Dutch Study Links Low Vitamin D to Bipolar Disorder
A 2016 study in the Netherlands found that people with bipolar disorder are more likely to have vitamin D deficiency than the general population. Vitamin D deficiency has been linked to other psychiatric disorders including schizophrenia and unipolar depression. Poor diet and lack of exposure to sunlight can put someone at risk for vitamin D deficiency.
The study, led by Remco Boerman and published in the Journal of Clinical Psychopharmacology, included 118 adults with bipolar disorder, 149 with schizophrenia, and 53 with schizoaffective disorder. More than 30% of these participants had deficient levels of vitamin D. Only 15% had optimum levels of the vitamin. More than 22% of the participants with bipolar disorder were deficient in vitamin D, while close to 35% of those with schizophrenia and schizoaffective disorder were deficient.
Study participants had vitamin D levels that were 25% lower than those of the white Dutch population, and vitamin D deficiency was 4.7 times more common in those with psychiatric disorders than the general Dutch population.
The authors suggested screening people with bipolar disorder, schizophrenia, and schizoaffective disorder for low levels of vitamin D.
Vitamin D Deficiency Linked to Depression, But Supplements Helped
 A review article in the Journal of Affective Disorders in 2017 summarized findings linking vitamin D to depression. Researcher Gordon B. Parker and colleagues found an association between low vitamin D levels and depression. They also found that vitamin D supplements improved treatment in people with clinical depression and vitamin D deficiency.
A review article in the Journal of Affective Disorders in 2017 summarized findings linking vitamin D to depression. Researcher Gordon B. Parker and colleagues found an association between low vitamin D levels and depression. They also found that vitamin D supplements improved treatment in people with clinical depression and vitamin D deficiency.
Editor’s Note: Vitamin D supplements are an obvious recommendation for people who are deficient. What has not yet been resolved is whether vitamin D is helpful to people who are depressed but not vitamin D deficient.
In a 2013 study in the Australian and New Zealand Journal of Psychiatry, Nayereh Khoraminya and colleagues suggested that a 1500 IU dose of vitamin D3 combined with the selective serotonin reuptake inhibitor (SSRI) antidepressant fluoxetine was more effective than fluoxetine plus placebo in depressed patients who were not necessarily deficient in vitamin D.
Giving Infants Vitamin D Can Reduce Type 1 Diabetes
 A 2001 cohort study in Finland showed that giving vitamin D supplements to infants may reduce their risk for type 1 diabetes. The data for the study, by Elina Hyppönen and colleagues in the journal The Lancet, came from 10,366 people born in 1966. Their mothers were part of a medical registry that collected information on vitamin D given to children during the first year of their lives.
A 2001 cohort study in Finland showed that giving vitamin D supplements to infants may reduce their risk for type 1 diabetes. The data for the study, by Elina Hyppönen and colleagues in the journal The Lancet, came from 10,366 people born in 1966. Their mothers were part of a medical registry that collected information on vitamin D given to children during the first year of their lives.
Of the 10,366 people in Hyppönen’s study, 81 had been diagnosed with type 1 diabetes by the end of 1997. Those participants who were given vitamin D supplements during their first year of life were less likely to be diagnosed with type 1 diabetes than other participants. Those who regularly took the recommended dose at the time, 2000 IU daily, during their first year of life had significantly lower diabetes rates 33 years later.
TDCS May Improve ADHD Symptoms
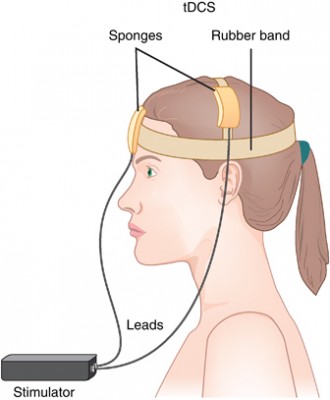 Transcranial direct current stimulation (tDCS) is a therapy in which electrodes placed on the skull deliver a steady, low level current to the brain, changing its threshold for electrical activity. Anodal tDCS to the prefrontal cortex can improve working memory. In a small 2017 study in the Journal of Neural Transmission, Cornelia Soff and colleagues found for the first time that tDCS may improve symptoms of attention-deficit hyperactivity disorder (ADHD).
Transcranial direct current stimulation (tDCS) is a therapy in which electrodes placed on the skull deliver a steady, low level current to the brain, changing its threshold for electrical activity. Anodal tDCS to the prefrontal cortex can improve working memory. In a small 2017 study in the Journal of Neural Transmission, Cornelia Soff and colleagues found for the first time that tDCS may improve symptoms of attention-deficit hyperactivity disorder (ADHD).
People with ADHD tend to have underactivation of the prefrontal cortex and deficits in working memory. The study randomized 15 young people aged 12–16 (three girls and twelve boys) to receive either real tDCS or a sham stimulation. The anodal tDCS was delivered at 1 mA targeting the left dorsolateral prefrontal cortex for 5 days. Those participants who received tDCS showed a reduction in inattention, impulsivity, and hyperactivity compared to those who received the sham stimulation. The effects were more pronounced 7 days after the stimulation, suggesting that tDCS’ effects may be long-term. Larger, more definitive trials are needed to clarify the effects of tDCS on ADHD, but these preliminary findings are promising.
NAD+ Supplements May Not Contain Much NAD+
NAD, or nicotinamide adenine dinucleotide, is found in all living cells. Its oxidized form, NAD+, has become popular as a nutritional supplement following a 2013 Harvard study that suggested it might slow aging in mice. However, commercially available NAD+ supplements may contain less than 100mg of NAD+, when ten times that amount would be required to produce any effect. NAD+ has not been tested in clinical trials.
