Brain Growth in Infancy Predicts Autism
A 2017 article in the journal Nature suggests that brain scans during infancy can predict which kids at risk for autism will go on to develop the disorder, leading to earlier treatment. Studies have shown that children with autism have enlarged brains. The new research zeroes in on the time period when this overgrowth occurs.
Researcher Heather Cody Hazlett and colleagues used magnetic resonance imaging (MRI) scans to measure brain growth in 106 high-risk infants with siblings who have autism spectrum disorder and 42 infants at low risk. The scans were performed when the infants were 6 months, 12 months, and 24 months old.
In 15 infants diagnosed with autism at 24 months, the researchers saw hyperexpansion of cortical surface area between 6 and 12 months and brain overgrowth between 12 and 24 months. The overgrowth coincided with symptoms of autism appearing, and with symptom severity.
The reseachers were able to create a computer algorithm that could predict whether an infant would develop autism based on images of brain growth. The algorithm corrected predicted autism 81% of the time.
Studies have suggested that starting interventions to treat autism early provides the best benefits, so using MRI to diagnose or predict autism before symptoms appear might allow for even earlier treatment that could be more effective.
The study also identified the sites of unusual brain development, which may help researchers determine what mechanisms lead to brain overgrowth in autism and eventually develop treatments that prevent these changes.
Study of Baby Teeth Links Autism and Exposure to Heavy Metals Such as Lead
Recent research has revealed that autism is linked to new onset genetic mutations (called ‘de novo’ mutations) that occur during early fetal development. A new study suggests that levels of heavy metals such as lead and zinc (but not mercury) may affect the likelihood that these mutations will occur.
The 2017 study by Manish Arora and colleagues in the journal Nature Communications included twins with and without autism, particularly twin pairs in which one twin had autism and the other did not. An international team of scientists collected naturally shed baby teeth from the twins. The researchers then used lasers to extract specific layers of dentine, the hard substance beneath tooth enamel, which correspond to different developmental periods, including before birth and in early childhood. The researchers then analyzed these dentine samples to determine the children’s uptake of various heavy metals in early life.
The analysis showed that children with autism had higher levels of lead (a neurotoxin) throughout development, but particularly right after birth. Children with autism also had lower uptake of manganese, an essential nutrient. Compared to children without autism, children with autism had lower zinc levels in utero, but higher zinc levels after birth. Zinc is another essential nutrient. Lead and manganese levels were also linked to autism severity.
The method of analyzing teeth allows researchers to look back in time and measure what children were exposed to years earlier. This may help identify environmental factors that contribute to autism spectrum disorders.
Autism Linked to Banned Chemicals
 An explanation for the increase in autism rates over the past few decades has remained elusive in the years since researcher Andrew Wakefield fabricated a link between the disorder and mercury in vaccinations that was eventually completely debunked.
An explanation for the increase in autism rates over the past few decades has remained elusive in the years since researcher Andrew Wakefield fabricated a link between the disorder and mercury in vaccinations that was eventually completely debunked.
In 2016, researcher Kristin Lyall of Drexel University’s A.J. Drexel Autism Institute published findings suggesting that high exposure during pregnancy to chemicals banned in the 1970s increased risk of an autism spectrum disorder.
The study looked at 1144 children born in southern California between 200 and 2003. Their mothers had participated in California’s Expanded Alphafetoprotein Prenatal Screening Program, intended to identify birth defects during pregnancy. Second trimester blood samples from these women could be used to determine to what extent their children were exposed to the chemicals while in utero. The researchers found an association between the highest exposure levels and later autism diagnoses.
Lyall and colleagues measured levels of two different classes of organochlorine chemicals: polychlorinated biphenyls (PCBs), used as lubricants, coolants, and insulators; and organochlorine pesticides (OCPs), including DDT, which was banned in 1972. All production of organochlorine chemicals was banned in the US in 1977, but they remain in the environment and are absorbed in the fat of animals that humans eat. According to Lyall, people in the US generally have detectable levels of organochlorine chemicals in their bodies.
The study revealed that exposure to two compounds in particular—PCB 138/158 and PCB 153—was linked to dramatically higher autism rates. Level of exposure is key to autism risk. Those children in the top 25 percentile of exposure were 79% and 82% more likely to have an autism diagnosis than those with the lowest levels of exposure, respectively.
