Diabetes Complicates Bipolar Disorder
People with bipolar disorder are three times more likely than the general population to develop type 2 diabetes. Type 2 diabetes typically occurs in adulthood and is associated with insulin resistance, as opposed to type 1, which is usually diagnosed in childhood and is associated with insulin deficiency.
In a talk at the 2015 meeting of the Society of Biological Psychiatry, researcher Tomas Hajek reported that in a large group of bipolar patients, 13% reported a history of type 2 diabetes, 21% were diagnosed with type 2 diabetes upon laboratory evaluation, and 32.2% had pre-diabetes without realizing it. Thus, about half of these patients with bipolar disorder were either affected by diabetes or at risk for it, many without knowing it.
The Bad News
Diabetes complicates the course of bipolar illness. Type 2 diabetes is associated with poorer response to treatment, atrophy of the hippocampus, cognitive impairment, and higher rates of conversion from mild cognitive impairment to full-blown dementia.
The main effect of type 2 diabetes is insulin resistance. The body produces enough insulin, but insulin’s effects at its receptors are impaired. Diabetes also causes deficits in growth factors, increases in the enzyme GSK3B, decreases in mitochondria and brain-derived neurotrophic factor (BDNF, which protects neurons), and glucose toxicity.
Recent research by Hajek and colleagues shows that diabetes has several other detrimental effects on the brain in bipolar disorder. On magnetic resonance spectroscopy (MRS) scans, people with type 2 diabetes had lower levels of NAA, a marker of neuronal integrity, in the prefrontal cortex. This can indicate impaired functioning. People with type 2 diabetes also had lower levels of creatine, indicating impaired energy metabolism. In addition, hippocampal volume decreases with aging, and type 2 diabetes accelerated this age-related decline.
Some of diabetes’ effects on the brain are mediated by other health factors, including obesity, cerebral blood vessel disease (which affects white matter integrity), and side effects from medications.
What You Can Do
Start early with a good diet and exercise, and have regular checkups with a doctor, who can tell you if you have diabetes or are at risk for it. If so, start long-term preventative treatment with the most effective and easy-to-tolerate medications, and periodically have your fasting blood sugar tested. If these tests are abnormal, have your hemoglobin A1c (HbA1c) checked. This is a measure of good glucose control, and should be under 6. If it creeps upward toward 6 (a sign of pre-diabetes), the drug metformin may be able to prevent the onset of type 2 diabetes. If you have type 2 diabetes, there are several types of effective medications that can minimize its effects.
Studies of Medications and RTMS in Children Lacking
At the 2015 meeting of the Transcranial Magnetic Stimulation Society in May, researcher Stephanie Ameis discussed the dearth of medication studies in children, particularly for depression but also for schizophrenia and autism spectrum disorders, which share the symptom of impaired executive functioning, which can include skills such as planning and problem solving.
Ameis noted that in a literature review, there were a total of 1046 controlled pharmacological treatment studies in adults compared to only 106 in children, which reflects a relative absence of treatment knowledge, especially for depression (where there were 303 studies in adults versus only 17 in children) and bipolar disorder (where there were 174 studies of adults and 24 of children).
Ameis then reviewed the few studies of rTMS for depression in young people. She identified several series with only a total of 33 children and adolescents who had been treated with rTMS. She is beginning to study rTMS in patients with high-functioning autism (40 patients aged 16 to 25 have been randomized in her study). Ameis also described a 2013 study of rTMS in which patients with schizophrenia showed improved performance on a test of working memory published by Mera S. Barr and colleagues in the journal Biological Psychiatry. Ameis cited this as a rationale for studying rTMS’s effect on cognitive performance in people with autism.
