Dark Chocolate May Have Some Health Benefits
Very dark chocolate made mostly from cocoa beans may be good for you. Cocoa is high in flavanols, which belong to a class of antioxidants called flavonoids. Dark chocolate has been associated with lowered risk of heart attack and stroke, improvements in cognition, lower body mass index (BMI, a weight to height ratio), dilation of blood vessels and lower blood pressure, and improved cholesterol profiles. This is despite containing a lot of saturated fat (a good trick, indeed). Among a study of 37,000 Swedish men, individuals who ate at least 1.8oz of dark chocolate a week had a 17% lower risk of stroke than those who ate less than 0.4oz a week.
Moderation is important. Two ounces of dark chocolate contain about 440 calories, so while a little may be good, a lot may not be so good. Watch out for milk chocolate and highly processed chocolates with great quantities of sugar added, they contain more calories and fewer health benefits.
A balanced diet and regular exercise are keys to good health, but don’t feel too badly if you top off a balanced meal with a tantalizing piece of the dark stuff.
Short Telomeres, More Depressions, and Risk of the Common Cold
 Too many depressions in unipolar and bipolar disorder are associated with multiple risks. These include social and employment losses, dysfunction and disability, cognitive dysfunction, reduction in hippocampal volume (in unipolar depression), increases in medical comorbidity, increased risk of cardiovascular disease, and endocrine abnormalities (see the 2012 article by this author Post et al. in the Journal of Psychiatric Research).
Too many depressions in unipolar and bipolar disorder are associated with multiple risks. These include social and employment losses, dysfunction and disability, cognitive dysfunction, reduction in hippocampal volume (in unipolar depression), increases in medical comorbidity, increased risk of cardiovascular disease, and endocrine abnormalities (see the 2012 article by this author Post et al. in the Journal of Psychiatric Research).
To this list we can now add short telomeres. Telomeres sit at the end of DNA strands and shorten with each cell replication. A person’s percentage of short telomeres increases with aging. The number of depressions a patient with bipolar II disorder has had is also associated with a higher percentage of short telomeres. The magnitude of the difference in telomeres is equivalent to 10 years of aging.
An article by Cohen et al. published by the Journal of the American Medical Association (JAMA) in 2013 suggests that short telomeres can even be linked to increased vulnerability to viral infections causing the common cold. Depression has also been linked to various immune deficiencies. Whether direct alteration in immune function is responsible or whether this is mediated via telomere length remains to be determined.
Editor’s Note: The moral of this story is that patients should stay on effective treatment long-term to prevent depression in the recurrent affective disorders. This means antidepressants for unipolar depression, and mood stabilizers and atypical antipsychotics for bipolar depression. Prevent depressions and protect your brain and your telomeres (and as a bonus, you may not get so many colds).
Gap in Life Expectancy Between Psychiatric Patients and the General Population Grows
A study published by Lawrence et al. in the journal BMJ in 2013 suggests that the gap in life expectancy between psychiatric patients and the general population is widening. This was due more to poor physical health than to suicide.
Investigators at the University of Western Australia in Perth found that within that geographic region, the gap in life expectancy for males with all mental disorders combined compared to males in the general population increased from 13.5 years in 1985 to 15.9 years in 2005. For females, the gap increased from 10.4 years in 1985 to 12.0 years in 2005.
Editor’s Note: Data from the US suggest even greater loss of years of life expectancy in those with serious mental illnesses. In the best case, in Virginia patients lost an average of 13 years of life expectancy compared to the general population, while in some western states up to 28 years of life expectancy was lost by the average patient.
Cardiovascular disease is one of the biggest contributors to these almost unbelievable statistics. It is possible that short telomeres resulting from stressors, episodes of depression, abused substances, and a variety of poor lifestyle factors such as smoking and lack of exercise also contribute to this huge deficit in longevity. Other factors that can co-occur with bipolar illness, such as inflammation, high cortisol, and oxidative stress, are likely problematic as well.
Telomere Length Important for Health
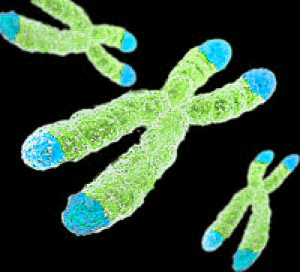 Elizabeth Blackburn (who won the Nobel Prize for medicine in 2009) gave a spectacular plenary lecture at the 2013 meeting of the American Psychiatric Association, in which she described the role of telomeres in psychiatric and other medical disorders. Telomeres are the strands of DNA at the end of each chromosome that protect the integrity of the DNA each time the cell replicates. The end is capped to prevent damage, degeneration, and genetic instability. A minimum length must be maintained for the protection of the cells.
