First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed
| October 28, 2022 |
| FEATURED NEWS: First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed Extended-release dextromethorphan HBr-bupropion HCl (Auvelity™), the only oral N-methyl D-aspartate (NMDA) receptor antagonist approved for the treatment of major depressive disorder (MDD), is now available by prescription in the United States, maker Axsome Therapeutics Inc. announced. The drug is supplied in 105-mg tablets in 30-count bottles.On August 18th, 2022, the US Food and Drug Administration (FDA) approved dextromethorphan HBr-bupropion HCl extended-release tablets 45mg/105mg |
Lithium Corrects Circadian Rhythm Abnormalities in Bipolar Depression

At a recent scientific meeting, researcher Monica Federoff described new findings about lithium’s effects in people with bipolar I disorder, especially regarding circadian rhythms. The 12-week study included 386 participants with bipolar I. Some participants responded well to lithium, but even those whose bipolar disorder did not remit saw improvements in total symptoms, depressive symptoms, and manic symptoms.
Only those who were classified as good responders to lithium treatment showed improvement in circadian symptoms. Their depression improved in the direction of more “morningness,” and the authors suggested that “stabilization of circadian symptoms of depression may be an essential feature of lithium’s therapeutic effects in [bipolar] I patients.”
No Association of Benzodiazepines, Z Drugs and Other Anxiolytics with Dementia

Benzodiazepines, so-called Z-drugs (such as zolpidem, zopiclone, and zaleplon), and other anxiolytics are commonly prescribed drugs that have some cognitive side effects. For this reason, there has been concern that the drugs may increase risk of dementia, and small studies had suggested that this might be the case. However, a new large study found no subsequent dementia risk after taking these drugs.
In a 2020 article in the American Journal of Psychiatry, researchers Merete Osler and Martin Balslev Jørgensen described a cohort and nested case-control study of 235,465 adult patients in Denmark in which they found no association of benzodiazepines, Z-drugs, or other anxiolytics with a subsequent diagnosis of dementia. Participants were patients over the age of 20 who were hospitalized for an affective disorder. Of these, 75.9% had been prescribed one of the drugs in question, and 4.2% went on to be diagnosed with dementia.
While participants in this study who had the lowest use of benzodiazepines or Z drugs showed a minimal increased risk of dementia compared to those who took none of these drugs, those who had the highest use of benzodiazepines and Z drugs actually had the lowest incidence of dementia in the study.
The previous studies may have been “confounded by indication” meaning they did not take the underlying psychiatric condition for which the drugs were prescribed into account.
Dr. Post’s Recommendations For Treating Youth with Bipolar Symptoms
Our Editor-in-Chief, Dr. Robert M. Post, shares his personal recommendations for the treatment of children and adolescents with symptoms of bipolar disorder. Remember: Patients and family members must consult a physician about all information conveyed in the BNN. With the exception of lithium, none of the medications or supplements discussed above have been approved by the US Food and Drug Administration for use in children under 10. The findings reported here are in many cases preliminary and cannot be taken as recommendations based on the short summaries provided here. All treatment decisions must be made in conjunction with a patient’s treating physician, who is solely responsible for initiating any treatment discussed in the BNN or elsewhere.
In symptomatic and functionally impaired children, medication is almost always necessary. Many treating psychiatrists would start with an atypical antipsychotic, since there is clear evidence of the efficacy of such treatments. The side effects profile should be considered, as there is a considerable difference in the degree of weight gain associated with different atypical antipsychotics. The largest weight gains occur with olanzapine and clozapine, intermediate gains occur with aripiprazole and quetiapine, and the least gains occur with ziprasidone and lurasidone (and the latter has the advantage of being approved by the US Food and Drug Administration for the treatment of bipolar depression in children who are 10–17 years old). The addition of the diabetes drug metformin to decrease weight gain in people taking atypical antipsychotics is increasingly common.
The addition of an anticonvulsant medication (such as lamotrigine, carbamazepine/oxcarbazepine, or valproate) or the mood stabilizer lithium may be needed, as multiple studies indicate that combination treatment is typically needed in children (as in adults) to achieve a more complete response or remission.
Interestingly, oxcarbazepine was effective in younger but not older children with mania in a previous placebo-controlled study by Karen D. Wagner and colleagues published in the American Journal of Psychiatry in 2006.
