Treating Prenatal Depression Improves Outcomes for Mothers and Babies
 A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
The 2016 study by Kartik K. Venkatesh and colleagues in the journal Obstetrics & Gynecology included 7,267 women who gave birth after at least 20 weeks of pregnancy. About 11% of the women screened positive for depression during their pregnancy. Depressed mothers-to-be were more likely to give birth before 37 weeks and before 32 weeks compared to nondepressed mothers-to-be. The depressed women were also more likely to deliver small babies or babies weighing under 2500g.
About 7% of the women in the study received antidepressant medication. Compared to nondepressed women, the women taking antidepressants did not have greater rates of early delivery or small babies. However, the authors caution that because so few women received antidepressants, the study does not reveal whether antidepressants improve outcomes for depressed pregnant women.
L-methylfolate Improves Depression; More Effective in Overweight Patients with Inflammation
A 2012 study by Geoge I. Papkostas and colleagues found that 15mg/day of the nutritional supplement l-methylfolate calcium (a form of the B vitamin folate that the body can more readily use) improved depression in people who had not responded adequately to treatment with a selective serotonin reuptake inhibitor (SSRI) antidepressant. In a follow-up study by Richard C. Shelton and colleagues published in the Journal of Clinical Psychiatry in 2015, the same researchers further analyzed these data and found that l-methylfolate worked better in patients who were overweight (with body mass indexes (BMIs) of 30 or above) and those who had higher than average levels of inflammation at the beginning of the study. Inflammatory markers linked to greater improvement with l-methylfolate included TNF-alpha, IL-8, high sensitivity CRP, and leptin. In overweight participants, higher than average levels of IL-6 were also linked to more improvement on l-methylfolate.
Stimulants Linked to Psychotic Symptoms in Offspring of Parents with Psychiatric Illness
Stimulants are one of the most common medications prescribed to children and adolescents, typically for attention deficit hyperactivity disorder (ADHD). In children of parents with major depression, bipolar disorder, or schizophrenia, stimulant use may come with a risk of psychotic symptoms. A 2016 study by L.E. MacKenzie and colleagues in the journal Pediatrics reported that among children and youth whose parents had one of these psychiatric illnesses, 62.5% of those who had taken stimulants had current psychotic symptoms, compared to only 27.4% of those who had not taken stimulants. The participants with psychotic symptoms tended to have hallucinations that occurred while they were taking stimulants. Doctors may want to consider whether parents have a history of psychiatric illness when deciding whether to prescribe stimulants to children and adolescents with ADHD. Activation is a common side effect of antidepressants in children who have a parent with bipolar disorder. Young people taking stimulants for ADHD should be monitored for psychotic symptoms, particularly if they have a parent with a history of depression, bipolar disorder, or schizophrenia.
Long-Acting Injectable Aripiprazole Approved for Schizophrenia
 In October, the US Food and Drug Administration (FDA) approved an injectable, long-acting version of the atypical antipsychotic aripiprazole for the treatment of adults with schizophrenia.
In October, the US Food and Drug Administration (FDA) approved an injectable, long-acting version of the atypical antipsychotic aripiprazole for the treatment of adults with schizophrenia.
The long-acting aripiprazole is administered every 4 to 6 weeks as an injection in the arm or buttocks. The company announced that it would begin releasing the drug immediately. The drug preparation for maintenance treatment is named Maintena while the preparation for acute treatment is named Aristada.
Children at Risk for Bipolar Disorder May Have Adverse Reactions to Antidepressants
 At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
Younger patients at risk for bipolar disorder were more likely to have an adverse reaction to antidepressants. Risk of an adverse reaction decreased 27% with each year of age.
Topiramate Added to Quetiapine Can Reduce Marijuana Craving in Young People
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. DelBello reported that compared to placebo, the anticonvulsant topiramate reduced marijuana craving in young people aged 12–21 who were already taking the antipsychotic quetiapine. Functional magnetic resonance imaging (fMRI) revealed that topiramate altered the activation of brain regions common to both drug craving and mood dysregulation. Topiramate could be a good treatment to reduce marijuana abuse. The antioxidant n-acetylcysteine (NAC) is another option.
RTMS Improves Executive Function in Kids with Schizophrenia and Autism
 Researcher Stephanie Ameis reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that following repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic coil placed over the scalp delivers electric pulses to the brain, children with schizophrenia and autism spectrum disorders showed improvements in executive function, including working memory. The rTMS treatment targeted the left dorsolateral prefrontal cortex.
