Transgenerational Transmission of PTSD
At a recent scientific meeting, Rachael Yehada showed that PTSD-like traits could be passed transgenerationally. Mothers in New York City who were pregnant on September 11, 2001 and developed post-traumatic stress disorder (PTSD) produced children with low cortisol in their blood (a sign of PTSD). If the fathers had PTSD during the mother’s pregnancy, the children had high cortisol.
These gender-related findings have some parallels in studies of rodents. When a rat pup is separated from its mother for 15 minutes, the mother is overjoyed to see the pup return and licks and grooms it excessively. This maternal overprotection yields an animal with lifelong low cortisol through an epigenetic process. The glucocorticoid receptor gives a feedback message to suppress cortisol, and glucocorticoid receptors are increased in the pups’ brains because of lower methylation of the DNA promoter for glucocorticoid receptors.
If a father has PTSD, there is more methylation of the promoter for glucocorticoid receptors and less expression of them in the forebrain. There is also less feedback suppression of cortisol and the baby exhibits high cortisol.
The methylation of the glucocorticoid receptors in the offspring’s white blood cells is highly correlated (r=0.57, p<0.005, n=23) with methylation in the parent’s white blood cells.
IV Ketamine Superior to IV Midazolam in Adults with PTSD
In a recent study, ketamine performed better than an active comparator on several measures in adults with post-traumatic stress disorder (PTSD). Since ketamine has noticeable dissociative effects, researchers have looked for another drug with mind-altering effects that would be a more appropriate comparator than placebo.
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, Adriana Feder of Mount Sinai Hospital reported on the randomized study in those with PTSD, in which intravenous ketamine was compared to intravenous midazolam, a potent benzodiazepine that produces anti-anxiety and sedating effects. Murrough et al. previously showed that intravenous ketamine was superior to midazolam in treatment-resistant depression.
In the randomized study Feder described, the participants had suffered PTSD from a physical or sexual assault and had been ill for 12 to 14 years. Those who received ketamine improved more, in some instances for as long as two weeks (ketamine’s blood levels disappear after a few hours, and its clinical antidepressant effects usually last only a few days). Reports of side effects included three patients with blood pressure increases requiring treatment with propranolol, and four patients who each had a transient episode of vomiting.
These controlled data parallel previous open observations. When ketamine was used as a surgical anesthetic during operations on burn patients, only 26.9% subsequently reported PTSD compared to 46.4% who developed PTSD when an alternative to ketamine was used as the anesthetic.
Childhood Adversity and Epigenetic Pockmarks
 Maltreatment in childhood may have a lasting impact on health through epigenetics. Epigenetics refers to the idea that events and substances in the environment can affect the structure of DNA by adding chemicals (often methyl or acetyl groups) onto DNA and histones (structures around which DNA is wound) in such a way that the DNA is more or less likely to be transcribed and activated to produce new proteins. Thus our DNA is shaped not only by the genetic inheritance we receive from our parents, but also by events in the environment (which do not alter the sequence of DNA but can influence how easily the DNA gets turned on to produce proteins in our bodies.)
Maltreatment in childhood may have a lasting impact on health through epigenetics. Epigenetics refers to the idea that events and substances in the environment can affect the structure of DNA by adding chemicals (often methyl or acetyl groups) onto DNA and histones (structures around which DNA is wound) in such a way that the DNA is more or less likely to be transcribed and activated to produce new proteins. Thus our DNA is shaped not only by the genetic inheritance we receive from our parents, but also by events in the environment (which do not alter the sequence of DNA but can influence how easily the DNA gets turned on to produce proteins in our bodies.)
A 2013 study by Divya Mehta et al. published in the Proceedings of the National Academy of Sciences analyzed the childhood backgrounds of adult patients with PTSD and found that patients’ profiles of disease-related gene expression and DNA methylation in blood differed greatly depending on whether or not they had experienced abuse in childhood. Adults who had been abused as children were about twice as likely to show patterns of DNA methylation accompanying their PTSD-related changes in gene expression.
