Longer Periods of Untreated Depression Linked to More Brain Inflammation
 A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
The study published in the journal The Lancet Psychiatry used positron emission tomography (PET scan) to examines levels of translocator protein in the brain. Higher levels of translocator protein indicate activation of microglia, the brain’s immune cells, which can respond to trauma or injury.
The study included 80 participants between the ages of 18 and 75. Ten had a history of more than 10 years of depression, ten had experienced fewer than 10 years of depression, and 30 comprised a healthy comparison group.
The best predictors of high levels of translocator protein were duration of untreated major depressive disorder, total illness duration, and duration of antidepressant exposure. These three factors explained about half of the variation in translocator protein levels. Those participants whose depression went untreated for 10 years or longer had inflammation levels 29–33% higher than those whose depression was untreated for 9 years or less.
Participants who had received antidepressant treatment appeared to avoid an average yearly increase in the extent of their microglial activation.
The study took place at Canada’s Centre for Addiction and Mental Health.
Editor’s Note: Since inflammation is a predictor of poorer response to antidepressants, these data add a further neurochemical rationale to the already strong clinical rationale for earlier and more sustained antidepressant treatment and prevention. Virtually all treatment guidelines suggest that after two or three prior unipolar depressions, patients should receive long-term (lifelong) antidepressant treatment.
There is now a large body of data, including a 2012 article by this editor Robert M. Post and colleagues in the Journal of Psychiatric Research that too many episodes can hurt the brain, and the current study adds to this perspective. Avoiding preventive treatment for too long may actually foster the development of more episodes and more treatment resistance. A good mantra is “prevent episodes, protect the brain.”
Consensus is now also building that comprehensive long-term treatment is indicated after a first manic episode. A 2013 article by Lars Kessing and colleagues in the British Journal of Psychiatry suggested that high quality initial treatment can improve the long-term course of illness. Moreover, a 2016 article by Jan-Marie Kozicky and colleagues and a 2017 article by Christine Demmo and colleagues, both in the journal Bipolar Disorders, suggest that after a first mania, cognition recovers over the next year only if no further episodes occur in that time.
In Animals, Exposure to High Fat Diet During Pregnancy Can Affect Offspring’s Neurological Development
New research in non-human primates suggests that exposure to a high fat diet during pregnancy and in early development prior to weaning can increase the offspring’s propensity for anxiety later in life.
The new research echoes 2010 findings about rats. Researcher Staci D. Bilbo and colleagues reported in the journal of the Federation of American Societies for Experimental Biology that in rats, a high fat diet during pregnancy and lactation led to offspring with greater body weight, increased inflammation, and problems with anxiety and spatial learning. Switching to a standard diet after weaning did not eliminate these outcomes.
The recent research by Jacqueline R. Thompson and colleagues, published in the journal Frontiers in Endocrinology in July 2017, suggests that maternal nutrition in the primate during pregnancy and lactation can have long-lasting effects on offspring’s neurological development, altering the brain and endocrine system. These changes occurred even if the offspring began a normal diet after weaning.
65 female Japanese macaques were divided into two groups, one that received a high-fat diet and one that received a normal diet. In the offspring of mothers who ate a high-fat diet, the researchers found impaired development of neurons containing serotonin. The offspring of the high-fat diet group also showed behavioral alterations such as increased anxiety.
The high rates of obesity in the US and other developed nations make these findings particularly important. The researchers suggest that 64% of women in the US who are of reproductive age are overweight, and 35% are obese. Co-author Elinor Sullivan suggested that the findings from the study could motivate mothers to make healthy nutritional decisions, not only for themselves but for their children as well.
Depression and Suicidal Thoughts Linked to Brain Inflammation
A 2017 article by Sophie E. Holmes and colleagues in the journal Biological Psychiatry reports that people with major unipolar depression, especially those with suicidal thoughts, have higher levels of the inflammatory marker translocator protein than do healthy individuals.
The participants with depression and suicidal thinking had high levels of translocator protein in the anterior cingulate cortex, which suggests that inflammation is affecting microglia.
Many studies have found links between different indicators of inflammation and mood disorders, leading researchers to speculate whether targeting the immune system could be an effective way to treat mood disorders. Patients with high levels of inflammation often fail to respond to typical treatments for depression.
Some previous research has found evidence of microglial activation in the brains of people who died from suicide.
The small study by Holmes and colleagues used positron-emission tomography, or PET scans, to observe evidence of translocator protein levels in the brain in 14 medication-free participants in a major depressive episode and 13 healthy volunteers. Those with depression, and particularly those with suicidal thoughts, showed more evidence of neuroinflammation.
An Inflammatory State Impedes Treatment for Bipolar Disorder
 A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
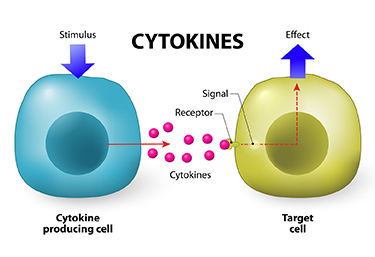
Researcher Francesco Benedetti and colleagues report that high levels of inflammatory cytokines (a type of small proteins) predicted a worse response to treatment with sleep deprivation and light therapy for bipolar depression. This treatment typically brings about a rapid antidepressant response.