High exposure to two other compounds, PCB 170 and PCB 180, increased autism risk by 50%.
The findings by Lyall and colleagues were published in the journal Environmental Health Perspectives.
Editor’s Note: Another study by Manish Arora and colleagues links autism risk to levels of lead, zinc and manganese absorbed in early life.
The myth that mercury in vaccines causes autism still lingers in our popular culture. Mercury is no longer used in vaccines, but autism rates are still increasing. Perhaps the new findings of a link between heavy metals and autism will help end the misinformation about the safety of vaccines and allow more parents to vaccinate their children without worry.
Offspring of Bipolar Parents Have More Psychiatric Illness
 A 2017 study from the Czech Republic found that children and adolescents with at least one parent with bipolar disorder had much higher lifetime rates of mood and anxiety disorders than their peers who did not have a parent with bipolar disorder. The offspring of bipolar parents also had lower quality of life, less social support, poorer self-perception, poorer relationships with their peers and parents, and more difficult home lives than those whose parents did not have bipolar disorder.
A 2017 study from the Czech Republic found that children and adolescents with at least one parent with bipolar disorder had much higher lifetime rates of mood and anxiety disorders than their peers who did not have a parent with bipolar disorder. The offspring of bipolar parents also had lower quality of life, less social support, poorer self-perception, poorer relationships with their peers and parents, and more difficult home lives than those whose parents did not have bipolar disorder.
The study by Michal Goetz and colleagues in the Journal of Child and Adolescent Psychopharmacology reported that 86% of the children of bipolar parents would be diagnosed with a psychiatric disorder in their lifetime. Similarly, David Axelson and colleagues from the Pittsburgh Bipolar Offspring Study reported in the American Journal of Psychiatry in 2015 that 74.2% of children with a parent with bipolar disorder would receive a lifetime psychiatric diagnosis, and a 2006 study by Myrna M. Weissman in the American Journal of Psychiatry found that the offspring of a unipolar depressed parent were three times more likely to have a psychiatric illness than offspring of nondepressed parents over 20 years of follow-up. Another study by this editor (Robert M. Post) and colleagues in the Bipolar Collaborative Network published in the Journal of Affective Disorders in 2016 found that a third of children at high risk due to a parent’s bipolar diagnosis would go on to have a psychiatric illness.
The Goetz study included a total of 86 participants between the ages of 7 and 18. Half had a parent with bipolar disorder and half did not. One limitation of the study was its recruitment procedure. Parents with bipolar disorder who enrolled their children in the study may have done so out of concern for their offspring’s mental health, increasing illness rates in the group with bipolar parents. Researchers were also aware of parents’ diagnoses, which may have affected their ratings of the young people’s symptoms. Despite these limitations, the study and its predecessors still suggest that psychiatric illness in a parent puts children at very high risk for a psychiatric illness themselves and can affect their wellbeing in a variety of ways.
Goetz and colleagues suggest that there is a need for proactive and complex care of families with psychiatric illness. They suggest that good communication is needed between adult and youth psychiatric services, with physicians who treat adults with bipolar disorder inquiring about those patients’ children and referring them to specialized psychiatric services for youth.
Editor’s Note: I not only endorse the conclusions of Goetz and colleagues, but would further recommend that parents with a diagnosis of bipolar disorder or unipolar depression discuss their children’s mood and behavior with their own psychiatrists and the children’s primary care physicians.
Parents of children aged 2 to 12 may enroll in our own Child Network, a secure online portal where they can record weekly ratings of their children’s symptoms and share these with their physicians.
There are many effective psychotherapeutic interventions for children with anxiety and mood disorders that should be sought for a child with symptoms that impair his or her functioning. Two evidence-based treatments are Family Focused Therapy, which incorporates family members into treatment so that they better understand the illness and can be supportive of the affected child, and cognitive behavioral therapy, in which negative patterns of thoughts and behaviors are challenged and patients are taught more effective problem-solving skills. When childhood psychiatric illness is recognized and treated appropriately, the results are often excellent, and it is possible that heading off the illness early may even prevent the development of more severe illness later in the child’s life.
