How Stress Triggers Inflammation and Depression
 Depression and bipolar disorder are associated with increases in markers of inflammation that can be found in the brain and blood. It is increasingly clear that the mechanisms that cause depression are not just in the brain, but actually throughout the body. These include two signaling systems that begin in the bone marrow and the spleen.
Depression and bipolar disorder are associated with increases in markers of inflammation that can be found in the brain and blood. It is increasingly clear that the mechanisms that cause depression are not just in the brain, but actually throughout the body. These include two signaling systems that begin in the bone marrow and the spleen.
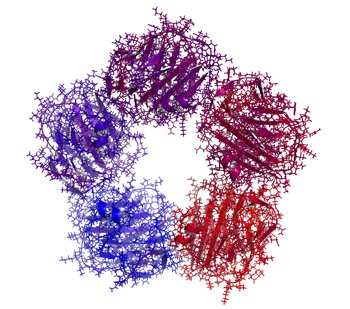
When a small mouse is repeated defeated by a larger animal, they show depression-like symptoms known as defeat stress. Animal studies have shown that stress and danger signals are perceived and relayed to the amygdala and the hypothalamus. The sympathetic nervous system releases the neurotransmitter norepinephrine into bone marrow, where stem cells are turned into activated monocytes (a type of white blood cells) that are then released into the blood. The monocytes travel to the brain, leading to the activation of more inflammatory cells.
Blocking part of this process can prevent the depression-like behaviors from occurring. If the bone marrow monocytes are blocked from entering the brain, inflammation and defeat stress behaviors like social avoidance do not occur. However, if there is a second bout of defeat stress, primed monocytes that have been stored in the spleen are released and travel to the brain, producing further increases in inflammatory cells and even more defeat stress behaviors.
If these monocytes from the spleen are blocked, the inflammation and the reaction to the new stressor do not occur.
Stress also activates lymphocytes (another type of white blood cells) to secrete the inflammatory cells Il-6. If this Il-6 secretion is inhibited, defeat stress behaviors can be prevented.
Defeat stress also leads to the release of the neurotransmitter glutamate. Some of this cascade begins in the brain, which evaluates stressors and releases IL-1 beta, another type of inflammatory cell. It slows down the production of glutamate, while IL-6 can endanger neurons and is associated with anhedonia—loss of interest in pleasurable activities. This cascade also leads to the production of another type of inflammatory cell, TNF-alpha, which has adverse effects on biochemistry, brain, and behavior.
This understanding of the role of the brain and body provides new targets for drug development. If inflammatory processes are blocked, defeat stress behaviors do not occur. Researcher Michael D. Weber and colleagues described this process in detail in the journal Neuropsychopharmacology Reviews in 2017.
Together these observations suggest that inflammatory processes in the body are crucial to the development of some stress- and inflammation-related depressive behaviors.
Measuring Inflammation in Neuropsychiatric Disorders May Shed Light on Treatment
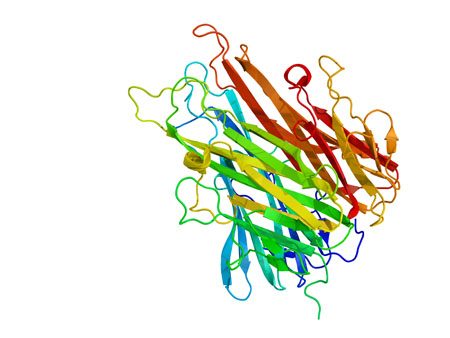
Meta-analyses have found links between elevated levels of inflammatory markers and many neuropsychiatric disorders, including depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and traumatic brain injury. Multiple studies also show that those with elevated inflammatory markers such as interleukin-1, interleukin-6, tumor necrosis factor (TNF) alpha, and c-reactive protein (CRP) also respond less well to typical treatments than those with normal levels of these markers in the blood.