Verbal Abuse in Childhood, Like Physical and Sexual Abuse, Linked to Earlier Onset and More Difficult Course of Bipolar Disorder
Earlier research has shown that childhood adversity is linked to earlier age of onset of bipolar disorder and more difficult course of illness. Physical and sexual abuse are associated with both earlier age of onset and more difficulties such as anxiety disorders and substance abuse. Now, new research by this editor (Robert M. Post) and colleagues links verbal abuse (even in the absence of physical and sexual abuse) to earlier onset of bipolar disorder and to more severe and complicated course of illness.
The study, published in the journal Bipolar Disorders, was based on the self-reports of 634 adult outpatients with bipolar disorder at four sites in the US. These participants were interviewed about their history of illness and the frequency of adverse events they experienced in childhood, adolescence, and adulthood, including physical, sexual, and verbal abuse. Twenty-four percent of these participants reported having experienced verbal abuse occasionally or frequently in childhood, but not other forms of abuse, while another 35% had a history of verbal abuse as well as physical or sexual abuse, for a total of 59% with a history of verbal abuse.
The greater the frequency of verbal abuse in childhood, the earlier the average age of onset of bipolar disorder. Participants with no history of abuse had a mean age of onset of 20.6 years, but verbal abuse by itself reduced the mean age of onset to 16.5 years, and verbal abuse plus sexual abuse reduced the mean age of onset to 15.3 years. (The mean age of onset for participants who experienced sexual abuse alone was 17.5 years.) It was impossible to determine the combined effect of verbal and physical abuse because verbal abuse was almost always present when physical abuse occurred. For the 14% of the participants who had experienced verbal, physical, and sexual abuse in childhood, the mean age of onset of bipolar disorder was 13.1 years.
Those who were verbally (but not physically or sexually) abused in childhood had more anxiety disorders, drug abuse, and rapid cycling than those who were not abused, but not more alcohol abuse. Those who were verbally abused also showed increasing severity of illness, including increased frequency of cycling.
Genetics can also play a role. Having a parent with a mood disorder also contributed to an earlier age of onset of bipolar disorder.
Editor’s Note: Researcher David J. Miklowitz and colleagues have shown that family focused therapy (FFT), which emphasizes illness education and communication enhancement within the family, is more effective than treatment as usual for children with a family history of bipolar disorder and a diagnosis of depression, cyclothymia, or bipolar not otherwise specified (BP NOS).
FFT was particularly effective in reducing symptoms in children from families with high expressed emotion, suggesting that this kind of family-based intervention could reduce levels of verbal abuse.
Solutions for Clozapine-Induced Drooling
Clozapine is a treatment for schizophrenia and treatment-resistant bipolar disorder. Drooling is a side effect for about one-third of people taking clozapine. Here are some treatments that may help reduce it:
1) Botox injected into each salivary (parotid) gland in doses of 50 IU.
2) Ipratropium, either sprayed under the tongue or intranasally. A 2004 case series by Oliver Freudenreich in the Journal of Clinical Psychiatry described sublingual administration.
3) Glycopyrrolate. In a 2011 article in the Annals of Pharmacotherapy, AM Bird described some treatments for clozapine-induced drooling, including glycopyrrolate.
4) The blood pressure drugs clonidine (50–100 mg) or terazosin.
4) Transdermal scopolamine patch. This is typically placed behind the ear to reduce motion sickness, but it also reduces saliva production.
Long-Term Lithium Treatment Has Risks for Kidney Function, Even with Precautions
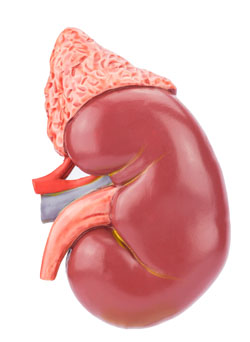 Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
The researchers, led by Harald Aiff, published the study in the Journal of Psychopharmacology in 2015. They identified 4,879 patients who had been prescribed lithium, and narrowed this list down to 630 adult patients who had taken lithium for at least 10 cumulative years, who had normal levels of creatinine when they began taking lithium, and on whom good data existed. About one-third of these patients had evidence of chronic renal impairment, and in 5% of these the impairment was severe or very severe.
