Lithium Better than Other Mood Stabilizers for Youth with Bipolar Disorder
A new study by Danella M. Hafeman and colleagues finds that lithium is superior to other mood stabilizers in young people. The data in this case come from 340 youth aged 7–17 who participated in a study known as Course and Outcome of Bipolar Youth (COBY).
At each visit over an average of 10 years, participants reported medications taken, symptoms they had experienced, etc. during the preceding six-month period. During times that participants had taken lithium (compared to other mood stabilizers) they were older, on fewer antidepressants, and they were less likely to have an anxiety disorder.
Those participants who took lithium had half as many suicide attempts, fewer depressive symptoms, less psychosocial impairment, and less aggression than those who took other mood stabilizers.
The researchers concluded, “Findings are consistent with adult studies, showing that lithium is associated with decreased suicidality, less depression, and better psychosocial functioning. Given the paucity of evidence regarding lithium in children and adolescents, these findings have important clinical implications for the pharmacological management of youth with bipolar disorder.”
Editor’s Note: Lithium should especially be considered in those with a family history of mood disorders, and in particular in those with a family history of good response to lithium. Lithium is under-prescribed in both adults and children and should be given much higher consideration in light of the multiple benefits it provides in addition to mood stabilization. These include maintenance of memory, increases in longevity (perhaps based in its ability to increase the length of telomeres, the bits of protective material at the end of DNA strands that deteriorate with age and illness), and neuroprotection against loss of gray and white matter volume in the brain, which often occurs in mood disorders.
Prazosin Effective and Well-Tolerated for PTSD in Young People
In a poster session at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), three posters highlighted the efficacy and tolerability of prazosin, a drug typically used to treat high blood pressure, for the treatment of childhood-onset post-traumatic stress disorder (PTSD).
Researchers Samira Khan and Taniya Pradhan of West Virginia University reviewed cases in which 39 patients aged 8–19 received 1–5 mg of prazosin at bedtime. The mean dose was 1.72 mg. Sleep (including nightmares) improved in 92.3% of the youths, and mood improved in 33.3%. Sleep improved more in patients who received lower doses (1–2 mg) than those who received higher doses. About 70% of the patients whose data were included in the case series were also receiving psychotherapy while being treated with prazosin.
In another poster, researcher Vladimir Ferrafiat and colleagues from University Hospital of Rouen in France reported on a prospective study of 18 participants under age 15 with severe PTSD who were unresponsive to other medications. The participants were given 1 mg of prazosin at bedtime, which was increased to 3 mg in 20% of the participants. The youth were assessed weekly over a one-month period. Improvement was seen in all domains, including sleep, nightmares and daytime intrusive symptoms. Prazosin was well tolerated, with only one patient experiencing low blood pressure, which did not necessitate withdrawal from the study.
In the final poster, researcher Fatima Motiwala and colleagues reviewed the literature on the treatment of PTSD in children. Motiwala indicated that among the options, prazosin was widely used in her hospital, at doses starting at 1 mg given at bedtime and increasing to a mean of 4 mg at bedtime with excellent results and tolerability.
Editor’s Note: Although these were not double-blind controlled studies, the findings are noteworthy in that they provide consistent data on the effectiveness and tolerability of prazosin in low doses in children with PTSD, essentially mirroring controlled data in adults, where higher doses are typically required.
Lithium Reverses Some White Matter Abnormalities in Youth with Bipolar Disorder
 Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Editor’s Note: This is another reason to consider the use of lithium in children with bipolar disorder. Lithium treatment may help normalize some of the earliest signs of neuropathology in the illness.
Lithium FDA-Approved for Bipolar Disorder in Children 7–17
 In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
Vitamin Methyl B12 Improved Autism Symptoms in Randomized, Placebo-Controlled Study
In a 2016 article in the Journal of the American Academy of Child and Adolescent Psychiatry, Robert L. Hendren and colleagues described an 8-week study in which the vitamin methyl B12 improved symptoms of autism spectrum disorders in children.
Fifty-seven children were randomized to receive either 75??g/kg of methyl B12 injected under the skin every three days or saline injections as a placebo instead. Methyl B12 improved the children’s autism symptoms compared to placebo. The improvements correlated with increases in levels of the amino acid methionine in the blood and improvements in cellular methylation capacity. Children with autism spectrum disorders have reduced ability to methylate (i.e. add methyl groups to) DNA. The methylation process helps convert the toxic amino acid homocysteine into beneficial methionine. The children who received methyl B12 showed a reduction in homocysteine and a better ratio of methionine to homocysteine.
