Hormone Replacement With Estrogen/Progestogen Combo Increases Breast Cancer Risk More Than Once Thought
A 2016 article in the British Journal of Cancer suggests that previous studies underestimated breast cancer risk in women who received hormone replacement therapy with the combination of estrogen and progestogen. The article by researcher Michael E. Jones and colleagues reported that combined hormone replacement therapy could increase the risk of breast cancer by more than three times, depending on how long a woman is exposed to the therapy. The longer the duration of use, the greater the risk of breast cancer. In the study, women who used other types of hormone replacement therapy, such as estrogen only or tibolone, did not have drastically higher rates of breast cancer than had been reported before.
Jones and colleagues suggest that previous studies did not use long enough follow-up periods to track whether women developed breast cancer while using hormone replacement. Their own study is based on a United Kingdom dataset known as the Breakthrough Generations Study. Study participants completed questionnaires at 2.5 years after recruitment, again at around 6 years, and again around 9.5 years. At the time of recruitment, women using combination hormone replacement therapy had been doing so for a median of 5.5 years.
Women who used combination hormone replacement therapy for 5.4 years were 2.74 times likelier to have breast cancer than those who didn’t receive hormone replacement. Using the combined therapy for more than 15 years increased risk 3.27 times compared to non-users.
The study also reported that as body mass index increased, breast cancer risk increased, regardless of hormone use.
While the study by Jones and colleagues was large (39,183 participants), the number of women who took combined hormone replacement and developed breast cancer was still fairly small (52). Seven of the 52 had taken the combined pill for more than 15 years. One limitation of this study is that these seven women may have skewed the risk assessments somewhat.
Experts suggest that women balance the possible risks and benefits of hormone replacement therapy. The therapy can be helpful in reducing symptoms of menopause, particularly hot flashes.
Using the lowest effective dose for the shortest time possible may be the best option. The increased risk of breast cancer drops after a woman stops using hormone replacement.
Use of Hormonal Contraceptives May Increase Depression Risk in Young Women
Women, particularly adolescent women, are at increased risk of developing depression if they use hormonal contraceptives, according to a 2016 study in the journal JAMA Psychiatry. The study by Charlotte Wessel Skovlund and colleagues used data from a Danish registry of more than one million women between the ages of 15 and 34 who had no history of depression or other psychiatric disorders. During follow-up (which lasted an average of 6.4 years), 55% of the women were using or had recently used hormonal contraceptives. These women were more likely to be prescribed an antidepressant for the first time, and more likely to be diagnosed with depression compared to women who did not use hormonal contraceptives.
The increased risk of being prescribed an antidepressant varied by contraceptive type. The norgestrolmin patch increased risk by 2.0 times, and the etonogestrel vaginal ring did so by 1.6 times. The levonorgestrel intrauterine device (IUD) made an antidepressant prescription 1.4 times more likely. Progestin-only pills increased risk by 1.34 times and combined oral contraceptive pills increased it by 1.23 times compared to women who did not use oral contraceptives.
The relative risk peaked at around six months after starting hormonal contraceptives.
Patients aged 15–19 were particularly vulnerable to depression. The likelihood of receiving an antidepressant prescription was 1.8 times higher in teens taking combined pills, 2.2 times higher in those taking progestin-only pills, and 3 times higher in teens using hormonal methods of birth control that are not delivered orally compared to those who did not use hormonal contraceptives at all.
Women with History of Depression 20 Times More Likely To Have Postpartum Depression
 A study of almost all women who gave birth in Sweden between 1997 and 2008 reports that women with a history of depression are 21.03 times more likely to suffer from postpartum depression than those without such a history. The 2017 article by Michael E. Silverman and colleagues in the journal Depression and Anxiety reports that advanced age and gestational diabetes also increased the likelihood of postpartum depression.
A study of almost all women who gave birth in Sweden between 1997 and 2008 reports that women with a history of depression are 21.03 times more likely to suffer from postpartum depression than those without such a history. The 2017 article by Michael E. Silverman and colleagues in the journal Depression and Anxiety reports that advanced age and gestational diabetes also increased the likelihood of postpartum depression.
Whether a woman had gone through a depression in the past also affected her other risk factors for postpartum depression. Among women who had been depressed before, having diabetes before pregnancy and having a “mild” pre-term delivery were risk factors for postpartum depression. In contrast, among women with no history of depression, young age, having an instrument-assisted or caesarean delivery, and “moderate” pre-term delivery were risk factors for postpartum depression.
Rates of postpartum depression decreased one month after delivery.