Aiff and colleagues’ findings show that lithium treatment requires careful monitoring, especially over the long term. Patients must consider the risk/benefit ratio of lithium treatment. Since prevention of mood episodes can preserve an average ten years of life expectancy, and lithium has the best data for efficacy in preventing manic and depressive episodes, patients must weigh the risks of insufficiently treated bipolar illness against the possibility for long-term decreases in kidney function.
Bipolar Disorder Is Often Overlooked in Primary Care
A 2014 study by Joseph M. Cerimele and colleagues in the journal Psychiatric Services found that primary care patients with bipolar disorder had severe depression and anxiety, symptoms of other psychiatric illnesses, and psychosocial problems such as housing difficulties, homelessness, or lack of support. Only 26% were referred to specialty mental health care despite the severity of these problems. These findings suggest the primary care setting, where many patients obtain their care, provides insufficient support for people with bipolar disorder.
Editor’s Note: There are several way to overcome the deficient recognition and treatment of bipolar disorder in primary care:
Record mood fluctuations
It is critical that patients keep a detailed longitudinal record of mood fluctuations in order to enhance the likelihood that their doctor can perform a well-informed evaluation and assessment of the effects of treatment. Several ways of doing this are available. We offer a variety of printable daily mood charts available on our website. Another option is What’s My M3, a free app that can be downloaded from the Itunes Store or Google Play. In a three-minute survey, it screens for depression, anxiety, OCD, PTSD, and mania. The ratings can be done longitudinally and printed out to assist a physician in the evaluation, assessment of course of symptoms, and response to treatment.
Parents of children aged 2–12 with mood or behavioral problems (or at risk for them because they have a parent with a diagnosis of depression or bipolar disorder) can rate their children each week as part of a new study. These ratings, which will help determine how children with symptoms of mental illness are being treated in the community, are done via a secure website and can be printed out to help a treating physician or other clinician to evaluate the children’s course of illness and responses to treatments. Access to informed consent documents and more information about participation in the study, known as the Child Network, is available here.
Learn about mood disorders
Patients should educate themselves about the signs and symptoms of mood disorders. Many books on this topic are available, and the BNN newsletter tries to update patients and clinicians about the latest findings about the treatment of depression and bipolar disorder.
Get extra help
Patients can seek out consultations with experts in bipolar disorder, who may be able to provide extra guidance to help primary care physicians arrive at the appropriate diagnosis or find an optimal treatment plan and back up approaches if the initial options do not bring about remission.
Finding a psychotherapist who can provide psychoeducation about bipolar disorder and cognitive behavioral or other specialized therapies may also be of great use, as more than a dozen randomized studies document the effectiveness of psychoeducation and/or psychotherapy compared to treatment as usual.
Talk about mood at every medical evaluation
Many medical problems such as heart disease and diabetes require careful monitoring, with patients as active participants. Likewise, careful monitoring of mood is a critical component of good treatment and should yield positive short-term and long-term results in recurrent depression and bipolar disorder.
Since depression can complicate many medical illnesses, patients should get in the habit of asking physicians not only about their blood sugar, blood pressure, or cholesterol, but also, “What about my low mood, anxiety, or insomnia?” It may be just the spark a physician needs to better attend to these equally important health issues.
Subthreshold Episodes of Mania Best Predictor of Bipolar Disorder in Children
Relatively little attention has been paid to the children of a parent with bipolar disorder, who are at risk not only for the onset of bipolar disorder, but also anxiety, depression, and multiple other disorders. These children deserve a special focus, as on average 74.2% will receive a major (Axis 1) psychiatric diagnosis within seven years.
