Vagus Nerve Stimulation Improves Depression When Other Treatments Fail
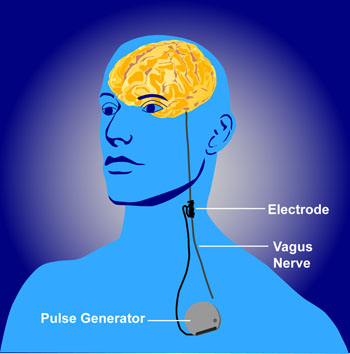
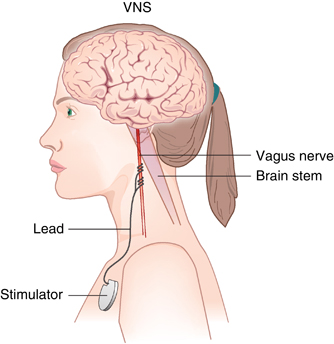 Vagus nerve stimulation (VNS) has been approved by the US Food and Drug Administration as an adjunctive therapy for treatment-resistant unipolar and bipolar depression since 2005. The treatment consists of a pacemaker-like device implanted under the skin in the chest that delivers regular, mild electrical pulses to the brain via the left vagus nerve.
Vagus nerve stimulation (VNS) has been approved by the US Food and Drug Administration as an adjunctive therapy for treatment-resistant unipolar and bipolar depression since 2005. The treatment consists of a pacemaker-like device implanted under the skin in the chest that delivers regular, mild electrical pulses to the brain via the left vagus nerve.
A 2017 study by Scott T. Aaronson and colleagues in the American Journal of Psychiatry reports that over a 5-year period, people with treatment-resistant depression who received VNS did better than those who received treatment as usual. The 795 participants at 61 US sites had either a depressive episode that had lasted for at least two years or had had three or more depressive episodes and had failed to respond to at least four treatments, including electroconvulsive therapy (ECT). Over five years, those who received VNS had higher response rates (67.6% versus 40.9%) and higher remission rates (43.3% versus 25.7%) compared to those who received treatment as usual.
While the study by Aaronson and colleagues was non-blind and non-randomized, it suggests that VNS could be helpful in the long-term management of treatment-resistant unipolar and bipolar depression.
Editor’s Note: VNS was FDA-approved for treatment-resistant seizures in patients aged 12 and older in 1997 and for children 4 years and older in 2017. It was also approved for cluster headaches in 2017. Insurance coverage and reimbursement for VNS is typically available for these neurological conditions, but not for the treatment of depression. This is an unfortunate example of the stigmatization of psychiatric illness—when an FDA-approved device can be kept from people in need of treatment.
VNS Covered For Reimbursement For Refractory Epilepsy But Not Refractory Depression
 The federal Centers for Medicare and Medicaid Services (CMS) appear to discriminate against people with psychiatric illness. They will not approve the use of VNS (Vagus Nerve Stimulation) for treatment resistant depression among Medicare beneficiaries but have approved it for refractory epilepsy.
The federal Centers for Medicare and Medicaid Services (CMS) appear to discriminate against people with psychiatric illness. They will not approve the use of VNS (Vagus Nerve Stimulation) for treatment resistant depression among Medicare beneficiaries but have approved it for refractory epilepsy.
Vagus nerve stimulation consists of electrical stimulation of the vagus, one of the cranial nerves. The Federal Drug Administration (FDA) has already approved VNS for both illnesses, meaning that it has been judged to be effective and safe in both.
The CMS decision will make it harder for poor patients to access this treatment because it means that Medicare will not reimburse the cost of the treatment.
Cyberonics, the company that manufactures the device used to provide VNS, applied for CMS approval of the use of VNS for depression in 2007 and was rejected, but hoped that the research collected in the intervening years that shows VNS’s efficacy in treatment-resistant depression would be enough to get eventual approval from CMS. They have been rejected again.
Editor’s Note: The data supporting VNS’s efficacy in epilepsy are skimpy and without a large effect size, so it cannot be argued that the quality of data supporting the coverage of VNS for depression is the reason it hasn’t been approved for that purpose. Both epilepsy and depression can be devastating and life altering. To support the use and reimbursement for the same FDA-approved device for one but not the other illness seems worthy of protest.
This appears to be another example of the incongruous use of FDA approval status to deny coverage. Insurance companies and government agencies routinely use lack of FDA approval to deny reimbursement claims for many commonly used drugs and treatments, while at the same time, in cases such as the use of VNS, actual FDA approval is disregarded and considered an insufficient criterion. Having it both ways does not seem to bother the policy makers who appear to put the financial bottom line ahead of ethics, fairness, and good medical care.