The implication of this research is that childhood trauma can leave a kind of epigenetic pockmark on a person’s DNA, affecting the way the DNA produces proteins, potentially for the rest of that person’s life.
N-acetylcysteine Improves Blast-Induced Mild Traumatic Brain Injury
Michael E. Hoffer et al. reported in the journal PLosOne in 2013 that veterans with blast-induced mild traumatic brain injury had a better acute outcome when they were given the antioxidant N-acetylcysteine (NAC) within the first 24 hours after the trauma versus when they were given placebo during the same period. Forty-two percent of those receiving placebo had a good acute outcome, while 86% of those receiving N-acetylcysteine had a good acute outcome. Memory loss, sleep disturbance, dizziness, and headaches all improved more in the N-acetylcysteine group. NAC’s benefits diminished when it was given 3 or 7 days after the trauma.
Editor’s Note: These data add to the growing list of neuropsychiatric syndromes in which NAC has shown efficacy. These include schizophrenia, bipolar depression, unipolar depression, cocaine and heroin addiction, gambling addiction, trichotillomania (compulsive hair-pulling), obsessive-compulsive disorder (as an adjunctive treatment to SSRIs), and improvement in irritability and stereotypy (repetitive behaviors) in children with autism.
Given what appears so far to be a relatively benign side effects profile for NAC, and the potential for severe consequences from traumatic brain injury (TBI), a case for wider use of NAC (for example in emergency rooms) might be made.
The mechanisms of action of NAC in different syndromes remains to be clarified. Researcher Michael Berk used NAC in schizophrenia and bipolar disorder and more recently in unipolar depression because it has antioxidant properties. Peter Kalivas found that NAC can normalize glutamate in the reward area of the brain through actions on the cystine-glutamate exchanger, and it also increases clearance of glutamate by increasing the glutamate transporter in glial cells. NAC decreases the amount of cued glutamate release in a part of the brain called the nucleus accumbens, which may be helpful in recovery from pathological habits. NAC also has anti-inflammatory and perhaps neuroprotective effects, and it increases brain-derived neurotrophic factor (BDNF), which protects neurons and is important for long-term learning and memory. Which of these many actions is important in the treatment of PTSD is not yet known.
One Doctor’s Protocol for the Treatment of Severe PTSD
 Note: The following article discusses “off-label” treatments for the treatment of PTSD or traumatic brain injury, i.e. those which are not FDA-approved for these purposes. In some of these instances, there is no controlled research to support the use of these drugs in patients with PTSD. Thus the ideas noted here cannot be taken as anything more than anecdotal information from personal experience. Patients and physicians must make their own decisions about any of the strategies reported in this or other issues of BNN.
Note: The following article discusses “off-label” treatments for the treatment of PTSD or traumatic brain injury, i.e. those which are not FDA-approved for these purposes. In some of these instances, there is no controlled research to support the use of these drugs in patients with PTSD. Thus the ideas noted here cannot be taken as anything more than anecdotal information from personal experience. Patients and physicians must make their own decisions about any of the strategies reported in this or other issues of BNN.
At a recent scientific conference, Vaishali P. Bakshi, a renowned Canadian psychopharmacologist, shared a novel treatment strategy he has developed for patients with exceptionally profound degrees of post-traumatic stress disorder (PTSD), which, particularly among military veterans, can be compounded by traumatic brain injury.
Treatment options based on placebo-controlled clinical trials are sometimes insufficient for the treatment of seriously ill patients. FDA-approved treatment for PTSD consists of serotonin-selective antidepressants, while exposure therapies (in which the patient is gradually exposed to more of the stimuli that triggered symptoms) are the recommended psychotherapy, but these methods often leave patients highly disabled.