Editor’s Note: About one in five women in the general population experience postpartum depression. All new mothers should be screened for postpartum depression, but especially those with a history of depression. Instituting supportive measures may help prevent an episode.
Safety of Atypical Antipsychotics in Pregnancy
A 2017 article in the Journal of Clinical Psychiatry systematically reviewed data on the risks related to schizophrenia, bipolar disorder, and treatment with atypical antipsychotic medication during pregnancy. The article by researcher Sarah Tosato and colleagues suggests that a mother’s illness may be more harmful to a fetus than treatment for that illness is.
The review analyzed 49 articles about illness-related and atypical antipsychotic–related risks in bipolar disorder and schizophrenia. Tosato and colleagues found that abrupt discontinuation of treatment led to a high risk of relapse in pregnant women with bipolar disorder or schizophrenia.
Schizophrenia was linked to a slight increase in obstetric complications for mothers, while both bipolar disorder and schizophrenia were linked to a slight increase in complications for newborns. Mothers ill with schizophrenia had the highest risk for serious complications, including stillbirth, neonatal or infant death, and intellectual disability in the child.
The researchers reported that untreated bipolar disorder and schizophrenia are risk factors for birth defects, but use of atypical antipsychotics is not. Children’s neurodevelopment also does not seem to be affected by mothers’ use of atypical antipsychotics during pregnancy.
The authors suggest that, given parents agree and understand any risks involved, the least harmful choice of action is to maintain treatment of women with bipolar disorder and schizophrenia during pregnancy at the safest minimum dosage to keep their illness at bay.
Birth Defects from Valproate Lower in Bipolar Disorder than in Epilepsy
 The anticonvulsant valproate increases the risk of serious birth defects in fetuses exposed to it. However, a 2017 report by ANSM, France’s agency for health and product safety, and its national insurance fund for employed workers shows that these risks are lower for women taking valproate for bipolar disorder than for women taking valproate for epilepsy.
The anticonvulsant valproate increases the risk of serious birth defects in fetuses exposed to it. However, a 2017 report by ANSM, France’s agency for health and product safety, and its national insurance fund for employed workers shows that these risks are lower for women taking valproate for bipolar disorder than for women taking valproate for epilepsy.
In France, the risk of a major fetal malformation was 10.2 per 1000 women in the general population, about twice that (22.2 per 1000) in women taking valproate for bipolar disorder, and about 4 times higher (46.5 per 1000) in women taking valproate for epilepsy. The authors suggest that treatment for bipolar disorder may be more likely to be interrupted during pregnancy, and this could explain the different levels of risk by diagnosis.
Among the risks of defects in the fetuses of women being treated with valproate for epilepsy, the risk of a ventricular septal defect (a hole in the wall separating the lower heart chambers) was 11.2% compared to 2.7% in fetuses not exposed to valproate, while risk of an atrial septal defect (a hole in the wall separating the upper heart chambers) was 19.1% in the fetuses of those prescribed valproate for epilepsy compared to 1.9% in unexposed fetuses. Risk of hypospadias (placement of the urethra opening on the underside of the penis rather than its end) was 22.7% compared to 4.8% in the general population.
Risks of a major malformation were dose dependent in those with epilepsy (but interestingly, not in those with bipolar disorder), meaning the more valproate patients with epilepsy took, the higher their risk of a fetus with birth defects.
The only birth defects that were more common in the fetuses of women taking valproate for bipolar disorder than in fetuses not exposed to valproate were hypospadias (17.5% risk compared to 4.8% in the general population) and craniostenosis, a deformity of the skull (4.2% risk compared to 0.4% in the general population).
The relative safety of valproate in women being treated for bipolar disorder compared to those being treated for epilepsy is good news for some. However, fetal exposure to valproate has also been linked to deficits in cognitive development.
The risk of spina bifida, which causes lifetime paralysis, in a fetus may no longer be such a catastrophic issue for women taking valproate for bipolar disorder (where the risk did not exceed that of the general population), as was once assumed based on data from women with epilepsy (where the risk is usually 2-4%, but was 8% in this French study). This may be of some comfort to women with bipolar disorder who require valproate treatment to remain stable and wish to become pregnant or in those who experience an unplanned pregnancy.
Antidepressant Use in Pregnancy Does Not Increase Autism Risk
 Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
One of the studies, by researcher Ayesha C. Sujan and colleagues, analyzed exposure to antidepressants in the first trimester and neurodevelopmental outcomes in almost 1.6 million Swedish children. Antidepressant use did slightly increase the chance of a preterm birth, but was not linked to autism spectrum disorder, attention-deficit hyperactivity disorder (ADHD), or small size of the fetus.