New research published by David Axelson and colleagues in the American Journal of Psychiatry describes a longitudinal study comparing children who have a parent with bipolar disorder to demographically matched children in the general public. Offspring at high risk for bipolar disorder because they have a parent with the disorder had significantly higher rates of subthreshold mania or hypomania (13.3% versus 1.2%) or what is known as bipolar disorder not otherwise specified (BP-NOS); manic, mixed, or hypomanic episodes (9.2% versus 0.8%); major depressive episodes (32.0% versus 14.9%); and anxiety disorders (39.9% versus 21.8%) than offspring of parents without bipolar disorder. Subthreshold episodes of mania or hypomania (those that resemble but do not meet the full requirements for bipolar disorder in terms of duration) were the best predictor of later manic episodes. This finding was observed prospectively, meaning that patients who were diagnosed with manic episodes during a follow-up assessment were likely to have been diagnosed with a subthreshold manic or hypomanic episode during a previous assessment.
The study included 391 children (aged 6–18) of at least one bipolar parent, and compared these to 248 children of parents without bipolar disorder in the community. The participants took part in follow-up assessments every 2.5 years on average, for a total of about 6.8 years. Each follow-up assessment included retrospective analysis of symptoms that had occurred since the previous assessment.
In addition to having more subthreshold manic or hypomanic episodes; manic, mixed, or hypomanic episodes; and major depressive episodes, the high-risk children also showed more non-mood-related axis 1 disorders, including attention deficit hyperactivity disorder (ADHD), disruptive behavior disorders, and anxiety disorders than the children of parents without bipolar disorder. Axelson suggested that monitoring for these symptoms may help with early identification and treatment.
Children with a bipolar parent were diagnosed with bipolar spectrum disorders at rates of 23% compared to 3.2% in the comparison offspring. Mean age of onset of mania or hypomania in the high-risk offspring was 13.4 years. Of those offspring who had a manic episode, more than half had the episode before age 12, with the earliest occurring at age 8.1.
Compared to previous studies of children of parents with bipolar disorder, this study found that the mean age of onset of manic or hypomanic episodes was younger, possibly because other studies did not include young children. Another new finding was that major depressive episodes were risk factors for mania and hypomania but did not always precede the onset of mania or hypomania in the high-risk offspring.
Parents of children who are at high risk for developing bipolar spectrum disorders should be aware of the common precursors to mania—subthreshold manic or hypomanic symptoms and non-mood disorders—and make sure that clinicians assess for these symptoms and differentiate them from the symptoms of depression or other disorders.
Editor’s Note: In Axelson’s study, 74.2% of the offspring of a bipolar parent suffered a major (Axis I) psychiatric disorder. However, 48.4% of the offspring from the comparison group of community controls also had an Axis 1 psychiatric disorder. These high rates of illness and dysfunction indicate the importance of monitoring a variety of symptom areas and getting appropriate evaluation and treatment in the face of symptoms that are associated with impairment in both high risk children and in the general population.
One way of doing this is for parents to join our new Child Network, a study collecting information about how children at risk for bipolar disorder or with symptoms of bipolar disorder are being treated in the community and how well they are doing. Parents rate their children on a weekly basis for depression, anxiety, ADHD, oppositionality, and mania-like symptoms. Parents will be able to produce a longitudinal chart of their children’s symptoms and response to treatment, which may assist their child’s physician with early detection of illness and with treatment. See here for more information and to access informed consent documents.
Recovery and Relapse After a First Mania
The timeframe during which recovery and recurrence occur in people with a first episode of mania are somewhat variable. A meta-analysis by Andréanne Gignac and colleagues published in the Journal of Clinical Psychiatry in 2015 offers some new information. The meta-analysis included eight studies with a total of 734 participants in a first episode of mania. Syndromal recovery rates (when patients no longer met diagnostic criteria for bipolar disorder) were 77.4% at six months after first episode of mania and 84.2% at one year after. However, some symptoms lingered, and only 62.1% of patients reached a period of symptomatic recovery within one year.