Bakshi’s typical treatment algorithm goes well beyond these treatment guidelines to find solutions for hard-to-treat patients. He first addresses sleep disturbance, which often occurs in PTSD. He suggests the anticonvulsant levetiracetam (Keppra), starting at doses of 150mg per night and increasing to 500–1000mg as tolerated. This highly sedating anticonvulsant not only improves sleep but may also help cognition, since it is structurally similar to other cognitive enhancers such as piracetam. Levetiracetam also decreases the hippocampal hyperactivity associated with some forms of cognitive dysfunction, as we’ve noted before. In order to further enhance sleep effects, Bakshi adds trazodone at 50–150mg per night as needed.
Instead of selective serotonin reuptake inhibitors (SSRIs), Bakshi recommends the selective serotonin and norepinephrine reuptake inhibitors (SNRIs). Among these, he prefers desvenlafaxine (Pristiq) over venlafaxine, as desvenlafaxine has fewer interactions with other drugs. Theoretically, duloxetine (Cymbalta) is another SNRI that could be used.
Another component of Bakshi’s treatment plan is topiramate (Topamax), which can target many comorbidities of PTSD, including alcohol and substance abuse, particularly stimulant abuse. In addition, topiramate has efficacy in anger attacks, which often accompany PTSD.
In patients with ongoing problems with depression and/or cognition, Bakshi adds bupropion (Wellbutrin). Read more
Prazosin Treats PTSD Nightmares
Patients with PTSD often struggle with nightmares, but a treatment normally used for high blood pressure may also be able to prevent these sometimes horrific dreams. In a study that marks the third replication of this finding, Murray Raskind, a researcher from the University of Seattle, reported that prazosin was significantly better than placebo at selectively blocking nightmares in 77 Iraq war veterans with PTSD in a 15-week trial. (Interestingly, normal dreaming is uninterrupted.)
Editor’s Note: Prazosin is a noradrenergic alpha-1 receptor antagonist. Doses of this drug must be titrated upward slowly over a period of 6 weeks to avoid orthostatic hypotension (a sudden fall in blood pressure that occurs when a person stands up). Maximum doses achieved in this study were 5mg mid-morning and 20mg at night (although 10mg at night is often effective). This treatment, although not FDA-approved, is increasingly being used in veteran populations and other patients with PTSD.
In Veterans, PTSD Is Associated With Autoimmune Illnesses
At a recent scientific meeting, Thomas Neylan and colleagues reported that post-traumatic stress disorder (PTSD) may be connected to autoimmune illnesses. In this study, 673,277 veterans of the US military who had served in Iraq and Afghanistan were screened for the development of PTSD. The illness was diagnosed in 31% of the veterans, and those individuals had a higher incidence of autoimmune-related disorders including thyroiditis, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, and systemic lupus erythematosus. Neylan’s research group specifically examined those whose disorders developed after the onset of the PTSD, and found that the statistical relationship between their illnesses and PTSD was strong. However, the researchers also found that there was evidence of a similarly strong relationship in the other direction: veterans who were first diagnosed with some of these same autoimmune difficulties also went on to develop PTSD.
Many previous clinical and preclinical studies have linked altered immune and autoimmune mechanisms to severe stressors such as those that are involved in PTSD. This is the first study to unequivocally demonstrate the relationship in an extraordinarily large number of patients.
Editor’s Note: These findings resemble those that suggest that among the general population, childhood adversity is associated with an increased incidence of a variety of medical disorders in adulthood. Similarly, in the Bipolar Collaborative Network in which this editor (Post) is an investigator, we found that a history of childhood adversity in patients with bipolar disorder was associated with an increased incidence of a variety of medical illnesses in adulthood, including some related to immune and autoimmune function.
More research that would measure inflammatory markers in PTSD and mood disorders is needed. It would also be important to ascertain whether treatment of mood disorders and PTSD reduces the risk of autoimmune disorders.
Neuronendocrine Function in Sexually Abused Adolescent Girls
Brooks R. Keeshin from a research group led by Frank Putnam presented a poster at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) on neuroendocrine function in recently sexually abused adolescent girls with and without post-traumatic stress disorder (PTSD). Average age of the girls was 15 and they had experienced the sexual abuse six months to one year before the study. The researchers found that morning cortisol awakening response was flattened in the girls, and this was associated with PTSD severity and the severity of intrusive symptoms. Increased adversity prior to the sexual abuse experience was also associated with flattening of the cortisol awakening response.
