courses of illness, greater treatment resistance, and more medical comorbidities. Patients in the US also have more psychosocial stress.
The researchers are now turning their attention to these psychosocial vulnerabilities, and in a new paper that will be published in Psychiatry Research (late in 2013 or early in 2014), the authors show that patients in the US had more stressors both in childhood and just prior to the onset of their illness. Childhood stressors analyzed in the study were verbal abuse, physical abuse, and sexual abuse. Stressors in adulthood included indicators of a lack of social support, troubles with finances or employment, lack of access to health care, and medical comorbidities.
The stressors patients experienced just prior to their most recent episode of bipolar illness were related to: stressors in childhood, an earlier age of illness onset, anxiety and substance abuse comorbidity, lower income, both parents having an affective illness such as depression, and feeling more stigma.
The new research suggests that for patients with bipolar disorder in the US, adverse life events in childhood and later in life are more prevalent than they are for patients in the Netherlands or Germany. Earlier and more effective approaches to these stressors, such as the Family-Focused Therapy developed by David Miklowitz and Kiki Chang, could potentially slow the onset or progression of bipolar illness in this country.
Earlier Age of Onset of Bipolar Illness in the US Compared to Europe
 As we have previously reported in the BNN, the Bipolar Collaborative Network (including this editor Robert M. Post) found that patients from 4 sites in the United States had significantly earlier ages of onset of their bipolar illness compared to 3 sites in the Netherlands and Germany). These findings have been replicated by Frank Bellivier et al., who used a broader sample of European participants.
As we have previously reported in the BNN, the Bipolar Collaborative Network (including this editor Robert M. Post) found that patients from 4 sites in the United States had significantly earlier ages of onset of their bipolar illness compared to 3 sites in the Netherlands and Germany). These findings have been replicated by Frank Bellivier et al., who used a broader sample of European participants.
Bellivier’s research group studied two large samples of bipolar I patients from the US (n= 2275) and from 14 countries in Europe (n= 3616). The researchers found 3 different distributions of age of onset, and patients from the US had a greater representation in the early age of onset subgroup. Sixty-three percent of the sample from the US fell into the early-onset group versus 25% of those from Europe. The mean age of onset of the early-onset subgroup was significantly lower in the US sample (14.5 +/- 4.9 years) than in the European sample (19 +/- 2.7 years).
Editor’s Note: It is time that we took these geographical differences in the frequency of early age of onset of bipolar disorder seriously. While some controversy has surrounded the diagnosis of bipolar illness in children, it becomes increasingly important to recognize that this bona fide, well-diagnosed illness is more common in children from the US than from many other countries. Affected children should have careful clinical evaluation and, if the diagnosis warrants, definitive treatment. This should include both psychoeducational approaches; focused psychotherapies, including the family-focused therapy pioneered by Dave Miklowitz; and psychopharmacological intervention. When this kind of combined treatment is implemented, young patients who are treated with lithium, another mood stabilizer, or an atypical antipsychotic do much better than those who do not receive these consensus-based treatments.
Treatment algorithms for children of different ages with bipolar disorder are still being developed. However, it appears that in young and very young children, the atypical antipsychotics are often more effective than lithium or valproate monotherapy, as suggested in recent large randomized clinical trials. Initiating appropriate treatment is extremely important, since the duration of the untreated interval (that is, the time from illness onset to first treatment) is directly related to worse outcomes in adulthood. The longer the duration of untreated illness, the greater the severity of depression, the longer the duration of depression, and the greater the number of episodes an adult experiences.
As might be expected from the earlier age of onset of bipolar disorder, US patients also have a higher incidence of the major vulnerability factors for early onset—more genetic vulnerability (parents with bipolar disorder), more childhood stressors, and more stressors in the year prior to illness onset. Patients from the US also had a variety of other poor prognosis factors, including a higher degree of anxiety comorbidity, alcohol and substance abuse problems, a higher incidence of having more than 20 episodes over their lifetime, and a higher incidence of rapid cycling. All of these characteristics combine to produce worse outcomes in adult patients from the US compared to those from Europe. Earlier and more judicious treatment of the illness in the United States is needed to help ward off this more pernicious course of bipolar illness.
