Translocator Protein Levels in Brain Predict Response to Anti-Inflammatory Celecoxib in Major Depressive Disorder
Gliosis describes changes in glia that result from damage to the central nervous system. Researchers can use PET scans (positron emission tomography) to measure the extent of gliosis in the brain. But a new study explored whether these PET scans could instead be used to determine who might respond to a given medication.
Researcher Sophia Attwells and colleagues reported in the journal Biological Psychiatry in 2020 that people with high levels of translocator protein (TSPO), a measure of gliosis and inflammation, had a better antidepressant response to the anti-inflammatory drug celecoxib than patients who started out with lower levels of TSPO.
The study participants, who had treatment-resistant depression, all received 200mg of the anti-inflammatory drug celecoxib twice/day for eight weeks on an open (non-blind) basis. Before they began taking celecoxib, the participants received PET scans to measure translocator protein total distribution volume (TSPO VT) in the prefrontal cortex and the anterior cingulate cortex.
Patients with high levels of TSPO showed greater reductions in depression ratings over the course of the study than those with normal levels of TSPO at baseline.
Attwells and colleagues conclude that “this personalized medicine approach of matching a marker of gliosis to [an anti-inflammatory treatment] …should be applied in early development of novel therapeutics, in particular for [treatment-resistant depression].”
Editor’s Note: These findings are of considerable importance, as they are among the first to indicate that measures of inflammation may predict response to an anti-inflammatory medication such as celecoxib. In a 2013 article in the journal JAMA Psychiatry, Charles L. Raison and colleagues reported that patients with high levels of the peripheral inflammatory marker CRP saw marked improvement in their depression when they received the anti-inflammatory treatment infliximab while those with lower or normal levels of inflammation actually worsened.
Dr. Post’s Recommendations For Treating Youth with Bipolar Symptoms
Our Editor-in-Chief, Dr. Robert M. Post, shares his personal recommendations for the treatment of children and adolescents with symptoms of bipolar disorder. Remember: Patients and family members must consult a physician about all information conveyed in the BNN. With the exception of lithium, none of the medications or supplements discussed above have been approved by the US Food and Drug Administration for use in children under 10. The findings reported here are in many cases preliminary and cannot be taken as recommendations based on the short summaries provided here. All treatment decisions must be made in conjunction with a patient’s treating physician, who is solely responsible for initiating any treatment discussed in the BNN or elsewhere.
In symptomatic and functionally impaired children, medication is almost always necessary. Many treating psychiatrists would start with an atypical antipsychotic, since there is clear evidence of the efficacy of such treatments. The side effects profile should be considered, as there is a considerable difference in the degree of weight gain associated with different atypical antipsychotics. The largest weight gains occur with olanzapine and clozapine, intermediate gains occur with aripiprazole and quetiapine, and the least gains occur with ziprasidone and lurasidone (and the latter has the advantage of being approved by the US Food and Drug Administration for the treatment of bipolar depression in children who are 10–17 years old). The addition of the diabetes drug metformin to decrease weight gain in people taking atypical antipsychotics is increasingly common.
The addition of an anticonvulsant medication (such as lamotrigine, carbamazepine/oxcarbazepine, or valproate) or the mood stabilizer lithium may be needed, as multiple studies indicate that combination treatment is typically needed in children (as in adults) to achieve a more complete response or remission.
Interestingly, oxcarbazepine was effective in younger but not older children with mania in a previous placebo-controlled study by Karen D. Wagner and colleagues published in the American Journal of Psychiatry in 2006.
Conversely, in a 2015 article in the journal JAACAP, researcher Robert Findling reported that in a placebo-controlled study of lamotrigine, 13–17-year-olds responded better than 10–12-year-olds.
Lithium treatment deserves consideration in children with classical presentations of bipolar disorder and those who have family members who have responded well to lithium treatment.
Lithium has the benefit of improving the white matter abnormalities seen in the brains of patients with early-onset bipolar disorder. Hafeman and colleagues reported in a 2019 article that children with bipolar disorder who were treated with lithium had better long-term results upon follow up than those treated with atypical antipsychotics or anticonvulsants.
There is much less scientific consensus about other adjunctive treatments for young people with additional bipolar symptoms and comorbidities, but this editor often uses several. Vitamin D3 is often low in children with psychiatric illness, and may improve mood and cognition.
The antioxidant N-acetylcysteine (NAC) helps depression, anxiety, and irritability, and is effective at treating habit-related behaviors such as trichotillomania (compulsive hair-pulling), obsessive-compulsive disorder (OCD), and drug use, including specifically reducing marijuana use in adolescents. A typical dose is 500–600 mg capsules, one capsule twice a day for one week, then two capsules in the morning and two in the evening thereafter.