The researchers suggest that alterations in the hypothalamic pituitary adrenal axis (HPA) appear around the time of the abuse and are associated with the severity of PTSD symptomatology in sexually abused adolescent girls.
Memory Consolidation and Reconsolidation: Cortisone after trauma could prevent PTSD
 Memories are created in a series of phases in which different neurobiological mechanisms are required. In order for short-term memories to be placed in long-term storage, new protein synthesis is required. If protein synthesis is inhibited during a window about 2-4 hours after the short-term memory was encoded, consolidation into long-term memory does not occur.
Memories are created in a series of phases in which different neurobiological mechanisms are required. In order for short-term memories to be placed in long-term storage, new protein synthesis is required. If protein synthesis is inhibited during a window about 2-4 hours after the short-term memory was encoded, consolidation into long-term memory does not occur.
In addition to the initial phase of memory consolidation, a second phase of memory reconsolidation is now recognized. During this phase, memory is again alterable.
The alterability of memories has implications for some types of post-traumatic stress disorder (PTSD), in which emotional memories repeatedly intrude into consciousness. Pharmacological intervention during the period of memory reconsolidation may be able to reduce the impact of traumatic memories.
One example of an attempt to alter memory consolidation or reconsolidation after trauma has been reported by researcher Ariel Shalev and colleagues. These researchers found that administration of a high dose of intravenous cortisone (100 to 240mg) immediately following an extreme trauma was able to decrease the incidence of PTSD. One month after a traumatic event, the incidence of PTSD was 60% in those who received placebo, compared to only 16% in those who received the intravenous cortisone.
Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
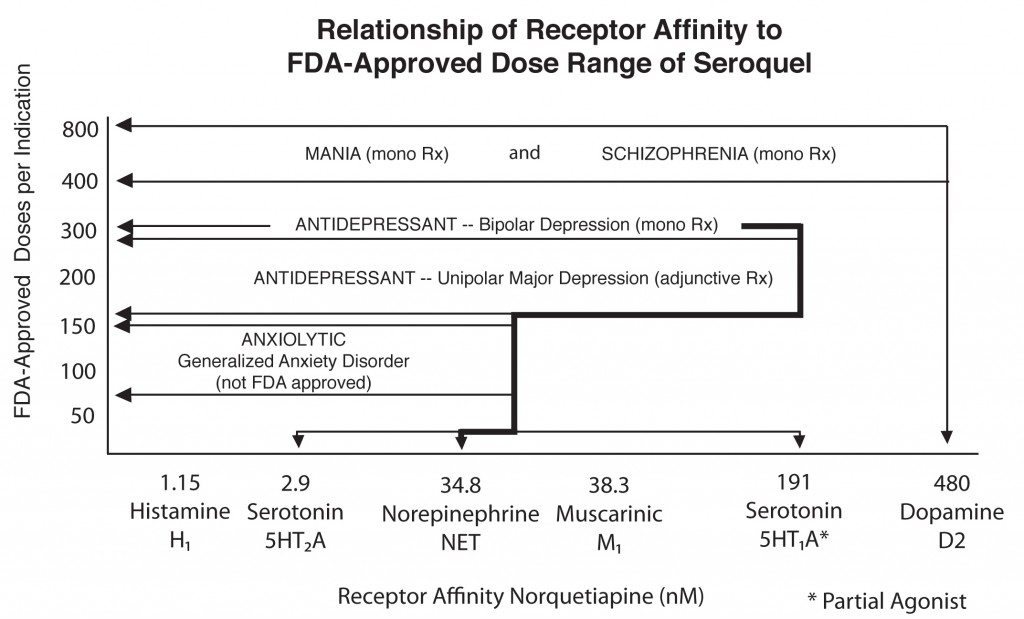
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Read more