Early Life Stressors Linked to Persistent Inflammation and Endocrine Abnormalities
Epigenetics is a relatively new area of study that examines changes in DNA regulation and structure that can come about as a result of environmental events, as opposed to the genetic inheritance (DNA sequence) people receive through their parents’ genes. Epigenetic effects occur when an environmental stressor or chemical causes methyl or acetyl groups to attach to DNA or to histones (around which DNA are wound). These epigenetic changes determine how difficult it is to turn on genes coded in the DNA (see here for more information about the way the environment produces these epigenetic effects).
After the jump: Several studies presented at the 65th Annual Scientific Convention of the Society of Biological Psychiatry earlier this year suggested a link between environmental stress and both inflammation and abnormalities in DNA.
 Read more
Read more
Incidence of Childhood Onset Bipolar Disorder Varies Geographically: More in US than Europe
A poster by Aditya Sharma of Newcastle University and colleagues at the Pediatric Bipolar Conference assessed the incidence of childhood-onset bipolar illness based on monthly letters sent to approximately 750 consultants in child and adolescent psychiatry in the British Isles. Only five confirmed cases were reported, with the youngest child being 11 years old.
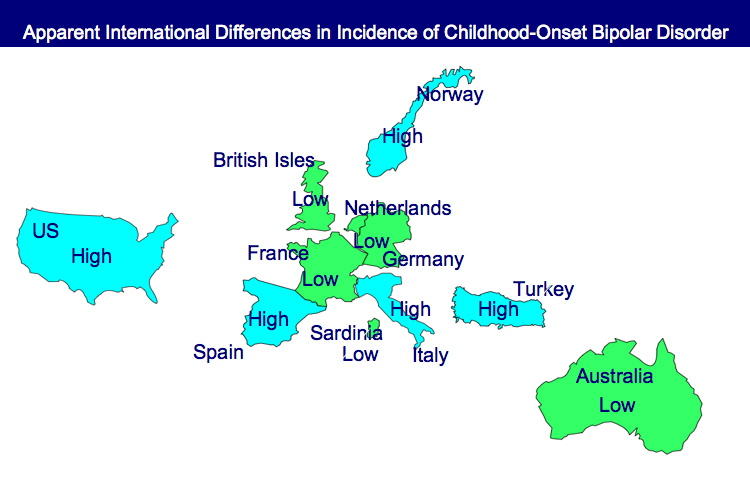
EDITOR’S NOTE: These data are of particular interest in relationship to earlier data indicating that childhood-onset bipolar disorder may be relatively rare in some European countries, including the British Isles, France, the Netherlands, and Germany, as well as in Australia, South Korea, and New Zealand.
In contrast, childhood-onset bipolar illness with an onset prior to age 13 appears to be prevalent in the US, with one-fifth to one-quarter of adult outpatients reporting onsets of either depression with dysfunction or mania prior to age 13. Another substantial group of patients report onsets in adolescence, indicating that some 50-66% of bipolar illness in the US begins in either childhood or adolescence.
Similarly higher amounts of childhood-onset bipolar illness are reported in Italy, Turkey, and Norway, indicating some heterogeneity of vulnerability factors and course of illness outcomes among different European countries.
Awareness of metabolic concerns in patients with bipolar disorder: A survey of European psychiatrists
Michael Bauer, Yves Lecrubier, Trisha Suppes
From the Department of Psychiatry and Psychotherapy, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany; Hôpital de la Salpêtrière, Paris, France; and Bipolar Research Program, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX
Objective: An online survey of European psychiatrists assessed awareness of the metabolic syndrome and its influence on the management of bipolar disorder.