Short Telomeres Associated with Family Risk of Bipolar Disorder
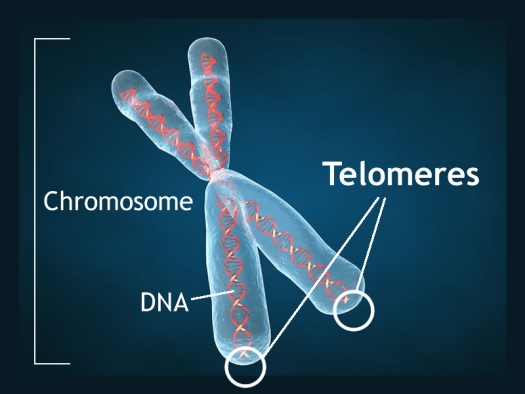
Telomeres are bits of genetic material at the end of each strand of DNA that protect chromosomes as they replicate. Short telomeres have been linked to aging and a variety of medical and psychiatric diseases. Stress and depressive episodes can shorten telomeres, while treatment with lithium can lengthen them.
Telomere length is a heritable trait, and a 2017 study by researcher Timothy R. Powell and colleagues suggests that shorter telomeres are a familial risk factor for bipolar disorder.
The study, published in the journal Neuropsychopharmacology, compared the telomere lengths of 63 people with bipolar disorder, 74 of their immediate relatives (49 of whom had no lifetime psychiatric illness, while the other 25 had a different mood disorder), and 80 unrelated people with no psychiatric illness. The well relatives of the people with bipolar disorder had shorter telomeres than the unrelated healthy volunteers.
Relatives (both well and not) and people with bipolar disorder who were not being treated with lithium both had shorter telomeres than people with bipolar disorder who were being treated with lithium.
Another finding was that longer telomeres were linked to greater volume of the left and right hippocampus, and improved verbal memory on a test of delayed recall. This study provides more evidence that taking lithium increases the volume of the hippocampus and has neuroprotective benefits for people with bipolar disorder.
Traumatic Events in Childhood Linked to Shorter Telomeres
Telomeres are bits of DNA at the end of chromosomes that protect the DNA as it replicates. Shorter telomeres have been linked to aging and increases in multiple types of medical and psychiatric disorders. A 2016 article in PNAS, the Proceedings of the National Academy of Sciences of the United States of America, reported that cumulative life adversity and particularly stressful or traumatic events in childhood, predict shorter telomere length.
The study by Eli Puterman and colleagues included 4,590 individuals from the US Health and Retirement Study who reported stressful events that had experienced. A single experience of adversity was not linked to short telomeres, but lifetime cumulative adversity predicted 6% greater odds of having shorter telomeres. This result was mainly explained by adversity that occurred in childhood. Each stressful or traumatic event in childhood increased the odds of short telomeres by 11%. These were mostly social or traumatic experiences rather than financial stresses.
Hormone Replacement With Estrogen/Progestogen Combo Increases Breast Cancer Risk More Than Once Thought
A 2016 article in the British Journal of Cancer suggests that previous studies underestimated breast cancer risk in women who received hormone replacement therapy with the combination of estrogen and progestogen. The article by researcher Michael E. Jones and colleagues reported that combined hormone replacement therapy could increase the risk of breast cancer by more than three times, depending on how long a woman is exposed to the therapy. The longer the duration of use, the greater the risk of breast cancer. In the study, women who used other types of hormone replacement therapy, such as estrogen only or tibolone, did not have drastically higher rates of breast cancer than had been reported before.
Jones and colleagues suggest that previous studies did not use long enough follow-up periods to track whether women developed breast cancer while using hormone replacement. Their own study is based on a United Kingdom dataset known as the Breakthrough Generations Study. Study participants completed questionnaires at 2.5 years after recruitment, again at around 6 years, and again around 9.5 years. At the time of recruitment, women using combination hormone replacement therapy had been doing so for a median of 5.5 years.
Women who used combination hormone replacement therapy for 5.4 years were 2.74 times likelier to have breast cancer than those who didn’t receive hormone replacement. Using the combined therapy for more than 15 years increased risk 3.27 times compared to non-users.
The study also reported that as body mass index increased, breast cancer risk increased, regardless of hormone use.