These links suggest that it could be useful to measure levels of these inflammatory markers in the blood of people who are responding poorly to medications. If one or more of these markers are elevated, it might be a sign that treatment with an anti-inflammatory agent could be helpful. Preliminary studies have shown that some neuropsychiatric disorders may improve after treatment with anti-inflammatory drugs such as aspirin, celecoxib (Celebrex), and the antibiotic minocycline, among others.
Inflammatory Marker CRP Higher in Bipolar Disorder, Particularly Mania
Inflammation has been linked to mood disorders. A 2016 meta-analysis in the journal Lancet Psychiatry described the role of inflammatory marker C-reactive protein (CRP) in bipolar episodes. Researchers led by Brisa S. Fernandes identified 27 studies that measured CRP levels in a total of 2,161 patients with bipolar disorder and 81,932 healthy participants. The researchers determined that compared to healthy controls, people with bipolar disorder have higher levels of CRP. CRP levels were moderately elevated between episodes and during depression, and substantially elevated during episodes of mania.
Editor’s Note: This meta-analysis shows that CRP is linked to bipolar disorder, and the inflammatory burden is highest during mania. It remains to be seen whether anti-inflammatory treatments work best in patients with high CRP levels compared to normal CRP levels.
CRP is also a risk factor for cardiovascular disease, and lithium and other treatments for bipolar disorder probably lower CRP levels.
The same group of researchers previously showed that statins, drugs typically used to lower cholesterol, could help alleviate depression. Since statins have anti-inflammatory effects, they can probably reduce depression risk in addition to lowering cardiovascular risk, as initial studies suggest.
Other drugs with anti-inflammatory effects that may improve depression include the anti-arthritis drug celecoxib and the antibiotic minocycline. The amino acid N-acetylcysteine and omega-3 fatty acids also have anti-inflammatory effects and have been found to improve depression in some studies.
Anti-Inflammatory Treatments Improve Depression
Inflammation can interfere with the balance of neurotransmitters in the brain, making antidepressants less effective. Anti-inflammatory treatments (such as those used to treat rheumatoid arthritis) may help. In a 2016 meta-analysis published in the journal Molecular Psychiatry, researchers led by Nils Kappelmann analyzed the results of 20 clinical trials of chronic inflammatory conditions where depressive symptoms were also recorded. In a subset of 7 clinical trials that compared anti-inflammatory treatment to placebo, they found that anti-inflammatory treatment improved depressive symptoms significantly compared to placebo.
The anti-inflammatory drugs studied most often targeted the inflammatory marker tumor necrosis factor (TNF) alpha using an antibody. Some of the anti-inflammatory drugs that improved depressive symptoms were adalimumab, etanercept, infliximab, and tocilizumab.
The researchers also found that those participants with the most inflammation when they began treatment saw the largest improvement in their depression after taking anti-inflammatory treatments.
Kappelmann and colleagues suggest that inflammation may cause depression, and that anti-inflammatory drugs may be useful in the treatment of depression in people with high inflammation.
Inflammation Predicts Depression and Anxiety Four Years Later in Older Americans
A large study of retired Americans found that those with high levels of the inflammatory marker C-reactive protein in the blood had more depression and anxiety. Higher CRP also predicted severity of depression and anxiety four years later.
The study, by researchers Joy E. Lin and Aoife O’Donovan, included 18,603 people over age 50 from the Health and Retirement Study. It was presented at the 2016 meeting of the Society of Biological Psychiatry.
Lin and O’Donovan hope that treating or preventing inflammation may be the key to preventing symptoms of depression and anxiety.
Psychotherapy Improved Depression, Reduced Inflammation
A recent study shows that psychotherapy can not only improve depression symptoms, but may also reduce the inflammation that often accompanies them.
Researcher Jean Pierre Oses and colleagues randomly assigned participants with depression to receive Supportive-Expressive psychodynamic therapy, which is designed to help patients understand conflictual relationship patterns, or an alternative therapy. Among the 47 participants who received Supportive-Expressive therapy, depression improved significantly after 16 sessions, and blood levels of the inflammatory markers interleukin-6 and TNF alpha also dropped.