Benedetti and colleagues measured 15 immune-regulating compounds in 37 patients who were experiencing an episode of bipolar depression and 24 healthy volunteers. Among those participants with bipolar disorder, 84% had a history of non-response to medication. Twenty-three of the 37 patients, or 62%, responded to the sleep deprivation/light therapy combination. Those who did not had higher levels of five cytokines: interleukin-8, monocyte chemoattractant protein-1, interferon-gamma, interleukin-6, and tumor necrosis factor-alpha.
Body mass index was correlated with cytokine levels and also reduced response to the treatment.
The finding supports a link between the immune system and mood disorders. Evaluating a patient’s level of inflammation may, in the future, allow doctors to predict the patient’s response to a given therapy. Patients with high levels of inflammation might benefit most from treatments that target their immune system.
Simvastatin Looks Promising in Treatment of Negative Symptoms of Schizophrenia
The statin drug simvastatin (Zocor) enhances the effects of risperidone on negative symptoms of schizophrenia, according to a 2017 article by Soode Tajik-Esmaeeli and colleagues in the journal International Clinical Psychopharmacology.
In the 8-week study, 40 mg/day of simvastatin enhanced the effects of 4–6 mg/day of the antipsychotic risperidone on negative symptoms of schizophrenia, such as apathy and withdrawal, but not positive symptoms such as hallucinations or delusions.
Other statins, lovastatin and pravastatin, have not had a similar effect, possibly because they do not cross the blood-brain barrier as easily as simvastatin does.
Simvastatin has other benefits as well. Like all statins it decreases lipid levels, reducing cardiovascular disease. People with schizophrenia and bipolar disorder are at especially high risk for cardiovascular disease.
Simvastatin also decreases inflammation (lowering IL-1 alpha and TNF-beta levels) and may be neuroprotective, as it increases brain-derived neurotrophic factor (BDNF), a protein that protects neurons and is important for learning and memory. Inflammation is increasingly implicated in schizophrenia and bipolar disorder.
There is also some evidence that statins can prevent depressions over long-term follow-up. Studies in women without depression and men who had recently had heart attacks both showed that those taking statins had a lower rate of future depression than those not taking statins.
Editor’s Note: These findings suggest a potential 5-fold benefit to simvastatin: 1) It reduces negative symptoms in schizophrenia. 2) It reduces inflammation. 3) It increases BDNF. 4) It decreases cardiovascular disease risk by lowering lipid levels. 5) It may prevent future depressions.
Other approaches to augmenting schizophrenia treatment include nutritional supplements vitamin D3 and folate. Patients with psychosis often have vitamin D deficits. Folate supplements can reduce homocysteine, which has been linked to cognitive deficits in schizophrenia.
Inflammation Predicts Poor Response to Sleep Deprivation with Light Therapy
A 2017 article by Francesco Benedetti and colleagues in the Journal of Clinical Psychiatry reports that people with bipolar depression who have higher levels of certain inflammatory markers may have a poor antidepressant response to the combination of sleep deprivation and light therapy, compared to those with lower levels of inflammation.
The study included 37 participants with bipolar disorder who were in the midst of a major depressive episode. Of those, 31 participants (84%) had a history of poor response to antidepressant medication. The patients were treated with three cycles of total sleep deprivation and light therapy within one week, a combination that can often bring about a rapid improvement in depression.
Depression improved in a total of 23 patients (62%) following the therapy. Blood analysis showed that compared to those who had a good response, the non-responders had higher levels of five intercorrelated inflammatory markers: IL-8, MCP-1, IFN-gamma, IL-6, and TNF-alpha. Those with higher body mass index had more inflammation, indirectly decreasing response to the therapy.
Teens with Bipolar Disorder at Increased Risk for Cardiovascular Disease
 A scientific statement from the American Heart Association reported in 2015 that youth with major depressive disorder and bipolar disorder are at moderate (Tier II level) increased risk for cardiovascular disorders. The combined prevalence of these illnesses in adolescents in the US is approximately 10%.
A scientific statement from the American Heart Association reported in 2015 that youth with major depressive disorder and bipolar disorder are at moderate (Tier II level) increased risk for cardiovascular disorders. The combined prevalence of these illnesses in adolescents in the US is approximately 10%.
There are many factors that contribute to this risk, including inflammation, oxidative stress (when the body falls behind neutralizing harmful substances produced during metabolism), dysfunction in the autonomic nerve system, and problems with the endothelium (the inner lining of blood vessels). Lifestyle factors include adversity in early life, sleep disturbance, sedentary lifestyle, poor nutrition, and abuse of tobacco, alcohol, or other substances.
Taking some atypical antipsychotics as treatment for bipolar disorder also contributes to the risk of cardiovascular problems by increasing weight and/or lipid levels. Among the atypicals, ziprasidone (Geodon) and lurasidone (Latuda) come with the lowest likelihood of weight gain.