Conversely, in a 2015 article in the journal JAACAP, researcher Robert Findling reported that in a placebo-controlled study of lamotrigine, 13–17-year-olds responded better than 10–12-year-olds.
Lithium treatment deserves consideration in children with classical presentations of bipolar disorder and those who have family members who have responded well to lithium treatment.
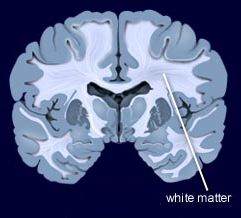
Lithium has the benefit of improving the white matter abnormalities seen in the brains of patients with early-onset bipolar disorder. Hafeman and colleagues reported in a 2019 article that children with bipolar disorder who were treated with lithium had better long-term results upon follow up than those treated with atypical antipsychotics or anticonvulsants.
There is much less scientific consensus about other adjunctive treatments for young people with additional bipolar symptoms and comorbidities, but this editor often uses several. Vitamin D3 is often low in children with psychiatric illness, and may improve mood and cognition.
The antioxidant N-acetylcysteine (NAC) helps depression, anxiety, and irritability, and is effective at treating habit-related behaviors such as trichotillomania (compulsive hair-pulling), obsessive-compulsive disorder (OCD), and drug use, including specifically reducing marijuana use in adolescents. A typical dose is 500–600 mg capsules, one capsule twice a day for one week, then two capsules in the morning and two in the evening thereafter.
Folate or folic acid may enhance antidepressant effects and those of lithium. In patients who have a particular low-functioning variant of a gene known as MTHFR, L-methylfolate is required instead of folate.
The widely-used supplement acetyl-L-carnitine (ALC) is poorly studied in children, but deserves consideration as a supplemental treatment for patients with histories of childhood adversity. In adults with depression, blood levels of ALC may be low, particularly in those with an early onset of bipolar symptoms and a history of childhood adversity (see a 2018 article by Carla Nasca in the journal PNAS). There is a modicum of evidence that ALC produces antidepressant effects in adults. ALC may also sensitize insulin receptors and normalize blood pressure.
There is increasing evidence of the role of inflammation in depression, mania, post-traumatic stress disorder (PTSD), and schizophrenia. Checking for abnormalities in inflammatory markers in the blood (especially Il-6 and CRP) may point the way to appropriate therapy with anti-inflammatory drugs such as minocycline (100 mg twice a day) or celecoxib (200 mg twice a day) in patients who do not respond fully to first-line medications.
Treating Symptoms of Bipolar Disorder in Children at Risk
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported. See previous articles for more on this symposium.
Sub-Threshold Bipolar Disorder or BP-NOS is Impairing and Requires Treatment
In research Danella M. Hafeman’s research, children with BP-NOS were almost as ill as those with bipolar I disorder (BP I) and experienced equal incidence of suicide attempts, substance abuse, other simultaneous psychiatric diagnoses, and functional impairment, clearly indicating that they were in need of treatment. About 50–65% of participants with a family history of bipolar disorder converted from diagnoses of BP-NOS to BP I, while those with BP-NOS and no family history of bipolar disorder converted to BP I at rates of about 30–48%.
Several presenters presented data showing that those with sub-threshold bipolar disorder had severe functional impairment, a high incidence of suicide attempts, and additional diagnoses including ADHD, conduct disorder, anxiety, and substance abuse.
Diagnostic Tool Can Help Identify Children with Bipolar Disorder
Researcher Amy Yule indicated that a tool called the Child Behavior Checklist (CBCL) is effective for making the diagnosis of conduct disorder in children with bipolar disorder, while researcher Joseph Biederman showed that the CBCL can also identify children with bipolar I disorder and is faster and simpler to use in clinical practice than are full structured diagnostic interviews.
Researcher Janet Wozniak found that there was a high incidence of bipolar disorder in first-degree relatives of children with sub-threshold bipolar disorder, suggesting the validity of identifying youth with sub-threshold bipolar symptoms.
As discussed above, there is also a high incidence of children with BP-NOS progressing to a full diagnosis of bipolar I or II disorder (as many as 50% of those with a family history of bipolar disorder). However, the point is not to wait for the negative effects of a full diagnosis before beginning treatment: BP-NOS itself requires treatment.