The research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Meta-Analysis Shows Inflammation is Common in Unipolar Depression, Bipolar Depression, and Schizophrenia
In a symposium at the 2016 meeting of the Society of Biological Psychiatry, Mark Hyman Rapaport described the results of his research group’s meta-analysis of studies comparing levels of inflammation in the blood of people with unipolar depression, bipolar depression, and schizophrenia. Rapaport and colleagues determined that people acutely ill with any of the three illnesses showed abnormally high levels of certain inflammatory proteins. These included: interleukin-1beta, interleukin-6, TNF alpha, and c-reactive protein. Those who were chronically ill showed elevations in interleukin-6.
These data are consistent with increasing evidence that inflammation also occurs in the brain. Brain inflammation can be observed by measuring translocator protein binding, a measure of brain microglial activation, using positron emission tomography (PET) scans.
Teens with Bipolar Disorder Have More Inflammation, Cardiovascular Risks
 Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Hatch and colleagues assessed the blood of 60 teens with bipolar I or II disorder and 20 healthy controls for a variety of biomarkers, including the inflammatory proteins interleukin 6, interleukin 10, and TNF alpha; VEGF, which is responsible for the production of new blood vessels; and brain-derived neurotrophic factor (BDNF), which protects neurons. The researchers also assessed the participants’ cardiovascular health, performing the carotid intima media thickness test to estimate how much plaque is in the arteries, and measuring how well the patients’ arteries dilate in response to changes in bloodflow.
Participants with bipolar disorder had higher levels of interleukin 6 than healthy controls, regardless of whether their bipolar illness was symptomatic. Low BDNF was linked to greater carotid intima thickness in participants with symptomatic bipolar disorder, and vascular measurements suggest a possible mechanism by which bipolar disorder increases cardiovascular risk.
Brain Inflammation Found in Autopsy Studies of Teen and Adult Suicides
Suicide and depression have both been linked to elevated levels of inflammatory cytokines in the blood and cerebrospinal fluid. A recent study finds that these inflammatory markers are also elevated in the brains of teens and depressed adults who died from suicide.
In autopsy studies, researcher Ghanshyam N. Pandey measured levels of the inflammatory cytokines interleukin-1beta, interleukin 6, and TNF-alpha in the brains of teen suicide victims, and compared these to the brains of teens who died from other causes. Pandey also measured levels of interleukin-1beta, interleukin 6, interleukin 8, interleukin 10, interleukin 13, and TNF-alpha in the prefrontal cortex of depressed adult suicide victims and compared them to levels in adults who died of other causes.
There were abnormalities in the inflammatory markers in the brains of those who died from suicide compared to their matched controls. The suicide victims had higher levels of interleukin-1beta, interleukin 6, and TNF-alpha than the controls. Among the adults, levels of the anti-inflammatory cytokine interleukin 10 were low in the suicide victims while levels of Toll-like receptors (TLR3 and TLR4), which are involved in immune mechanisms, were high.
Brain inflammation has also been observed in positron emission tomography (PET) scans of depressed patients, where signs of microglial activation can be observed. Elevated inflammatory cytokines are also found in the blood of some people with bipolar disorder, depression, and schizophrenia.
Pandey presented this research at the 2016 meeting of the Society of Biological Psychiatry.
IL-6 in Blood and Bone Marrow Linked to Lack of Resilience to Stress
Rodents who are repeatedly defeated by larger animals often exhibit depression-like behaviors. In new research that researcher Georgia E. Hodes presented at the 2016 meeting of the Society of Biological Psychiatry, animals who are susceptible to these social defeat stress behaviors showed immune irregularities, including high levels of the inflammatory marker interleukin-6.
An intervention to prevent the mice from secreting interleukin-6 in blood and bone marrow took away their susceptibility to social defeat stress. When bone marrow from rodents with no interleukin-6 was transplanted into susceptible mice, the recipients showed resilience to social defeat stress. Conversely, a transplant from susceptible mice to those mice without IL-6 led to social defeat stress in the previously “immune” mice.
This research shows that the peripheral immune system, including blood and bone marrow, plays an important role in depression-like behaviors in mice.