Meta-Analysis Finds Antidepressants More Effective Than Placebo
In a 2018 article in the journal The Lancet, researchers led by Andrea Cipriani compared the efficacy of 21 different antidepressants and established that antidepressants are more effective than placebo at reducing unipolar depression. To date, this is the largest meta-analysis of double-blind, randomized controlled studies of antidepressant efficacy, including 522 trials and a total of 116,477 participants. All 21 of the antidepressants were found to be more effective than placebo.
Looking at head to head studies, Cipriani and colleagues found that the most effective antidepressants were agomelatine, amitriptyline, escitalopram, mirtazapine, paroxetine, venlafaxine, and vortioxetine. The least effective antidepressants were fluoxetine, fluvoxamine, reboxetine, and trazodone.
In terms of tolerability, agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine were most tolerable to patients, while amitriptyline, clomipramine, duloxetine, fluvoxamine, reboxetine, trazodone, and venlafaxine caused the most study dropouts due to side effects. Only agomelatine and fluoxetine had better dropout rates than placebo.
Interestingly, agomelatine, the medication found to be most effective and most tolerable, is unavailable in the US. Pharmaceutical company Novartis, which owns the rights to the drug, was disappointed by some lackluster studies of the drug and never applied for Food and Drug Administration approval to sell it in the US. The studies found potential problems regarding drug interactions related to the metabolic enzyme CYP1A2 and a risk of liver damage with longer-term use.
Editor’s Note: This meta-analysis should end any remaining controversy about the efficacy of antidepressants in the acute treatment of unipolar depression.
This study did not address maintenance treatment for the prevention of depressive episodes. Researcher John R. Geddes and colleagues have found robust, statistically significant data that continuation treatment with antidepressants can prevent depressive relapse, suggesting that if patients continue taking effective antidepressants, rather than switching to placebo, the antidepressants can reduce depressive occurrences by about 70%.
It is now recommended in most guidelines that patients with two or three prior episodes of depression consider staying on antidepressants indefinitely over their lifetime in order to prevent recurrence. Antidepressants increase the creation of new neurons and brain-derived neurotrophic factor (BDNF), which protects neurons and is important for learning and memory. Antidepressants can also prevent loss of hippocampal volume.
Using Antidepressants During Pregnancy Likely Does Not Increase Autism Risk
In the past year or so, several meta-analyses have analyzed data from numerous studies of a possible link between antidepressant use in pregnancy and autism in the offspring. In a 2017 article in the Journal of Clinical Psychiatry, researcher Chittaranjan Andrade offers a meta-analysis of these previous meta-analyses, and determines that while there is a small link between antidepressant use in pregnancy and autism in the offspring, it is most likely the mother’s depressive illness rather than the medications that is responsible for this link.
Andrade found that antidepressant exposure was linked to an increased risk of autism spectrum disorders in the offspring even when the antidepressant use occurred only before conception occurred, when it could not possibly have affected the future fetus’ physiology. This implies that it is the mother’s illness rather than the antidepressant treatment that is a determinant of autism risk.
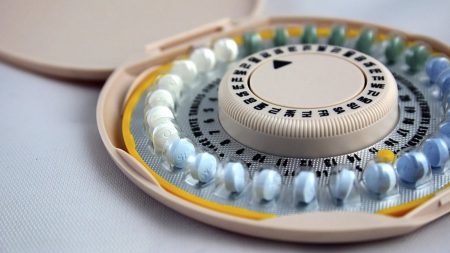
Use of Hormonal Contraceptives May Increase Depression Risk in Young Women
Women, particularly adolescent women, are at increased risk of developing depression if they use hormonal contraceptives, according to a 2016 study in the journal JAMA Psychiatry. The study by Charlotte Wessel Skovlund and colleagues used data from a Danish registry of more than one million women between the ages of 15 and 34 who had no history of depression or other psychiatric disorders. During follow-up (which lasted an average of 6.4 years), 55% of the women were using or had recently used hormonal contraceptives. These women were more likely to be prescribed an antidepressant for the first time, and more likely to be diagnosed with depression compared to women who did not use hormonal contraceptives.
The increased risk of being prescribed an antidepressant varied by contraceptive type. The norgestrolmin patch increased risk by 2.0 times, and the etonogestrel vaginal ring did so by 1.6 times. The levonorgestrel intrauterine device (IUD) made an antidepressant prescription 1.4 times more likely. Progestin-only pills increased risk by 1.34 times and combined oral contraceptive pills increased it by 1.23 times compared to women who did not use oral contraceptives.
