Sodium Benzoate Helps Treat Schizophrenia When Added to Clozapine
In a 2017 article in the journal Biological Psychiatry, Chieh-Hsin Lin and colleagues reported that sodium benzoate, a common food preservative, may augment the effects of clozapine in patients with schizophrenia.
Clozapine is the most effective antipsychotic available, but as many as 40–70% of patients with treatment-resistant schizophrenia do not respond to it. For those with a poor response to clozapine, sodium benzoate may offer some hope.
In a randomized, double-blind trial, sixty inpatients taking clozapine for schizophrenia were divided into three groups. One group received an additional 1 g/day of sodium benzoate, another received 2 g/day, and the third received placebo in addition to clozapine. Both groups taking sodium benzoate and clozapine showed improvements in negative symptoms of schizophrenia (which can include apathy and inability to experience pleasure) compared to the group taking only clozapine. The larger 2g dose also improved positive symptoms of schizophrenia (such as hallucinations or delusions) and quality of life. Changes in levels of the antioxidant catalase were linked to the total improvement in symptoms and the improvement in positive symptoms. Sodium benzoate did not seem to cause any side effects.
Editor’s Note: Sodium benzoate is a D-amino acid oxidase inhibitor that activates NMDA receptors and increases levels of the amino acid D-serine in the brain by preventing it from breaking down. D-serine can reverse the effects of the illicit drug PCP, and very high doses of D-serine have improved the effectiveness of atypical antipsychotics in people with schizophrenia. By increasing levels of D-serine, sodium benzoate may offer new benefits to people with schizophrenia, especially those who have not responded to other treatments.
Early Intervention Improves Outcomes in Early-Stage Schizophrenia
A recent meta-analysis of 10 studies found that early intervention after a first episode of psychosis or in the early stages of a schizophrenia spectrum disorder led to better patient outcomes than treatment as usual.
The meta-analysis by researcher Christoph U. Correll and colleagues appeared in the journal JAMA Psychiatry in 2018. The 10 studies that were included had randomized a total of 2,176 patients to receive either treatment as usual or early intervention services, which typically include efforts at early detection of symptoms, early treatment with low doses of antipsychotic medication, interventions to prevent relapse, and strategies to help patients return to normal work and social activities.
Those patients who received early intervention services were less likely to discontinue treatment, were less likely to have a psychiatric hospitalization, were more involved in school or work, and had less severe symptoms, including both positive and negative symptoms of schizophrenia.
The authors called for better funding and implementation of early intervention services in early psychosis or the beginning stages of schizophrenia.
Editor’s Note: This finding with regard to schizophrenia spectrum disorders emphasizes the enormous disparity in allocation of research resources for the study of early psychosis versus early bipolar disorder, where almost no studies of this kind have been done.
The mean age of the patients in this psychosis meta-analysis was 27.5 years. Symptoms of bipolar disorder can often begin earlier, in childhood, and early onset of bipolar disorder predicts poor long-term outcomes into adulthood and is associated with a high risk of substance abuse and suicide. This editor (Robert M. Post) and many colleagues have witnessed two decades of scientific literature on early-onset bipolar disorder. We know that early intervention is necessary, but more treatment studies are needed at the early stages of the illness, and calls for funding treatment-focused research have gone unheeded.
More advocacy is needed among families affected by bipolar disorder and advocacy groups interested in better treatment of bipolar disorder. We must try to change the abysmal status quo and campaign publicly, privately, and politically for more funds and public health attention to be directed toward early intervention in bipolar disorder.
Antioxidant N-Acetylcysteine Improves Working Memory in Patients with Psychosis
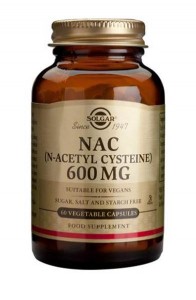 In a 2017 article in the journal Psychological Medicine, researcher Marta Rapado-Castro and colleagues reported that among 58 patients with bipolar disorder or schizophrenia and symptoms of psychosis, those who took two grams per day of the antioxidant n-acetylcysteine (NAC) showed improvements in working memory after six months compared to those who took placebo over the same study period.
In a 2017 article in the journal Psychological Medicine, researcher Marta Rapado-Castro and colleagues reported that among 58 patients with bipolar disorder or schizophrenia and symptoms of psychosis, those who took two grams per day of the antioxidant n-acetylcysteine (NAC) showed improvements in working memory after six months compared to those who took placebo over the same study period.
Antipsychotic medications can typically reduce psychotic symptoms such as delusions or hallucinations, but cognitive symptoms such as problems with learning, memory, or information processing may remain. NAC, which is sold over-the-counter as a nutritional supplement, seemed to improve these symptoms.
The researchers suggest that larger studies of NAC are needed, particularly to determine whether giving NAC to patients during their first episode of psychosis could prevent cognitive decline from occurring at all during the course of their illness.