Homocysteine is bad for the heart, for cognition, and for fetal development, while methionine can help improve depression and is important to many cellular reactions. Converting homocysteine to methionine requires vitamin B12 and folate, another B vitamin found in foods such as green vegetables and beans.
Taking folate supplements can help make antidepressants more effective by aiding the methylation process. However, some people have a common variation in the MTHFR gene that makes it difficult for the body to make use of folate. These people would need to take the nutritional supplement L-methylfolate instead of regular folate to help in the conversion of homocysteine to s-adenosylmethionine (SAMe, which acts as an antidepressant).
Preventing Illness in the Offspring of a Parent with Bipolar Disorder
A 2018 article by researcher Robert Freedman and colleagues in the American Journal of Psychiatry reported that prenatal nutritional supplements can reduce mental illness in at-risk offspring. The article made a good case for supplementation with folate, phosphatidylcholine, and vitamins A and D.
Here we describe some additional ways to minimize risk of mental illness in children who are at risk for bipolar disorder or other mental illnesses.
Some efforts at prevention can begin even before a child is conceived. Avoiding smoking or drinking alcohol and maintaining a nutritious diet to prevent inflammation and excessive weight gain before conception could reduce adverse epigenetic effects on the offspring. Epigenetics refers to environmental influences on gene transcription. The impact of life experiences such as a mother or father’s substance use is not registered in their child’s DNA sequence, but can influence the structure of the child’s DNA or its packaging.
Maternal good health and wellbeing during pregnancy has also been shown to improve neonatal health and functioning.
Once a child is born, they can be encouraged in healthy habits, including a nutritious diet, good sleeping habits, regular vigorous exercise, and mindfulness/meditation training (which pediatric psychiatrist James Hudziak has suggested should be universal).
For a child who is beginning to develop mood or behavioral symptoms, more intensive intervention may be prudent. Research supports the effectiveness of family interventions such as family-focused therapy (FFT) for youth with depression, cyclothymia, or bipolar disorder not otherwise specified (BP-NOS) and a family history of bipolar disorder. Researcher David J. Miklowitz described the effects of this intervention in a 2013 article in the Journal of the American Academy of Child and Adolescent Psychiatry.
Depression in children 3 to 6 years of age is as common as depression in older children (with rates around 1–2%), and robust improvements have been observed when families engage in parent child interaction therapy (PCIT) with a focus on emotional development. In PCIT, parents are coached while interacting with their children and encouraged to establish warm interactions while setting appropriate limits. In a study by Joan L. Luby and colleagues published in the American Journal of Psychiatry in 2018, using PCIT modified to include an emotional development component improved depression and associated symptoms in children aged 3 to 11, and it also improved mothers’ mood and behavior. Read more
Lithium Superior to Other Mood Stabilizers in a Longitudinal Study of Bipolar Youth
At a late-2018 scientific meeting, researcher Danella Hafeman and colleagues reported some results of the Course and Outcome of Bipolar Youth (COBY) study. The study includes long-term follow up of 413 youth with bipolar disorder, who ranged in age from 7 to 17 years old. Hafeman and colleagues reported that taking lithium more than 75% of the time was linked to fewer suicide attempts, fewer depressive symptoms, and fewer psychosocial difficulties than taking another mood stabilizer (such as an atypical antipsychotic, lamotrigine, or valproic acid) more than 75% of the time after adjusting for demographic variables.
Despite the limitations of observational studies such as this one, the authors concluded, “Our findings are consistent with studies in adult populations, showing that lithium (compared to other mood stabilizers) is associated with decreased suicidality, less depression, and better psychosocial functioning. Given the paucity of evidence regarding lithium in children and adolescents, these findings have important clinical implications for the pharmacological management of youth with [bipolar disorder].”
Editor’s Note: These observations are consistent with several other studies. Researcher Barbara Geller and colleagues observed in eight years of follow up of children diagnosed with bipolar disorder that those who were treated with lithium spent more time in remission than those who took other medicines. A randomized controlled study by researcher Robert Findling and colleagues documented that maintenance lithium treatment was more effective than placebo at preventing bipolar episodes. Together, these data suggest that lithium should be used more often in the long-term treatment of children with bipolar disorder.
Way ahead of his time in about 1993, the renowned child psychiatrist Dennis Cantwell said something like this: “If I had an adolescent child with a first manic episode, I would have him stay on lithium for the rest of his life.” He seems to have been prescient, as evidence of the many benefits of lithium over other alternatives in the treatment of both children and adults has been accumulating.
An open-access review article this editor (Robert M. Post) published in the journal Neuropsychopharmacology in 2017, “The New News about Lithium: An Underutilized Treatment in the United States,” argues that lithium’s many benefits have been underestimated, while its side effects have been overestimated. It is my view that it would be beneficial if lithium were more often included in the treatment regimen of adults as well as children and adolescents with bipolar disorder.