The relative risk peaked at around six months after starting hormonal contraceptives.
Patients aged 15–19 were particularly vulnerable to depression. The likelihood of receiving an antidepressant prescription was 1.8 times higher in teens taking combined pills, 2.2 times higher in those taking progestin-only pills, and 3 times higher in teens using hormonal methods of birth control that are not delivered orally compared to those who did not use hormonal contraceptives at all.
Antidepressant Use in Pregnancy Does Not Increase Autism Risk
 Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
One of the studies, by researcher Ayesha C. Sujan and colleagues, analyzed exposure to antidepressants in the first trimester and neurodevelopmental outcomes in almost 1.6 million Swedish children. Antidepressant use did slightly increase the chance of a preterm birth, but was not linked to autism spectrum disorder, attention-deficit hyperactivity disorder (ADHD), or small size of the fetus.
The researchers suggested that doctors and patients work together to decide how depression should be treated during pregnancy, based on severity of the depression, treatment history, and access to services.
The other study, by researcher Hilary K. Brown and colleagues, analyzed 36,000 births in Ontario, Canada and found no increased risk of autism spectrum disorder based on antidepressant exposure in utero. The study controlled for 500 characteristics such as mother’s education, age, and health history.
The journal JAMA Pediatrics also published a meta-analysis and review of 10 studies on the subject, finding that a woman’s history of psychiatric disorders weakened any link between antidepressant use during pregnancy and risk of autism spectrum disorder in her children. This implies that the underlying illness, not its treatment, may be responsible if there is any link between depression and autism. The meta-analysis was carried out by researcher Antonia Mezzacappa and colleagues.
Only Fluoxetine is More Effective Than Placebo for Children and Adolescents with Depression
 In a meta-analysis published in 2016, researchers Andrea Cipriani, Xinyu Zhou, and colleagues reported that many antidepressants are not effective in children and adolescents. Fluoxetine alone was more effective than placebo. Other antidepressants also caused high study drop-out rates compared to placebo.
In a meta-analysis published in 2016, researchers Andrea Cipriani, Xinyu Zhou, and colleagues reported that many antidepressants are not effective in children and adolescents. Fluoxetine alone was more effective than placebo. Other antidepressants also caused high study drop-out rates compared to placebo.
In an article published in the journal The Lancet, Cipriani, Zhou, and colleagues analyzed 34 randomized, controlled clinical trials of antidepressants in children and adolescents. These trials included a total of 5,260 participants and 14 different antidepressants.
The researchers determined that much of the evidence was of a low quality. Only fluoxetine was statistically significantly more effective than placebo. Fluoxetine was also more tolerable to patients than duloxetine or imipramine. Patients who received imipramine, venlafaxine, or duloxetine were more likely to drop out of studies due to adverse events compared to patients who received placebo.
The authors suggest that prescribing antidepressants to children or adolescents may not necessarily be beneficial, and that fluoxetine is probably the best option to consider.
Editor’s Note: It may be best to use caution when prescribing antidepressants to children or adolescents. First, these data that suggest that many antidepressants are ineffective in young people. In addition, depression in children and adolescents may be a sign of bipolar disorder, and antidepressant use may cause activation or switching into mania in vulnerable patients.
While there is a warning about using antidepressants in young people because of the risk of increased suicidal ideation, the actual suicide rate in young populations decreases when these patients take antidepressants and cognitive behavioral therapy. Psychotherapy should be a high priority. Other safe adjunctive approaches might include omega-3 fatty acids, N-acetylcysteine, vitamin D3, and folic acid. Evidence for the efficacy of rTMS in young people is also positive and growing.
Meta-Analysis Suggests Statins Can Help Treat Depression
Depression and poor cardiovascular health often go hand in hand. Now it seems a treatment for high cholesterol may also help treat depression. A 2016 study by E. Salagre and colleagues in the Journal of Affective Disorders analyzed evidence from 3 earlier studies of drugs called statins, which inhibit an enzyme needed for the production of cholesterol, for people with depression.
The three studies included a total of 165 participants taking an antidepressant (citalopram or fluoxetine) for moderate or severe depression. Of these participants, 82 were prescribed an additional statin (lovastatin, atorvastatin, or simvastatin), while the remaining were given a placebo. After 6 to 12 weeks, those who had received a statin reported greater improvement in their depression than those who had received a placebo in addition to the antidepressant. No serious side effects were reported.
These data are also consistent with other studies showing that women on statins had fewer depressions over subsequent years than those not taking statins.