NAC has been found to have a range of benefits, including reducing substance abuse and interfering with habit-based behaviors such as compulsive hair-pulling, obsessive-compulsive disorder, and gambling.
Researcher Michael Berk, a co-author of the study, reported in the journal Biological Psychiatry in 2008 that NAC could also improve depressive symptoms in bipolar disorder and negative symptoms in schizophrenia.
Editor’s Note: Since cognitive deficits are common in both schizophrenia and bipolar disorder, using NAC in addition to antipsychotic medications could be a useful tool to address these types of symptoms.
Simvastatin Looks Promising in Treatment of Negative Symptoms of Schizophrenia
The statin drug simvastatin (Zocor) enhances the effects of risperidone on negative symptoms of schizophrenia, according to a 2017 article by Soode Tajik-Esmaeeli and colleagues in the journal International Clinical Psychopharmacology.
In the 8-week study, 40 mg/day of simvastatin enhanced the effects of 4–6 mg/day of the antipsychotic risperidone on negative symptoms of schizophrenia, such as apathy and withdrawal, but not positive symptoms such as hallucinations or delusions.
Other statins, lovastatin and pravastatin, have not had a similar effect, possibly because they do not cross the blood-brain barrier as easily as simvastatin does.
Simvastatin has other benefits as well. Like all statins it decreases lipid levels, reducing cardiovascular disease. People with schizophrenia and bipolar disorder are at especially high risk for cardiovascular disease.
Simvastatin also decreases inflammation (lowering IL-1 alpha and TNF-beta levels) and may be neuroprotective, as it increases brain-derived neurotrophic factor (BDNF), a protein that protects neurons and is important for learning and memory. Inflammation is increasingly implicated in schizophrenia and bipolar disorder.
There is also some evidence that statins can prevent depressions over long-term follow-up. Studies in women without depression and men who had recently had heart attacks both showed that those taking statins had a lower rate of future depression than those not taking statins.
Editor’s Note: These findings suggest a potential 5-fold benefit to simvastatin: 1) It reduces negative symptoms in schizophrenia. 2) It reduces inflammation. 3) It increases BDNF. 4) It decreases cardiovascular disease risk by lowering lipid levels. 5) It may prevent future depressions.
Other approaches to augmenting schizophrenia treatment include nutritional supplements vitamin D3 and folate. Patients with psychosis often have vitamin D deficits. Folate supplements can reduce homocysteine, which has been linked to cognitive deficits in schizophrenia.
Liraglutide Decreased Body Weight, Improved Glucose Tolerance and Cardio Health in Schizophrenia
 A 2017 article by Julie R. Larsen and colleagues in the journal Archives of General Psychiatry reported that the drug liraglutide, a treatment for type 2 diabetes, improved certain health measures in people with schizophrenia who were overweight and prediabetic and being treated with the atypical antipsychotics olanzepine or clozapine.
A 2017 article by Julie R. Larsen and colleagues in the journal Archives of General Psychiatry reported that the drug liraglutide, a treatment for type 2 diabetes, improved certain health measures in people with schizophrenia who were overweight and prediabetic and being treated with the atypical antipsychotics olanzepine or clozapine.
In the 16-week trial, patients received a daily 2 mg injection of liraglutide under the skin or placebo. Liraglutide decreased body weight, improved glucose tolerance, and improved cardio-metabolic measures. Weight decreased by more than 10 pounds on average compared to placebo.
Liraglutide is derived from a human metabolic hormone. It binds to the same receptors as does the metabolic hormone GLP-1, which stimulates insulin secretion.
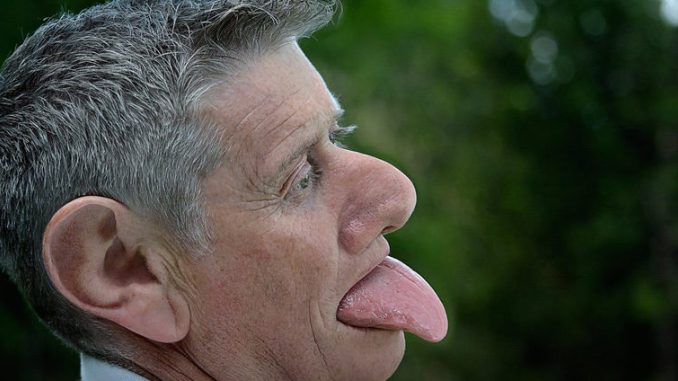
FDA Approves New Higher Dose of Valbenazine for Tardive Dyskinesia
The US Food and Drug Administration has approved an 80 mg capsule dose of valbenazine (Ingrezza) for tardive dyskinesia (jerky, involuntary movements of the face, especially the mouth and tongue, fingers and body that can be a side effect of antipsychotic medication). Valbenazine, a selective vesicular monoamine transporter 2 inhibitor, was the first drug FDA-approved for tardive dyskinesia. The FDA initially approved a dosage of 40 mg/day in April 2017. The 80 mg/day dose was approved in October 2017.