Elizabeth Blackburn (who won the Nobel Prize for medicine in 2009) gave a spectacular plenary lecture at the 2013 meeting of the American Psychiatric Association, in which she described the role of telomeres in psychiatric and other medical disorders. Telomeres are the strands of DNA at the end of each chromosome that protect the integrity of the DNA each time the cell replicates. The end is capped to prevent damage, degeneration, and genetic instability. A minimum length must be maintained for the protection of the cells.
Telomeres shorten with aging and with each cell replication. They also shorten as a function of childhood adversity, stressors in adulthood, and number of episodes of depression. When a cell’s telomeres get too short, the cell enters a period of senescence, meaning it no longer replicates. Senescence is associated with a variety of adverse events, including the possibility of apoptosis (cell death), pro-inflammatory effects, and pro-tumor effects. The cell can begin to resemble a rotten apple that spreads its ill effects to others nearby. These effects can predispose a person to diseases such as diabetes, depression, attention deficit hyperactivity disorder (ADHD), anxiety disorders, pulmonary fibrosis, aplastic anemia, cardiovascular disorders (stroke and heart attack), osteoarthritis, immune abnormalities, dementia (in women), and premature aging.
Certain lifestyle alterations can increase telomere length, such as mindfulness/yoga training, exercise, sleep, omega-3 fatty acids, and having a positive purpose or meaning in life. Telomeres can also be lengthened by a synthetic enzyme called telomerase.
Other lifestyle factors can shorten telomeres or make telomerase less effective. Chronic stress can decrease the activity of telomerase by 50%. For people serving as the caregiver of a loved one, the longer the duration of this stress, the shorter the length of telomeres. High levels of what Blackburn described as cynical hostility also decrease telomere length.
Editor’s Note: Here we have more evidence that stress can affect our genes. We have written before about epigenetics, the study of the process by which environmental events such as stress can leave behind methyl and acetyl groups on DNA and histones that affect how easily DNA is turned on or off. Now it seems that stress can also have profound effects on the telomeres that cap each strand of DNA and keep it stable. An overly high proportion of short chromosomes is associated with a range of psychiatric and medical illnesses. This type of non-hereditary influence on genes could mediate some of the long-term effects of the environment on health. The good news for patients with bipolar disorder is that M. Schalling et al. found that treatment with lithium lengthened telomeres. Perhaps the bottom line of this whole collection of fascinating data is: Take good care of your telomeres, and they will take care of you.
Higher Levels of Caffeine in Blood May Be Associated With Lower Likelihood of Dementia
Alzheimer’s disease and other kinds of dementia can be devastating. Researchers are looking for treatments and lifestyle choices that may prevent, slow, or lessen the likelihood of serious dementia. Some epidemiological research in humans and other studies of animals has suggested that consumption of coffee or caffeine may help protect against the development of Alzheimer’s disease. A 2012 study by Arendash et al. published in the Journal of Alzheimer’s Disease sought to clarify the connection between coffee and cognitive status. The researchers also collected data on biomarkers in blood.
In patients with mild cognitive impairment, those patients whose blood levels of caffeine were 1200 ng/mL or higher (an amount that would result from drinking 3–5 cups of coffee daily) did not develop dementia during the following two to four years, while half of those whose blood levels of caffeine were below this threshold did. Moreover, those patients who had mild cognitive impairment at the beginning of the study had lower levels of caffeine than those who had normal cognitive functioning at that time.
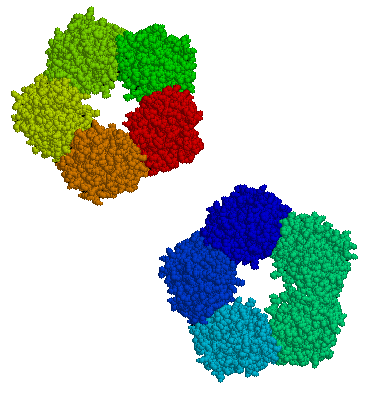
Patients with mild cognitive impairment who later developed dementia had low levels of three biomarkers in their blood—the neurotrophic factor granulocyte colony-stimulating factor (G-CSF), the anti-inflammatory cytokine IL-10, and the pro-inflammatory cytokine IL-6. This suggests that low levels of these biomarkers may be an indicator of impending Alzheimer’s disease. G-CSF, in particular, has shown beneficial effects on cognition in mice.