Thiamine (Vitamin B1) May Increase Effectiveness of Antidepressants
A new study suggests that the nutritional supplement vitamin B1, also known as thiamine, can improve symptoms of depression when taken with an antidepressant. Edith Holsboer-Trachsler and colleagues presented the research from their randomized, double-blind, placebo-controlled study at a recent scientific meeting. In a 12-week study, about 50 adults (averaging 35 years of age) with major depression were prescribed a selective-serotonin reuptake inhibitor (SSRI) antidepressant. In addition, half received thiamine supplements while the other half were given placebos. Starting at six weeks, those receiving thiamine with their antidepressant showed more improvement in their depressive symptoms than those receiving the antidepressant alone.
Thiamine is an essential nutrient for humans. It is found in foods such as yeast, pork, cereal grains, and certain vegetables. Thiamine deficiency has been linked to irritability and symptoms of depression, while thiamine supplementation can improve mood and reduce feelings of stress. No side effects were reported in the study.
Holsboer-Trachsler and colleagues hope that thiamine supplementation may help patients adhere to their antidepressant regimens by decreasing the time it takes until their moods begin to lift.
Treating Prenatal Depression Improves Outcomes for Mothers and Babies
 A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
The 2016 study by Kartik K. Venkatesh and colleagues in the journal Obstetrics & Gynecology included 7,267 women who gave birth after at least 20 weeks of pregnancy. About 11% of the women screened positive for depression during their pregnancy. Depressed mothers-to-be were more likely to give birth before 37 weeks and before 32 weeks compared to nondepressed mothers-to-be. The depressed women were also more likely to deliver small babies or babies weighing under 2500g.
About 7% of the women in the study received antidepressant medication. Compared to nondepressed women, the women taking antidepressants did not have greater rates of early delivery or small babies. However, the authors caution that because so few women received antidepressants, the study does not reveal whether antidepressants improve outcomes for depressed pregnant women.
Most SSRIs Free of Birth Defect Risk Early in Pregnancy, Fluoxetine and Paroxetine are Exceptions
A large study of women who took selective serotonin reuptake inhibitor (SSRI) antidepressants in the month before pregnancy and throughout the first trimester suggests that there is a smaller risk of birth defects associated with SSRI use than previously thought, though some risks were elevated in women who took paroxetine or fluoxetine.
The 2015 study, by Jennita Reefhuis and colleagues in the journal BMJ, investigated the drugs citalopram, escitalopram, fluoxetine, paroxetine, and sertraline, and examined birth defects that had previously been associated with SSRI use in smaller studies. The participants were 17,952 mothers of infants with birth defects and 9,857 mothers of infants without birth defects who had delivered between 1997 and 2009.
Sertraline was the most commonly used SSRI among the women in the study. None of the birth defects included in the study were associated with sertraline use early in pregnancy. The study found that some birth defects were 2 to 3.5 times more likely to occur in women who had taken fluoxetine or paroxetine early in their pregnancies.
Five different birth defects, while uncommon, were statistically linked to paroxetine use: anencephaly (undersized brain), heart problems including atrial septal defects and right ventricular outflow tract obstruction defects, and defects in the abdominal wall including gastroschisis and omphalocele. Two types of birth defects were associated with fluoxetine use: right ventricular outflow tract obstruction defects and craniosynostosis (premature fusion of the skull bones). Absolute incidence of these defects was also low.
Another Antidepressant Fails in Bipolar Depression
Despite repeated studies, including meta-analyses, showing that antidepressants that work in unipolar depression do not work in bipolar depression as adjuncts to mood stabilizers, antidepressants remain widely used for the treatment of bipolar depression. A recent study of the antidepressant agomelatine has shown that it is not effective in bipolar depression. In patients taking lithium or valproate but still depressed, agomelatine was no better than placebo at reducing depression.
Agomelatine has an unusual mechanism of action (blockade of 5HT-2C receptors and activation of melatonin M1 and M2 receptors) that helps normalize sleep and circadian rhythms, but only in unipolar depression. Until this study by Lakshmi Yatham and colleagues in the British Journal of Psychiatry, it was thought that these properties would make the drug ideal for bipolar depression.
Three atypical antipsychotics are have been approved by the Federal Drug Administration for bipolar depression: quetiapine (Seroquel), lurasidone (Latuda), and the olanzepine-fluoxetine combination Symbyax. These, used alongside mood stabilizers (lithium, valproate, carbamazepine, and lamotrigine) are more effective treatments for bipolar depression. There are other adjunctive treatments that may be helpful, such as the antioxidant N-acetylcysteine, vitamin D3, and folate.