Recurrence rates were 25.7% within six months, 41.0% within one year, and 59.7% by four years. Those who were younger at the time of the first episode were at higher risk for relapse within one year.
Editor’s Note: On the positive side, most recovered, but on the negative side, at one year, 60% remained symptomatic and 40% had a recurrence. What is not clear is how intensively patients were treated and monitored. The main message of this study is that a first episode of mania is not trivial and deservces concerted acute and long-term treatment. When expert multimodal treatment is given results are vastly more superior than treatment as usual (Kessing et al. British Journal of Psychiatry 2013).
Meta-Analysis Shows Effectiveness of Ketamine for Bipolar and Unipolar Depression
Ketamine, an anesthetic sometimes used intravenously in the treatment of depression, can bring about rapid onset of antidepressant effects. A new meta-analysis by researcher Michael Bloch and colleagues presented at a recent conference showed that ketamine’s maximum antidepressant effects occur within one day of administration, and its effects remain significant (compared to control conditions) one week following infusion. Ketamine’s effects were diminished in patients taking other medications. There was a trend for better response in patients with bipolar disorder than with unipolar disorder.
Bloch and colleagues analyzed eight earlier studies including a total of 180 participants. In each study, ketamine had been compared to a control condition, either an infusion of saline solution or of midazolam, which mimics ketamine’s sensory effects but does not have antidepressant effects. The researchers are calling for more meta-analyses of ketamine studies to determine which patients respond best to ketamine and how to sustain ketamine’s effects.
Editor’s Note: In another poster presented at the same conference, James Murrough reported that patients with slower processing speed responded best to ketamine. Other findings have shown that those with a history of alcohol abuse and a common genetic variant of brain-derived neurotrophic factor (BDNF), the val-66-val allele of proBDNF, are more likely to respond to ketamine.
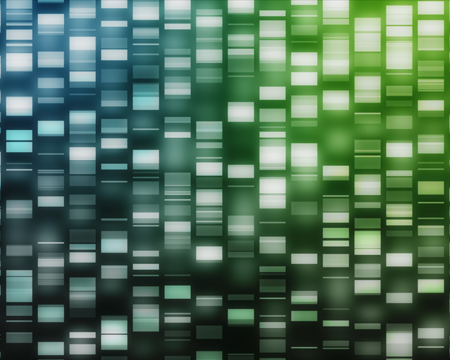
Gene CACNA1C is Associated with Early-Onset Bipolar Disorder
Several genes have previously been implicated in bipolar illness. In a recent study, researchers at the Mayo Clinic, led by Paul Croarkin, compared variations in three genes (CACNA1C, ANK3, and ODZN) across 69 children aged 6–15 with mania, a 776-person control group from the Mayo Biobank database, and 732 adults with bipolar disorder (some with onset in childhood and adolescence and some with onset in adulthood, also from the Biobank). All participants were Caucasian, to minimize confounding by population stratification. The researchers found that the minor allele of rs10848632 in CACNA1C was associated with childhood onset of bipolar disorder. The haplotype (or sequence of nucleotides) T-G-G-T was the one associated with risk. Genetic risk scores were also associated with early onset of illness.
Editor’s Note: In research by Michael McCarthy and colleagues, CACNA1C has been linked to abnormal circadian rhythms in bipolar disorder and to responsiveness to lithium treatment. Together, these data suggest the importance of studying the calcium channel blocker nimodipine (which blocks calcium influx through CACNA1C) in childhood-onset bipolar disorder. A 1999 case report by Pablo A. Davanzo and colleagues described a teenager with ultra rapid cycling bipolar disorder (multiple mood switches/day) that did not respond to a host of conventional medications, who improved dramatically on nimodipine, reaching remission. This author (Robert M. Post) has also seen confirmed responsivity in adults with rapid cycling bipolar disorder (reported in the 2008 book Treatment of Bipolar Illness: A Casebook for Clinicians and Patients, by Post and Gabriele S. Leverich).