Since half of patients with lower levels of caffeine did not develop dementia, it is clear that caffeine is far from being the only factor that could affect cognitive functioning. Arendash suggested that other factors may include levels of cognitive and physical activity, hypertension (high blood pressure), and antioxidant intake, especially from fruits and vegetables.
Editor’s Note: This study of caffeine was not randomized and is subject to other interpretations. For example, people who drink less coffee may have more hypertension, which is associated with dementia risk. However, the study does raise the possibility that caffeine could have positive effects on the brain (especially if it does not make a patient anxious or insomniac).
The caffeine findings are also supported by studies of dementia in mice. Long-term administration of caffeine to these animals resulted in a similar biomarker profile and prevented cognitive impairment.
Other treatments may also be useful in preventing cognitive decline. In BNN Volume 16, Issue 5 from 2012, we wrote about a one-year prospective study published by Forlenza et al. in the British Journal of Psychiatry in 2011 that showed that lithium at the small dose of 150mg per day reduced the rate of cognitive decline in those with mild cognitive impairment compared to placebo.
BDNF Is Decreased in Depression and Mania
Brain-derived neurotrophic factor (BDNF), which protects neurons and is necessary for long-term memory, can be measured in blood. In a symposium on bipolar disorder at the 2012 meeting of the Society of Biological Psychiatry, researcher Flavio Kapsczinski reviewed evidence from several meta-analyses showing that low levels of BDNF in the blood correlate with severity of an episode of depression or mania. In addition to the findings that BDNF levels are low during a mood episode, there are other reliable biomarkers of illness, including increases in intracellular calcium, increases in cortisol and failure to suppress cortisol by dexamethasone, and a variety of indices of inflammation and oxidative stress.
There are several common variants of the gene responsible for the production of BDNF, depending on which types of amino acids appear in its coding—valine or methionine. The Val66Val allele of proBDNF is the most frequently occurring in the population, and is the best-functioning variant. Those with a methionine substitution (Val66Met or Met66Met) have less efficient forms of BDNF. Researcher Jair Soares reported that the Met allele was associated with deficits in declarative memory in patients with bipolar disorder, and was also associated with smaller volume of the anterior cingulate gyrus.
Researcher Ghanshyam N. Pandey reported that patients with pediatric or adult bipolar disorder had decreased BDNF protein and mRNA levels in platelets and lymphocytes compared to controls. Treatment significantly increased these BDNF levels in the pediatric, but not in the adult bipolar subjects. These measurements in blood are consistent with findings that there are decreases in BDNF in the hippocampus and prefrontal cortex of patients who died while depressed or who committed suicide compared to controls.
CRP in Blood Predicts Onset of New Episode in Childhood Mood Disorders
At the 2013 meeting of the International Society for Bipolar Disorders, researcher Barbara Gracious presented evidence that increased levels of high sensitivity c-reactive protein (hsCRP), a marker of inflammation, were associated with an increased risk for developing a full-blown mood episode in 71 youth (average age 13.8) participating in a study called Longitudinal Assessment of Manic Symptoms (LAMS-2). The children were selected for the study because they had manic symptoms that were not severe enough to meet criteria for a diagnosis of bipolar I or II disorder. This research has not yet been published in a peer-reviewed journal, but the abstract can be found in first 2013 supplement of the journal Bipolar Disorders (page 67).
CRP levels are also known to predict cardiovascular disease and Type II diabetes.
Levels of 25-OH vitamin D, TNF?, and IL-6 did not predict a later mood disorder.
Editor’s Note: These data suggest the importance of assessing CRP and other markers in youth who are either prodromal (having early symptoms of a mood disorder) or at high risk because of a family history of a mood disorder.
The next step for clinical research would be to determine what treatment might decrease CRP and whether it would also prevent the development of mood episodes.
Inflammatory Markers May Predict Antidepressant Response
There appears to be a link between inflammation and depression. In the journal Neuropsychopharmacology, Cattanes et al. reported in 2013 that compared to controls, depressed patients had significantly higher baseline levels of inflammatory cytokines, less glucocorticoid receptor function, less neuroplasticity, and fewer neuroprotective factors. Certain variables predicted response to treatment, others were seen only in responders, and still others changed in everyone with antidepressant treatment.