Folate or folic acid may enhance antidepressant effects and those of lithium. In patients who have a particular low-functioning variant of a gene known as MTHFR, L-methylfolate is required instead of folate.
The widely-used supplement acetyl-L-carnitine (ALC) is poorly studied in children, but deserves consideration as a supplemental treatment for patients with histories of childhood adversity. In adults with depression, blood levels of ALC may be low, particularly in those with an early onset of bipolar symptoms and a history of childhood adversity (see a 2018 article by Carla Nasca in the journal PNAS). There is a modicum of evidence that ALC produces antidepressant effects in adults. ALC may also sensitize insulin receptors and normalize blood pressure.
There is increasing evidence of the role of inflammation in depression, mania, post-traumatic stress disorder (PTSD), and schizophrenia. Checking for abnormalities in inflammatory markers in the blood (especially Il-6 and CRP) may point the way to appropriate therapy with anti-inflammatory drugs such as minocycline (100 mg twice a day) or celecoxib (200 mg twice a day) in patients who do not respond fully to first-line medications.
Measuring Inflammation in Neuropsychiatric Disorders May Shed Light on Treatment
Meta-analyses have found links between elevated levels of inflammatory markers and many neuropsychiatric disorders, including depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and traumatic brain injury. Multiple studies also show that those with elevated inflammatory markers such as interleukin-1, interleukin-6, tumor necrosis factor (TNF) alpha, and c-reactive protein (CRP) also respond less well to typical treatments than those with normal levels of these markers in the blood.
These links suggest that it could be useful to measure levels of these inflammatory markers in the blood of people who are responding poorly to medications. If one or more of these markers are elevated, it might be a sign that treatment with an anti-inflammatory agent could be helpful. Preliminary studies have shown that some neuropsychiatric disorders may improve after treatment with anti-inflammatory drugs such as aspirin, celecoxib (Celebrex), and the antibiotic minocycline, among others.
Arthritis Drug Celecoxib May Improve Bipolar Depression When Paired with Escitalopram
A new study suggests that for people with bipolar depression, the anti-inflammatory drug celecoxib (Celebrex), typically used to treat arthritis, can boost the effectiveness of the antidepressant escitalopram (Lexapro).
In the 8-week study by researcher Angelos Halaris and colleagues, adults with bipolar depression were randomly assigned to one of two groups. The first group received the selective-serotonin reuptake inhibitor (SSRI) antidepressant escitalopram plus celecoxib to target inflammation. The second group received just the antidepressant escitalopram and a placebo.
By the end of the study, 78% of the group taking the anti-arthritis drug had seen major improvement in their depression, with 63% reporting that it had lifted completely. Meanwhile in the placebo group, only 45% reported major improvement, and 10% reported remission.
The group that received celecoxib with their escitalopram also began seeing improvement within one week of beginning treatment, instead of after four to six weeks, which is typical of antidepressant treatment.
Researchers think depression creates an immune response leading to chronic inflammation, which can upset the balance of neurotransmitters in the brain and make antidepressants less effective. Halaris suggests that reducing this inflammation with a drug like celecoxib can make antidepressants more effective.
The research was presented at the Fifth International Congress on Psychiatry and the Neurosciences and has not yet been published.
Anti-Inflammatory Treatments Improve Depression
Inflammation can interfere with the balance of neurotransmitters in the brain, making antidepressants less effective. Anti-inflammatory treatments (such as those used to treat rheumatoid arthritis) may help. In a 2016 meta-analysis published in the journal Molecular Psychiatry, researchers led by Nils Kappelmann analyzed the results of 20 clinical trials of chronic inflammatory conditions where depressive symptoms were also recorded. In a subset of 7 clinical trials that compared anti-inflammatory treatment to placebo, they found that anti-inflammatory treatment improved depressive symptoms significantly compared to placebo.
The anti-inflammatory drugs studied most often targeted the inflammatory marker tumor necrosis factor (TNF) alpha using an antibody. Some of the anti-inflammatory drugs that improved depressive symptoms were adalimumab, etanercept, infliximab, and tocilizumab.
The researchers also found that those participants with the most inflammation when they began treatment saw the largest improvement in their depression after taking anti-inflammatory treatments.
Kappelmann and colleagues suggest that inflammation may cause depression, and that anti-inflammatory drugs may be useful in the treatment of depression in people with high inflammation.
Kynurenine Pathway Suggests How Inflammation is Linked to Schizophrenia
The kynurenine pathway describes the steps that turn the amino acid tryptophan (the ingredient in turkey that might make you sleepy) into nicotinamide adenine dinucleotide. This pathway might be a connection between the immune system and neurotransmitters involved in schizophrenia.