The statement by Benjamin I. Goldstein and colleagues that appeared in the Heart Association-affiliated journal Circulation suggested that therapeutic interventions should address some of these risk factors to help prevent cardiovascular problems and improve life expectancy for young people with depression or bipolar disorder. These could include a good diet, regular exercise, and treatments with good long-term tolerability that are aimed at preventing episodes.
The Role of Inflammatory Markers and BDNF
Inflammation worsens the risk of cardiovascular problems, while brain-derived neurotrophic factor (BDNF), which protects neurons and plays a role in learning and memory, may improve prospects for someone with depression or bipolar disorder.
A 2017 article by Jessica K. Hatch and colleagues including Goldstein in the Journal of Clinical Psychiatry suggests that inflammation and BDNF are mediators of cardiovascular risk in youth with bipolar disorder. The study looked at 40 adolescents with bipolar disorder and 20 healthy controls.
Those with bipolar disorder had greater waist circumference, body mass index, and pulse pressure than the controls. The youth with bipolar disorder also had higher levels of the inflammatory cytokine Il-6. Participants who had lower BDNF had greater thickness of the carotid vessel internal lining (intima media).
Hatch and colleagues point to the importance of prevention strategies in adolescents with these indicators of increased cardiovascular risk. These data complement the American Heart Association’s recognition of adolescent mood disorders as a large problem that deserves wider attention both in psychiatry and in the media.
Immune Response to Repeated Stress Alters Behavior in Mice
In research presented at the 2016 meeting of the Society of Biological Psychiatry, Jonathan P. Godbout described how an immune reaction to repeated stressors may lead to anxious behaviors in mice.
Mice were repeatedly defeated by a larger animal, a form of stress that produces a depression-like state. This provoked an immune response in the mice—the release of a type of white blood cells called monocytes from the bone marrow into the circulatory system. These inflammatory monocytes then traveled to the brain and spleen, attracted by signaling proteins called chemokines. The monocytes in turn produced inflammatory marker interleukin-1beta.
The defeat stress also provoked a reaction in the central nervous system, where microglia were activated.
These changes produced inflammation and anxiety-like behaviors in the mice. Blocking the microglial activation, monocyte recruitment to the brain, or interleukin-1beta signaling each reversed the anxiety-like behaviors.
Another researcher, Scott Russo, has shown that leukocytes, another type of white blood cells, secrete inflammatory interleukin-6 following defeat stress, and blocking this secretion prevents defeat stress–related behaviors.
Inflammation Predicts Poor Response to Fluoxetine in Kids
Inflammation upsets the balance of neurotransmitters in the brain and can make antidepressants less effective. In new research by Maya Amitai and colleagues, children and adolescents were less likely to respond to the selective serotonin reuptake inhibitor (SSRI) antidepressant fluoxetine if they had high levels of inflammation measured in the blood.
Amitai’s study included 41 patients between the ages of 9 and 18. They met criteria for a diagnosis of either major depression or an anxiety disorder. The participants were treated with the SSRI fluoxetine for eight weeks. Those with high levels of the inflammatory markers tumor necrosis factor (TNF) alpha, interleukin-6, and interleukin 1 beta were less likely to respond to the antidepressant treatment. The research was published in the Journal of Child and Adolescent Psychopharmacology in 2016.
Editor’s Note: These findings parallel those from studies of adults, suggesting that inflammation can predict poor response to antidepressants in all age groups.
Mysteries Remain in the Relationship Between Inflammation and Depression
At the 2017 meeting of the American College of Psychiatrists, researchers Charles L. Raison and Vladimir Maletic gave a plenary lecture on the role of inflammation in depression. Meta-analyses have confirmed that inflammatory markers including Il-1, Il-6, TNF alpha, and CRP are elevated in about 1/3 of depressed patients. However, Raison and Maletic made the point that anti-inflammatory medications are not for everyone. While patients with elevated levels of CRP at baseline responded to an anti–TNF alpha antibody, patients with low CRP values at baseline actually got worse.
Raison and Maletic cited three studies that have also linked CRP to differential response to traditional antidepressants. In unipolar depression, those with low CRP respond well to selective serotonin reuptake inhibitor (SSRI) antidepressants, while those with elevated blood levels of CRP seem to respond better to a dopamine-active antidepressant such as bupropion or a noradrenergic-active antidepressant such as nortriptyline or the serotonin norepinephrine reuptake inhibitor (SNRI) antidepressant duloxetine. Patients with high inflammation at baseline also seem to respond better to intravenous ketamine and oral doses of omega-3 fatty acids.
Studies of animals have suggested that inflammation throughout the body is implicated in depression. Studies in which rodents are repeatedly defeated by larger animals show that these animals have increased inflammation from lymphocites (a type of white blood cells) in the blood, and monocytes (another type of white blood cells) from the bone marrow and spleen. This inflammation can induce depression-like behaviors in the rodents, which is prevented if the inflammatory mechanisms are blocked. These data suggest that depression is not just in the brain—inflammation from all over the body plays an important role.
Read more