Cognitive Behavioral Prevention Program Can Reduce Incidence of Depression Among Teens
Adolescents whose parents have a history of depression are at greater risk for depression themselves. A new study suggests that a cognitive-behavioral prevention program aimed at these teens can reduce depression rates compared to the usual care.
The study, by David A. Brent and colleagues in the journal JAMA Psychiatry, included 316 participants aged 13–17, each of whom had a parent with a current or prior depression. Half of the participants participated in the cognitive-behavioral prevention program in addition to usual care initiated by their families. The program consisted of 8 weeks of 90-minute group sessions focused on developing positive thinking habits and improving problem solving, followed by six monthly sessions. The training was based on the Adolescents Coping with Depression program described in a June 2009 JAMA article by Garber et al.
The group who participated in the prevention program had a lower incidence of depression than the group who received only the usual care, and this difference persisted over six years of followup. Most of this effect was due to a reduced incidence of depression in the first nine months following the intervention. (Depression was roughly equal among the two groups at two later followups.)
Importantly, the benefit of the prevention program was only seen among adolescents whose parents were not depressed at the time of enrollment in the study, underscoring the importance of treating parents in order to keep the whole family healthy.
Benefits of the prevention program included reductions in onset of depression and days depressed, and improvement in interpersonal and academic competence.
Brent and colleagues say that the study shows that it is possible to prevent depression, and this can have long-term developmental consequences. They encourage focusing on the entire family’s mental health treatment.
While the main benefits came early, Brent suggests that booster sessions for teens who begin to show symptoms of depression might refresh the benefits of the prevention program at a later time.
Editor’s Note: This study has enormous health implications as depression in adolescents tends to recur and is associated with a more difficult course than depression beginning in adulthood. Preventing depressions would theoretically have positive consequences for both psychiatric and physical health, as depression is associated with increased risk of suicide and decreased longevity from increases in cardiovascular disease. Researcher Joan Luby recently reported that children with prepubescent onset of depression have decreased hippocampal volume in adolescence, so it is possible that preventing depression may have positive implications for brain volume and function.
Several Types of Psychotherapy Effective in Childhood Bipolar Disorder
Childhood onset bipolar disorder can be highly impairing. Treatment usually includes medication, but several types of psychotherapy have also been found to be superior to treatment as usual. These include family focused therapy, dialectical behavior therapy and multifamily psychoeducation groups, including Rainbow therapy.
Family focused therapy, developed by David Miklowitz, consists of psychoeducation about bipolar disorder and the importance of maintaining a stable medication routine. Families are taught to recognize early symptoms of manic and depressive episodes, and how to cope with them. Families also learn communication and problem solving skills that can prevent stressful interactions.
Dialectical behavior therapy was developed by Marsha Linehan, initially for the treatment of borderline personality disorder. It can be useful in bipolar disorder because participants learn how to manage stressors that might otherwise trigger depression or mania. DBT teaches five skills: mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness, and self management.
Multifamily psychoeducation was developed by Mary Fristad. In groups, children and parents learn about mood disorders, including how to manage symptoms, and also work on communication, problem solving, emotion regulation, and decreasing family tension.
Rainbow therapy is a type of multifamily approach also known as child and family-focused cognitive-behavioral therapy (CFF CBT). It integrates individual cognitive-behavioral therapy with family psychoeducation and mindfulness skills training. In a recent article in the journal Evidence Based Mental Health, Miklowitz reviewed the current research on Rainbow therapy. While the research to date has many limitations, he highlighted some benefits of Rainbow therapy: its flexibility, and its focus on treating parents’ symptoms along with children’s illness.
Lithium Safely Reduces Mania in Kids 7–17
The first large, randomized, double-blind study of lithium in children and teens has shown that as in adults, the drug can reduce mania with minimal side effects. The study by researcher Robert Findling was published in the journal Pediatrics in October. Lithium is the best available treatment for adults, but until now little research had been done on treatments for children and teens with bipolar disorder.
In the study, 81 participants between the ages of 7 and 17 with a diagnosis of bipolar I disorder and manic or mixed episodes were randomized to receive either lithium or placebo for a period of eight weeks. By the end of the study, those patients taking lithium showed greater reductions in manic symptoms than those taking placebo. Among those taking lithium, 47% scored “much improved” or “very much improved” on a scale of symptom severity, compared to 21% of those taking placebo.
Dosing began at 900mg/day for most participants. (Those weighing less than 65 lbs. were started at 600mg/day.) Dosing could be gradually increased. The mean dose for patients aged 7–11 was 1292mg/day, and for patients aged 12–17 it was 1716mg/day.
Side effects were minimal. There were no significant differences in weight gain between the two groups. Those taking lithium had significantly higher levels of thyrotropin, a peptide that regulates thyroid hormones, than those taking placebo. If thyroid function is affected in people taking lithium, the lithium dosage may be decreased, or patients may be prescribed thyroid hormone.
Lithium Has Minimal Effects On Renal Function: Results Of Two New Large Controlled Studies
 Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
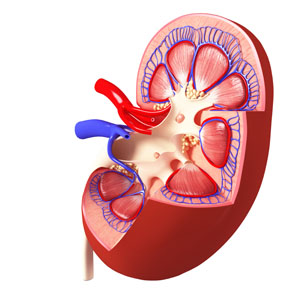
The first, by Stefan Clos et al. in The Lancet Psychiatry, included 1,120 patients followed for up to 12 years. On average, these patients had been exposed to lithium for a little over 4.5 years. Clos and colleagues determined patients’ estimated glomerular filtration rate (eGFR), a measure of how well the blood is filtered by the kidneys. The researchers concluded that there was “no effect of stable lithium maintenance therapy on the rate of change of eGFR over time” compared to other drugs such as quetiapine, olanzapine, or valproate.
The second new study, by Lars Vedel Kessing and colleagues in the journal JAMA Psychiatry, included 26,731 patients exposed to lithium and 420,959 exposed to anticonvulsants. Kessing and colleagues concluded that both exposure to lithium and exposure to an anticonvulsant were associated with an increased rate of chronic kidney disease, but lithium was not associated with end-stage kidney disease (the kind that requires dialysis or renal transplantation).
The three studies taken together suggest the following: Taking lithium for an average of 4–5 years does not affect kidney functioning, and longer exposure may not harm kidney function any more than other medications (such as anticonvulsants) would. However, kidney functioning (in terms of eGFR) does decline with age, and is also lower among those with higher baseline eGRF, those with other illnesses, those taking other drugs that affect the kidneys, and those who experience an episode of lithium toxicity. Read more
Saphris Reformulated for Kids with Bipolar I
The atypical antipsychotic asenapine has been reformulated for bipolar I disorder in children aged 10–17. The drug (trade name Saphris) was approved by the Food and Drug Administration (FDA) in 2009 for adults with schizophrenia and bipolar disorder. It is sometimes used as a treatment for mixed episodes (depression with some symptoms of mania).
The new formulation consists of 2.5mg tablets that are taken sublingually (under the tongue), and are available in a black cherry flavor. These can be prescribed as monotherapy for the acute treatment of manic or mixed episodes in children and teens.