Lithium has an astounding range of effectiveness. It prevents recurrent depressions and suicide (even in those with unipolar depression), increases hippocampal and cortical volume, protects memory, and increases the length of telomeres (the end portions of chromosomes that protect them as they replicate). In multiple animal models of neurological diseases, it has also been found to be neuroprotective and to reduce the size of brain lesions.
Poll Finds 87% of US Adults Think Children Need More Mental Health Support
In a poll of 2,014 adults in the US, 87% believed that children need more mental health support. For over a decade, the editors of the BNN have been emphasizing the great need for earlier recognition and treatment of children with bipolar and related mood and behavioral disorders. With so many Americans in agreement, now could be the time to direct public health and research funds to the better support of children’s mental health. Sadly this does not yet seem to be the case, but this is an election year. We need stand-up leaders in Congress to marshal the resources to increase the well-being of current and future generations.
Treatment Approaches to Childhood-Onset Treatment-Resistant Bipolar Disorder
Dear readers interested in the treatment of young children with bipolar disorder and multiple other symptoms: In 2017, BNN Editor Robert M. Post and colleagues published an open access paper in the journal The Primary Care Companion for CNS Disorders titled “A Multi-Symptomatic Child: How to Track and Sequence Treatment.” The article describes a single case of childhood-onset bipolar disorder shared with us via our Child Network, a research program in which parents can create weekly ratings of their children’s mood and behavioral symptoms, and share the long-term results in graphic form with their children’s physicians.
Here we summarize potential treatment approaches for this child, which may be of use to other children with similar symptoms.
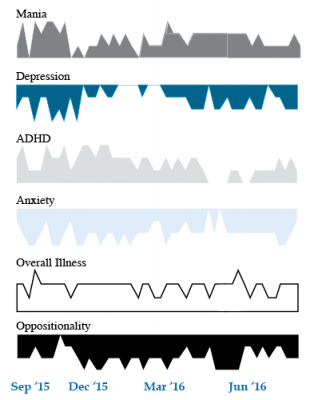
We present a 9-year-old girl whose symptoms of depression, anxiety, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania were rated on a weekly basis in the Child Network under a protocol approved by the Johns Hopkins School of Medicine Institutional Review Board. The girl, whose symptoms were rated consistently for almost one year, remained inadequately responsive to lithium, risperidone, and several other medications. We describe a range of other treatment options that could be introduced. The references for the suggestions are available in the full manuscript cited above, and many quotes from the original article are reprinted here directly.
As illustrated in the figure below, after many weeks of severe mania, depression, and ADHD, the child initially appeared to improve with the introduction of 4,800 micrograms per day of lithium orotate (a more potent alternative to lithium carbonate that is marketed as a dietary supplement), in combination with 1 mg per day of guanfacine, and 1 mg per day of melatonin.
Despite continued treatment with lithium orotate (up to 9,800 micrograms twice per day), the patient’s oppositional behavior worsened during the period from November 2015 to March 2016, and moderate depression re-emerged in April 2016. Anxiety was also generally less severe from December 2015 to July 2016, and weekly ratings of overall illness remained in the moderate severity range (not illustrated).
In June 2016, the patient began taking risperidone (maximum dose 1.7 mg/day) instead of lithium, and her mania improved from moderate to mild. There was little change in her moderate but fluctuating depression ratings, but her ADHD symptoms got worse.
The patient had been previously diagnosed with bipolar II disorder and anxiety disorders including school phobia, generalized anxiety disorder, and obsessive compulsive disorder.
Given the six weeks of moderate to severe mania that the patient experienced in October and November 2015, she would meet criteria for a diagnosis of bipolar I disorder.
Targeting Symptoms to Achieve Remission
General treatment goals would include: mood stabilization prior to use of ADHD medications, a drug regimen that maximizes tolerability and safety, targeting of residual symptoms with appropriate medications supplemented with nutraceuticals, recognition that complex combination treatment may be necessary, and combined use of medications, family education, and therapy.
Mood Stabilizers and Atypical Antipsychotics to Maximize Antimanic Effects
None of the treatment options in this section are approved by the US Food and Drug Administration for use in children under 10 years of age, so all of the suggestions are “off label.” Further, they may differ from what other investigators in this area of medicine would suggest, especially since evidence-based medicine’s traditional gold standard of randomized placebo-controlled clinical trials is impossible to apply here, given the lack of research in children with bipolar disorder.