Vitamin B3 is a better-tested alternative. A 2016 controlled clinical trial of a type of vitamin B3 called nicotinamide riboside (NR) found that this supplement was safe for humans and increased levels of NAD+. In the study by Samuel A.J. Trammell and colleagues in the journal Nature Communications, single doses of 100mg, 300mg, and 1000mg were all found to be safe. Larger doses increased NAD+ metabolism by greater amounts.
Check with your doctor before taking an NAD+ or vitamin B supplements.
Coenzyme NAD+ Postpones Aging in Mice and Worms
 Aging cells seem to lose their ability to repair DNA, while the mitochondria that power cells also become less reliable. A coenzyme called NAD+ may be able to postpone these changes. NAD+, which is found in all living cells, naturally decreases with age.
Aging cells seem to lose their ability to repair DNA, while the mitochondria that power cells also become less reliable. A coenzyme called NAD+ may be able to postpone these changes. NAD+, which is found in all living cells, naturally decreases with age.
A 2016 article by Evandro Fei Fang and colleagues in the journal Cell Metabolism reports that giving mice and roundworms supplemental NAD+ postponed cell aging and extended the lives of these animals.
The researchers hope this research might eventually help patients with Alzheimer’s and Parkinson’s’ diseases.
Single Dose of Modafinil Improved Memory in People in Remission from Depression
 Modafinil is a wake-promoting medication used to treat narcolepsy, but studies have also shown that it can improve cognition in people with schizophrenia or attention deficit hyperactivity disorder. It may also help people with lingering cognitive difficulties after recovering from a depression. A 2016 article in the journal Biological Psychiatry reported that a single 200mg dose of modafinil improved performance on tests of episodic memory and working memory (but not planning or attention).
Modafinil is a wake-promoting medication used to treat narcolepsy, but studies have also shown that it can improve cognition in people with schizophrenia or attention deficit hyperactivity disorder. It may also help people with lingering cognitive difficulties after recovering from a depression. A 2016 article in the journal Biological Psychiatry reported that a single 200mg dose of modafinil improved performance on tests of episodic memory and working memory (but not planning or attention).
The study by researcher Barbara Sahakian and colleagues included 60 patients who had recently recovered from a depression. They took some cognitive tests to establish a baseline of their performance. A week later, they were given either a placebo or a single dose of modafinil, and two hours later they completed the cognitive tests again. The modafinil group performed better on the memory-related tasks.
While side effects were limited, two participants who received modafinil had sleep disturbances that night.
Longer-term studies are needed to determine whether modafinil is safe and effective if taken over a longer period of time. Cognitive dysfunction can interfere with daily tasks such as work or school and put people at greater risk of relapse, so effective treatments have the potential to greatly improve quality of life for people in remission from depression.
Caffeine One of Several Compounds That May Protect Against Dementia
A 2017 article by Yousuf O. Ali and colleagues in the journal Scientific Reports finds that 24 different compounds may boost a brain enzyme that protects against dementia. The enzyme, NMNAT2, protects neurons from stress and combats misfolded proteins called tau that form plaques in the brain as people age.
Ali and colleagues screened 1280 compounds to identify those that might increase NMNAT2 production. Twenty-four of these looked promising, including caffeine and rolipram, an “orphaned drug” once studied as an antidepressant but discontinued in the 1990s. Others with weaker effects on NMNAT2 production included the atypical antipsychotic ziprasidone, cantharidin (a wart-removing substance secreted by blister beetles), fungal metabolite wortmannin, and retinoic acid, a vitamin A derivative. Thirteen of the compounds tested decreased NMNAT2 production.
The researchers followed up the caffeine finding by testing caffeine in mice genetically engineered to produce less NMNAT2. The caffeine administration normalized NMNAT2 production levels in these mice.
Senior researcher Hui-Chen Lu hopes this research will lead to the development of new drugs that can create a chemical blockade against the effects of neurodegenerative illnesses.
Antipsychotic Drug Pimavanserin Seems to Reduce Psychosis in People with Alzheimer’s
 The antipsychotic drug pimavanserin was approved by the US Food and Drug Administration last year as a treatment for hallucinations and delusions in Parkinson’s disease. Now it looks as though it may also help people with Alzheimer’s disease. Pimavanserin works differently than other antipsychotic medications—a selective serotonin inverse agonist, it acts at serotonin HT2A receptors to produce effects opposite to those that serotonin would produce at the same receptor.
The antipsychotic drug pimavanserin was approved by the US Food and Drug Administration last year as a treatment for hallucinations and delusions in Parkinson’s disease. Now it looks as though it may also help people with Alzheimer’s disease. Pimavanserin works differently than other antipsychotic medications—a selective serotonin inverse agonist, it acts at serotonin HT2A receptors to produce effects opposite to those that serotonin would produce at the same receptor.
In a trial of 181 patients with Alzheimer’s and psychotic symptoms, those who received 34 mg/day of pimavanserin had a significant improvement in psychotic symptoms in six weeks compared to those who received placebo.
Over 12 weeks of treatment, pimavanserin did not impair cognition, as atypical antipsychotics can do.
Pimavanserin was well tolerated. The most common side effects were falls, urinary tract infections, and agitation. Like other atypical antipsychotics, the drug carries a box warning from the FDA that there is an increased risk of death when the drug is used to treat older people with dementia-related psychosis.
The FDA has designated pimavanserin a breakthrough therapy and is giving it priority review. These designations can speed up the development and review of a drug and are granted when a drug looks like it will be substantially better or safer than existing treatments for a serious condition.