Discussion and Emerging Consensus on Treatment, Particularly of BP-NOS
Experts in the field agree that family focused therapy (FFT) or its equivalent is a crucial first step to treatment of depression, cyclothymia (cycling between depressive and hypomanic symptoms that do not meet the threshold for a diagnosis of bipolar disorder), and BP-NOS in children who are at high risk of bipolar disorder because they have a parent with the disorder.
A second area of agreement is that young people with BP-NOS should have a positive therapeutic coach (which could be a treating physician if no other person is available), who can emphasize important early steps that can improve short- and long-term health. These include maintaining a healthy diet, exercise (such as participation in school sports), the practice of mindfulness and/or meditation, and playing and practicing a musical instrument. Parental support is also critical to decreasing negative expressed emotion.
Early interventions and wellness programs that focus on these factors are part of the successful Vermont Family Based Approach, led by psychiatrist Jim Hudziak, Director of the Vermont Center for Children, Youth, and Families. Since programs like these are not widely available, treating physicians must create their own teams to provide such encouragement, and teach families how to find or establish such a support network.
School teachers should be engaged in support of the treatment of a child with bipolar disorder. Teachers should pay special attention to behavioral symptoms of an ill child. It also may be important for physicians to connect directly with teachers to ensure that children recovering from an episode of bipolar disorder receive extra time for assignments, a decreased academic burden, and other support. Researcher Manon H. Hillegers indicated that intervention by a physician will likely be listened to and believed, while parental requests alone to teachers or to the school may go ignored.
Hillegers, like researcher Lakshmi Yatham and colleagues, have found that it takes a year after a first manic episode for a child’s cognition to return to normal, so that special allowances should be made for such students even many months after they have recovered from their mania.
Positive Effects of a Brief Session of Aerobic Exercise for Sedentary Children
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Benjamin I. Goldstein reported that a single 20-minute session of aerobic exercise (achieving 70% of maximal heart rate) was associated with improvement in cognition and in abnormalities seen on brain imaging in young people. Goldstein urged clinicians to do motivational interviews with sedentary children in their care, emphasizing the positive cardiovascular and cognitive effects of exercise. He indicated this would be more effective than a focus only on weight loss, which is much more difficult to achieve.
Family Focused Therapy Effective in Youth at Risk for Bipolar Disorder Who Have Early Symptoms
 Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, Miklowitz reported findings from recent studies of youth who were at high risk for bipolar disorder because of a family history of the illness and the presence of early symptoms such as depression or cyclothymia or bipolar not otherwise specified (BP-NOS). Family focused therapy reduced symptoms. It also slowed onset of a first episode of mania and slowed the conversion to a diagnosis of bipolar I or bipolar II. These results converge with a total of 10 other positive studies of family focused therapy in different populations in children and adults. FFT or its equivalent should be made available to all symptomatic children who are at risk for bipolar disorder because of a family history of the disorder.
Potential Problems when Youth at Risk for Bipolar Disorder Take SSRIs
 At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
Quetiapine Reduced Childhood Mania, Especially in Those with Thicker Frontal Temporal Regions
 In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
In contrast, other researchers have found lithium superior to quetiapine. Vivian Kafantaris showed that patients who respond well to lithium show improvements in white matter abnormalities. Michael Berk and colleagues found that a year on lithium was superior to quetiapine on all measures including cognition and brain imaging in patients having their first episode of mania.
Lithium Effective for Maintenance Treatment of Childhood-Onset Bipolar Disorder
Evidence has been accumulating that lithium is effective in the treatment of young people with bipolar disorder. In a study by Robert Findling and colleagues published in the Journal of the American Academy of Child and Adolescent Psychiatry in 2018, participants aged 7–17 who responded well to lithium during a 24-week study were then randomized to receive either lithium continuation (17 participants) or placebo (14 participants) for 28 more weeks.
Those who continued lithium treatment were more likely to stay in the study. Participants who discontinued the study mostly reported that they did so due to re-emergence of their mood symptoms (mostly in the placebo group).
Lithium was well-tolerated and was not associated with any more weight gain than placebo. This study adds to the growing literature on the effectiveness and tolerability of lithium both acutely and in maintenance treatment in childhood bipolar disorder.