Higher baseline levels of inflammatory markers interleukin IB, macrophage inhibitory factor (MIF), and tumor necrosis factor TNF? were each associated with nonresponse to antidepressant treatment, and the three combined accounted for 50% of the variance in response—that is, they were the major predictor of whether a patient responded to treatment.
Levels of other factors changed in only those patients who responded well to antidepressants. The biggest changes were the normalization in levels of the neurotrophic factors BDNF and VEGF.
Several other markers normalized with antidepressant treatment regardless of whether the patients responded to treatment, and these included decreases in cytokines interleukin-IB and MIF and improved glucocorticoid receptor function.
The three different kinds of findings about these biomarkers were observed regardless of what type of antidepressant was used—SSRI versus tricyclic nortriptyline (which blocks norepinephrine reuptake).
Editor’s Note: This study replicates other studies in depression where signs of inflammation have been observed, including increases in inflammatory cytokines, decreases in glucocorticoid receptor function (needed to suppress high levels of the stress hormone cortisol) and lower levels of neuroplasticity and neuroprotection markers. This, however, is one of the first studies to show that levels of these markers at baseline may predict response to antidepressant treatment.
Also novel are the findings that while some high interleukin levels at baseline predicted antidepressant non-response, other ones normalized only in responders, and still others changed with treatment independent of whether the patients’ depression improved. These exciting findings require replication, but suggest the future possibility of personalized medicine, that is, choosing medications based on an individual biochemical marker profile. Eventually direct use of anti-inflammatory agents may be necessary in those with the highest levels of cytokines (predicting non-response to conventional antidepressant treatment). The same types of studies are needed in bipolar depression to determine the relationship between these inflammatory markers and treatment response.
Immune Mechanisms Are Important to the Emergence of Defeat Stress–Induced Depressive Behaviors
At a recent scientific meeting, researcher Georgia E. Hodes presented evidence that in mice, the immune system may play a role in behaviors that resemble human depression. Repeated social defeat stress (when an intruder mouse is threatened by a larger mouse defending its territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit social avoidance and lose interest in sucrose. Hodes et al. determined that interleukin 6 (IL-6), an inflammatory cytokine, or signaling molecule, secreted into the blood was crucial to these behaviors. When the researchers injected mice with antibodies that block the effects of IL-6, or when they irradiated the mice’s peripheral immune system to prevent the formation of IL-6, the depressive behaviors did not emerge following defeat stress.
Editor’s Note: There are increasing data that immunological and inflammatory mechanisms play a role in human affective disorders, and these preliminary data raise the possibility that blocking some immune mechanisms more directly in humans could be a novel therapeutic approach to explore in the future.
In Veterans, PTSD Is Associated With Autoimmune Illnesses
At a recent scientific meeting, Thomas Neylan and colleagues reported that post-traumatic stress disorder (PTSD) may be connected to autoimmune illnesses. In this study, 673,277 veterans of the US military who had served in Iraq and Afghanistan were screened for the development of PTSD. The illness was diagnosed in 31% of the veterans, and those individuals had a higher incidence of autoimmune-related disorders including thyroiditis, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, and systemic lupus erythematosus. Neylan’s research group specifically examined those whose disorders developed after the onset of the PTSD, and found that the statistical relationship between their illnesses and PTSD was strong. However, the researchers also found that there was evidence of a similarly strong relationship in the other direction: veterans who were first diagnosed with some of these same autoimmune difficulties also went on to develop PTSD.
Many previous clinical and preclinical studies have linked altered immune and autoimmune mechanisms to severe stressors such as those that are involved in PTSD. This is the first study to unequivocally demonstrate the relationship in an extraordinarily large number of patients.
Editor’s Note: These findings resemble those that suggest that among the general population, childhood adversity is associated with an increased incidence of a variety of medical disorders in adulthood. Similarly, in the Bipolar Collaborative Network in which this editor (Post) is an investigator, we found that a history of childhood adversity in patients with bipolar disorder was associated with an increased incidence of a variety of medical illnesses in adulthood, including some related to immune and autoimmune function.
More research that would measure inflammatory markers in PTSD and mood disorders is needed. It would also be important to ascertain whether treatment of mood disorders and PTSD reduces the risk of autoimmune disorders.