Researcher Stephanie Ameis reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that following repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic coil placed over the scalp delivers electric pulses to the brain, children with schizophrenia and autism spectrum disorders showed improvements in executive function, including working memory. The rTMS treatment targeted the left dorsolateral prefrontal cortex.
Dopamine Partial Agonists: An Overview
 Several atypical antipsychotic drugs are partial agonists of dopamine. They provide weak stimulation of dopamine receptors in the brain and prevent dopamine from overstimulating the receptors by binding to them in its place.
Several atypical antipsychotic drugs are partial agonists of dopamine. They provide weak stimulation of dopamine receptors in the brain and prevent dopamine from overstimulating the receptors by binding to them in its place.
In contrast, most antipsychotic and antimanic drugs are dopamine antagonists, which also bind to dopamine receptors but prevent any stimulation from occurring there.
A. Aripiprazole (Abilify) was the first partial dopamine agonist approved by the Food and Drug Administration for the treatment of schizophrenia, and mania, and as an add-on treatment to antidepressants for the treatment of unipolar depression, but not bipolar depression.
B. Brexpiprazole (Rexulti) received FDA approval for the treatment of schizophrenia and as an add-on treatment to antidepressants for the treatment of unipolar depression in 2015. It is similar to aripiprazole but has weaker activity at the dopamine D2 receptor. Brexpiprazole is associated with small increases in the hormone prolactin, as opposed to the small decreases in prolactin seen with aripiprazole.
C. Cariprazine (Vraylar) is FDA-approved for schizophrenia and mania, and it also has positive placebo-controlled data in bipolar depression and as an adjunct to antidepressants in unipolar depression. It differs from the others in that it is more potent at dopamine D3 receptors than at D2 receptors. It is thought that effects on D3 receptors may provide better antidepressant effects, but this proposition has not yet been tested.
New Drug Cariprazine Approved for Schizophrenia and Bipolar Disorder
 In late 2015, the Food and Drug Administration approved the new atypical antipsychotic drug cariprazine for the treatment of schizophrenia and mania in adults. The approval followed a series of clinical trials that showed that the drug reduced symptoms of each illness compared to placebo.
In late 2015, the Food and Drug Administration approved the new atypical antipsychotic drug cariprazine for the treatment of schizophrenia and mania in adults. The approval followed a series of clinical trials that showed that the drug reduced symptoms of each illness compared to placebo.
The most common side effects of cariprazine reported in the trials included tremor, slurred speech, and involuntary muscle movements.
Approaches to Restoring Cognition in Unipolar and Bipolar Depression
Many people with bipolar disorder suffer cognitive difficulties, and these may progress as a function of the number of mood episodes they experience. At the 2015 meeting of the International Society for Bipolar Disorders, researcher Eduard Vieta described the importance of directly prescribing diet, exercise, good sleep hygiene, smoking avoidance, and cognitive exercises designed to maintain cognitive reserves in people with bipolar disorder. Vieta stressed that one of the most important approaches to maintaining cognition is to help patients achieve and maintain remission. He also noted that those patients with lithium levels of .6meq/l or greater did not see cognitive deterioration.
Some treatments for bipolar disorder can contribute to cognition problems. Topiramate and benzodiazepines can impair cognition, as can atypical antipsychotic drugs and certain antidepressants that block the neurotransmitter acetylcholine. Avoiding these treatments and those with sedative side effects may also be helpful.
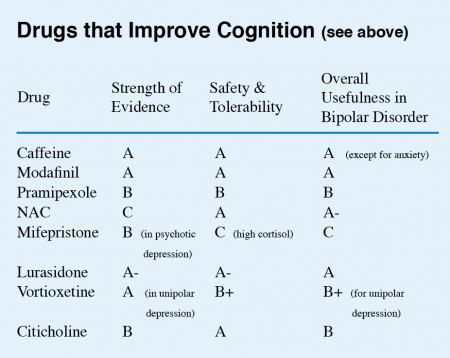
Vieta listed a series of drugs with some promise for improving cognition. (These did not include treatments for dementia, which include memantine and a group of drugs that increase acetylcholine by inhibiting its breakdown.)
This editor (Robert M. Post) has taken the liberty of giving a letter grade (A to D) to each drug on Vieta’s list on the basis of the strength of the data supporting its efficacy, its safety and tolerability, and its overall usefulness for patients with bipolar disorder. These recommendations, like other material in the BNN, are subjective and likely to change as more systematic studies on these treatments are published.