The new approval was based on a 6-week clinical trial in which 80 mg of valbenazine improved tardive dyskinesia significantly compared to placebo. Improvement continued over 48 weeks of treatment.
Augmentation Strategies for Negative Symptoms of Schizophrenia
In a 2017 article in the journal JAMA Psychiatry, Christoph U. Correll and colleagues reviewed 42 secondary strategies to treat schizophrenia when the primary antipsychotic treatment has an incomplete effect. Many people with schizophrenia show only a limited response to antipsychotic drugs, so additional treatments are often necessary, but currently there are no US Food and Drug Administration guidelines for combination treatment.
Correll and colleagues compiled data from 29 meta-analyses covering 381 individual trials. They found that while the meta-analyses were well done, the quality of the data in the original studies was lacking.
Focusing on Negative Symptoms
However, since the negative symptoms of the illness such as apathy, withdrawal, and blunted emotional response are the hardest to treat, any amount of improvement in this area could be particularly helpful. Read more
Safety of Atypical Antipsychotics in Pregnancy
A 2017 article in the Journal of Clinical Psychiatry systematically reviewed data on the risks related to schizophrenia, bipolar disorder, and treatment with atypical antipsychotic medication during pregnancy. The article by researcher Sarah Tosato and colleagues suggests that a mother’s illness may be more harmful to a fetus than treatment for that illness is.
The review analyzed 49 articles about illness-related and atypical antipsychotic–related risks in bipolar disorder and schizophrenia. Tosato and colleagues found that abrupt discontinuation of treatment led to a high risk of relapse in pregnant women with bipolar disorder or schizophrenia.
Schizophrenia was linked to a slight increase in obstetric complications for mothers, while both bipolar disorder and schizophrenia were linked to a slight increase in complications for newborns. Mothers ill with schizophrenia had the highest risk for serious complications, including stillbirth, neonatal or infant death, and intellectual disability in the child.
The researchers reported that untreated bipolar disorder and schizophrenia are risk factors for birth defects, but use of atypical antipsychotics is not. Children’s neurodevelopment also does not seem to be affected by mothers’ use of atypical antipsychotics during pregnancy.
The authors suggest that, given parents agree and understand any risks involved, the least harmful choice of action is to maintain treatment of women with bipolar disorder and schizophrenia during pregnancy at the safest minimum dosage to keep their illness at bay.
Dutch Study Links Low Vitamin D to Bipolar Disorder
A 2016 study in the Netherlands found that people with bipolar disorder are more likely to have vitamin D deficiency than the general population. Vitamin D deficiency has been linked to other psychiatric disorders including schizophrenia and unipolar depression. Poor diet and lack of exposure to sunlight can put someone at risk for vitamin D deficiency.
The study, led by Remco Boerman and published in the Journal of Clinical Psychopharmacology, included 118 adults with bipolar disorder, 149 with schizophrenia, and 53 with schizoaffective disorder. More than 30% of these participants had deficient levels of vitamin D. Only 15% had optimum levels of the vitamin. More than 22% of the participants with bipolar disorder were deficient in vitamin D, while close to 35% of those with schizophrenia and schizoaffective disorder were deficient.
Study participants had vitamin D levels that were 25% lower than those of the white Dutch population, and vitamin D deficiency was 4.7 times more common in those with psychiatric disorders than the general Dutch population.
The authors suggested screening people with bipolar disorder, schizophrenia, and schizoaffective disorder for low levels of vitamin D.
FDA Approves Treatment for Tardive Dyskinesia
 A new drug valbenazine (trade name Ingrezza) has been approved by the US Food and Drug Administration for the treatment of tardive dyskinesia. Tardive dyskinesia, a side effect of long-term use of antipsychotic medication, consists of involuntary movements of the tongue, face, torso, arms, and legs. It can interfere with walking, talking, and breathing.
A new drug valbenazine (trade name Ingrezza) has been approved by the US Food and Drug Administration for the treatment of tardive dyskinesia. Tardive dyskinesia, a side effect of long-term use of antipsychotic medication, consists of involuntary movements of the tongue, face, torso, arms, and legs. It can interfere with walking, talking, and breathing.
The approval followed 20 clinical trials of valbenazine that included a total of more than 1000 participants who had symptoms of tardive dyskinesia in addition to schizophrenia, schizoaffective disorder, or bipolar disorder.
In a 2017 article in the American Journal of Psychiatry, researcher Robert A. Hauser and colleagues reported that patients who received 80 mg/day of valbenazine had a significant reduction in tardive dyskinesia symptoms after six weeks compared to those who received placebo. Participants who received 40 mg/day of valbenazine also had reductions in symptoms, although not as dramatic as with the higher dose.
Serious side effects of valbenazine include sleepiness and lengthening of the QT interval, which can increase heart arrhythmias. The FDA notes that people who already have abnormal heartbeats due to a long QT interval should not take valbenazine. In addition, people taking the drug should avoid driving or operating heavy machinery until they know how valbenazine affects them.