As we share in the original article, reintroducing lithium alongside risperidone could be effective, as “combinations were more effective than monotherapy in a study [by] Geller et al. (2012), especially when they involved an atypical antipsychotic such as risperidone. This might include the switch from lithium orotate to lithium carbonate,” the typical treatment for bipolar disorder, on which more research has been done. “Combinations of lithium and valproate were also more effective than either [drug alone]…in the studies of Findling et al. (2006),” and many patients needed stimulants in addition.
“Most children also needed combinations of mood stabilizers (lithium, carbamazepine, valproate) in the study [by] Kowatch et al. (2000).” In a 2017 study by Berk et al. of patients hospitalized for a first mania, randomization to lithium for one year was more effective than quetiapine on almost all outcome measures.
Targeting ADHD
“[The increased] severity of [the child’s] ADHD despite improving mania speaks to the…utility of adding a stimulant to the regimen that already includes…guanfacine,” which is a common non-stimulant treatment for ADHD. “This would be supported by the data of Scheffer et al. (2005) that stimulant augmentation for residual ADHD symptoms does not [worsen] mania, and that the combination of a stimulant and guanfacine may have more favorable effects than stimulants alone.”
However, the consensus in the field is that mood stabilization should be achieved first, before low to moderate (but not high) doses of stimulants are added. “Thus, in the face of an inadequate response to the lithium-risperidone combination in this child, stimulants could be deferred until better mood stabilization was achieved.”
Other Approaches to Mood Stabilization and Anxiety Reduction
“The anticonvulsant mood stabilizers (carbamazepine, lamotrigine, and valproate) each have considerable mood stabilizing and anti-anxiety effects, at least in adults with bipolar disorder. With inadequate mood stabilization of this patient on lithium and risperidone, we would consider the further addition of lamotrigine.
Lamotrigine appears particularly effective in adults with bipolar disorder who have a personal history and a family history of anxiety (as opposed to mood disorders), and it has positive open data in adolescents with bipolar depression and in a controlled study of maintenance (in teenagers 13–17, but not in preteens 10–12) (Findling et al. 2015). With better mood stabilization, anxiety symptoms usually diminish…, and we would pursue these strategies [instead of using] antidepressants for depression and anxiety in young children with bipolar disorder.”
“Carbamazepine appears to be more effective in adults with bipolar who have [no] family history of mood disorders,” unlike lithium, which seems to work better in people who do have a family history of mood disorders.
“While the overall results of oxcarbazepine in childhood mania were negative, they did exceed placebo in the youngest patients (aged 7–12) as opposed to the older adolescents (13–18) (Wagner et al. 2006).
“There are long-acting preparations of both carbamazepine (Equetro) and oxcarbazepine (Oxtellar) that would allow for all nighttime dosing to help with sleep and reduce daytime side effects and sedation. Although data [on] anti-manic and antidepressant effects in adults are stronger for carbamazepine than oxcarbazepine,” there are good reasons to consider oxcarbazepine. First, there is the finding mentioned above that oxcarbazepine worked best in the youngest children. Second, there is a lower incidence of severe white count suppression on oxcarbazepine. Third, it has less of an effect on liver enzymes than carbamazepine. However, low blood sodium levels are more frequent on oxcarbazepine than carbamazepine.
Other Atypical Antipsychotics That May Improve Depression
Playing Tackle Football Before Age 12 May Be Bad for the Brain
A 2017 study found that men who began playing American tackle football before age 12 were more likely to have depression, apathy, problems with executive functioning, and behavioral issues in adulthood than their peers who began playing football after age 12. Duration of football play did not seem to matter—those men who stopped playing football after high school were just as likely to be affected in adulthood as those who went on to play football in college or professionally.
The study by Michael L. Alosco and colleagues was published in the journal Translational Psychiatry. It included 214 men (average age 51) who had played football in their youth, but not other contact sports. The men reported their own experiences with depression, apathy, cognitive function, and behavioral regulation. Those who began football before age 12 were twice as likely to report impairment in behavioral regulation, apathy, and executive function than those who began playing later. Those who started younger were also three times more likely to have clinical depression in adulthood than those who started older.
According to Alosco and colleagues, between ages 9 and 12, the brain reaches peak maturation of gray and white matter volume, and synapse and neurotransmitter density also increases. The repeated head injuries that can occur during youth football play during this time may disrupt neurodevelopment, with lasting negative effects.
One drawback to the study was that recruitment was not random—men who volunteered for the study might have done so due to a recognition of their own cognitive problems. However, the results suggest more study is needed, and caution is encouraged when making decisions about youth football participation. Some youth football leagues have begun placing greater limits on the type of contact allowed during play.