A recent autopsy study by researcher Thomas Weickert and colleagues explored this link by determining that in the brains of people with schizophrenia and high levels of inflammation, messenger RNA for Kynurenine Aminotransferase II (KATII, a step on the kynurenine pathway) was elevated in the dorsolateral prefrontal cortex compared to the brains of people who died healthy and those with schizophrenia but low levels of inflammation.
The KATII mRNA levels also correlated with mRNA levels of inflammatory markers such as glial fibrillary acidic protein and interleukin-6.
Blood measures related to the kynurenine pathway also differentiated people with schizophrenia from healthy controls. People with schizophrenia had lower levels of tryptophan, kynurenine, and kynurenic acid in their blood. The low levels of kynurenic acid in the blood were correlated with deficits in working memory and smaller volume of the dorsolateral prefrontal cortex.
Weickert and colleagues suggest that blood levels of kynurenic acid might provide a measurable indicator of the degree to which people with schizophrenia are experiencing problems with executive functioning (planning and decision-making) and loss of brain volume.
Meta-Analysis Shows Anti-Inflammatory Treatments Improve Bipolar Depression
 It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
Researcher Joshua D. Rosenblat and colleagues identified eight randomized controlled trials that met their criteria for anti-inflammatory treatments of bipolar disorder. These treatments included nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen and aspirin), omega-3 fatty acids, the antioxidant N-acetylcysteine, and pioglitazone (used to treat diabetes). Overall, the anti-inflammatory treatments had a moderate and statistically significant antidepressant effects. No serious side effects were reported, and the anti-inflammatory treatments did not cause a switch into mania in any of the participants.
The diversity of the anti-inflammatory treatments reviewed in this meta-analysis limit the extent to which it can be interpreted, but it is clear that more research on anti-inflammatory treatments for bipolar depression is needed. An open question is whether patients with particularly elevated levels of inflammatory markers in their blood would respond better to these anti-inflammatory treatments.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
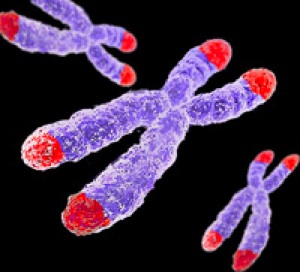
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
Anti-Inflammatory Treatments Look Promising for Bipolar Depression
Inflammation has been linked to both unipolar and bipolar depression. New research shows that anti-inflammatory treatments may reduce bipolar depression, for which few treatments exist.
Researchers led by Jonathan Savitz divided people with bipolar depression into four groups. One group received two placebos, another received minocycline (a drug with neuroprotective and immune-modulating properties) plus a placebo, the third received aspirin plus a placebo, and the final group received both minocycline and aspirin. Of the 64 participants, those who took both minocycline and aspirin were most likely to respond to treatment and to enter remission. In people with body mass indexes (BMIs) above the median of 30, a sign of greater inflammation, 100% of those who received both anti-inflammatory drugs responded to treatment, compared to 36% of those who received aspirin alone, 33% of those who received minocycline alone, and 25% of those who received two placebos.
Dosages of the drugs were 100mg twice a day for minocycline and 81mg twice a day for aspirin. Savitz and colleagues believe that aspirin and minocycline must work particularly well together, and are modifying their study to more directly compare use of the two anti-inflammatory drugs together to the absence of anti-inflammatory treatments.
Anti-Inflammatory Treatments May Improve Depressive Symptoms
Studies have found that inflammatory molecules play a role in depression. A recent study by researcher Yu Sun and colleagues used data from clinical trials of anti-inflammatory drugs to show that these drugs also reduced depressive symptoms. The two drugs, which are administered either by a shot or injection into the skin, each consist of antibodies that target the inflammatory molecule IL-6. Sirukumab is being looked at as a possible treatment for rheumatoid arthritis, while siltuximab is a potential treatment for Castleman’s disease, an illness characterized by enlarged lymph nodes. As part of the clinical trials for these drugs, patients with these illnesses responded to survey questions that assessed symptoms of depression and fatigue.
Among patients who reported that they have at least one depressive symptom most of the time and another symptom at least part of the time, the anti-inflammatory drugs significantly improved depressive symptoms compared to placebo. Even when the patients’ inflammatory illnesses did not respond to the anti-inflammatory treatments, their depressive symptoms did improve (symptoms of fatigue did not). An improvement in depressive symptoms was observed after 6 weeks in patients with Castleman’s disease taking siltuximab, and after 12 weeks in patients with rheumatoid arthritis taking sirukumab.
In the sirukumab study, the level of the inflammatory molecule IL-6 in participants’ blood before the study was linked to the magnitude of improvement in their depressive symptoms during the study. IL-6 is elevated in many patients with unipolar and bipolar depression. It is possible that antibodies that target IL-6 could be used to treat primary depression (in the absence of other inflammatory disorders).