While the study by Jones and colleagues was large (39,183 participants), the number of women who took combined hormone replacement and developed breast cancer was still fairly small (52). Seven of the 52 had taken the combined pill for more than 15 years. One limitation of this study is that these seven women may have skewed the risk assessments somewhat.
Experts suggest that women balance the possible risks and benefits of hormone replacement therapy. The therapy can be helpful in reducing symptoms of menopause, particularly hot flashes.
Using the lowest effective dose for the shortest time possible may be the best option. The increased risk of breast cancer drops after a woman stops using hormone replacement.
Women with History of Depression 20 Times More Likely To Have Postpartum Depression
 A study of almost all women who gave birth in Sweden between 1997 and 2008 reports that women with a history of depression are 21.03 times more likely to suffer from postpartum depression than those without such a history. The 2017 article by Michael E. Silverman and colleagues in the journal Depression and Anxiety reports that advanced age and gestational diabetes also increased the likelihood of postpartum depression.
A study of almost all women who gave birth in Sweden between 1997 and 2008 reports that women with a history of depression are 21.03 times more likely to suffer from postpartum depression than those without such a history. The 2017 article by Michael E. Silverman and colleagues in the journal Depression and Anxiety reports that advanced age and gestational diabetes also increased the likelihood of postpartum depression.
Whether a woman had gone through a depression in the past also affected her other risk factors for postpartum depression. Among women who had been depressed before, having diabetes before pregnancy and having a “mild” pre-term delivery were risk factors for postpartum depression. In contrast, among women with no history of depression, young age, having an instrument-assisted or caesarean delivery, and “moderate” pre-term delivery were risk factors for postpartum depression.
Rates of postpartum depression decreased one month after delivery.
Editor’s Note: About one in five women in the general population experience postpartum depression. All new mothers should be screened for postpartum depression, but especially those with a history of depression. Instituting supportive measures may help prevent an episode.
Following Collisions, High School Football Players with No Signs of Concussion May Still Have Neurological Impairment
In a small 2014 study in the Journal of Neurotrauma, researcher Thomas M. Talavaga and colleagues reported that repeated head trauma that did not produce concussion symptoms was still associated with neurocognitive and neurophysiological changes to the brain in high school football players.
The longitudinal study tracked ‘collision events’ experienced by 11 teens who played football at the same high school. The young men also completed neurocognitive testing and magnetic resonance imaging (MRI) scans of their brains over time.
The researchers expected to see the participants fall into two categories: those who had no concussions and normal neurological function, and those who had at least one concussion and subsequent neurological changes. They ended up observing a third group: young men who had not exhibited concussion symptoms, but nonetheless had measurable changes to their neurological functioning, including impairments to visual working memory and altered activation of the dorsolateral prefrontal cortex. Young men in this last group had had more collisions that impacted the top front of the head, directly above the dorsolateral prefrontal cortex.
The authors suggest that the discovery of this third category mean that some neurological injuries are going undetected in high school football players. The players who are injured in this way are not likely to seek treatment, and may continue playing football, risking more neurological brain injury or brain damage with subsequent collisions.
Dutch Study Links Low Vitamin D to Bipolar Disorder
A 2016 study in the Netherlands found that people with bipolar disorder are more likely to have vitamin D deficiency than the general population. Vitamin D deficiency has been linked to other psychiatric disorders including schizophrenia and unipolar depression. Poor diet and lack of exposure to sunlight can put someone at risk for vitamin D deficiency.
The study, led by Remco Boerman and published in the Journal of Clinical Psychopharmacology, included 118 adults with bipolar disorder, 149 with schizophrenia, and 53 with schizoaffective disorder. More than 30% of these participants had deficient levels of vitamin D. Only 15% had optimum levels of the vitamin. More than 22% of the participants with bipolar disorder were deficient in vitamin D, while close to 35% of those with schizophrenia and schizoaffective disorder were deficient.
Study participants had vitamin D levels that were 25% lower than those of the white Dutch population, and vitamin D deficiency was 4.7 times more common in those with psychiatric disorders than the general Dutch population.
The authors suggested screening people with bipolar disorder, schizophrenia, and schizoaffective disorder for low levels of vitamin D.