The researchers suggested that doctors and patients work together to decide how depression should be treated during pregnancy, based on severity of the depression, treatment history, and access to services.
The other study, by researcher Hilary K. Brown and colleagues, analyzed 36,000 births in Ontario, Canada and found no increased risk of autism spectrum disorder based on antidepressant exposure in utero. The study controlled for 500 characteristics such as mother’s education, age, and health history.
The journal JAMA Pediatrics also published a meta-analysis and review of 10 studies on the subject, finding that a woman’s history of psychiatric disorders weakened any link between antidepressant use during pregnancy and risk of autism spectrum disorder in her children. This implies that the underlying illness, not its treatment, may be responsible if there is any link between depression and autism. The meta-analysis was carried out by researcher Antonia Mezzacappa and colleagues.
Breathing in Through the Nose Enhances Judgment and Memory
A 2016 study published in the Journal of Neuroscience reported that the rhythm of breathing changes electrical activity in the brain and can improve emotional judgments and recall. Breathing in through the nose seemed to produce benefits compared to breathing out or to breathing in through the mouth.
Participants more easily identified a fearful face if they viewed it while breathing in. They also had an easier time remembering objects they observed while breathing in. The effects were not seen if the participants breathed through their mouth.
The researchers, led by Christina Zelano, reported that there was a major difference in brain activity in the amygdala and hippocampus during inhalation versus exhalation. Breathing in, in addition to stimulating the olfactory cortex responsible for smell perception, seems to activate the entire limbic system, the emotional center of the brain.
Breathing-Focused Yoga and Meditation Improved Depression
A 2016 article in the Journal of Clinical Psychiatry reports that Sudarshan Kriya yoga, a breathing-based meditation intervention, improved depression in people who had had an inadequate response to antidepressants.
In the study by researcher Anup Sharma and colleagues, 25 participants were randomized to either receive the breathing-based meditation training right away or be put on a waitlist to receive the training later. After two months, those who received the intervention showed improvement in depression scores compared to those on the waitlist. The intervention also reduced anxiety.
Following Collisions, High School Football Players with No Signs of Concussion May Still Have Neurological Impairment
In a small 2014 study in the Journal of Neurotrauma, researcher Thomas M. Talavaga and colleagues reported that repeated head trauma that did not produce concussion symptoms was still associated with neurocognitive and neurophysiological changes to the brain in high school football players.
The longitudinal study tracked ‘collision events’ experienced by 11 teens who played football at the same high school. The young men also completed neurocognitive testing and magnetic resonance imaging (MRI) scans of their brains over time.
The researchers expected to see the participants fall into two categories: those who had no concussions and normal neurological function, and those who had at least one concussion and subsequent neurological changes. They ended up observing a third group: young men who had not exhibited concussion symptoms, but nonetheless had measurable changes to their neurological functioning, including impairments to visual working memory and altered activation of the dorsolateral prefrontal cortex. Young men in this last group had had more collisions that impacted the top front of the head, directly above the dorsolateral prefrontal cortex.
The authors suggest that the discovery of this third category mean that some neurological injuries are going undetected in high school football players. The players who are injured in this way are not likely to seek treatment, and may continue playing football, risking more neurological brain injury or brain damage with subsequent collisions.
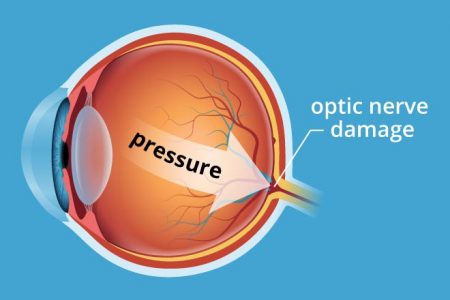
In Mice, Vitamin B3 (Niacin) Prevents Glaucoma
A study published in the journal Science in 2017 reports that adding vitamin B3 to the drinking water of mice prevented them from developing glaucoma. Glaucoma is an age-related condition in which pressure inside the eye damages retinal ganglion cells, the neuronal cells that connect the eye to the brain.
Age contributes both to the buildup of pressure within the eye and to the vulnerability of the neuronal cells to damage. Vitamin B3 seemed to correct the latter problem.
The study by Pete A. Williams and colleagues compared mice with an inherited risk of glaucoma to control mice. Williams and colleagues found that a molecule called NAD that keeps cells functioning normally declined with age, reducing the reliability of the neurons’ energy metabolism.
Vitamin B3 boosted the metabolic reliability of the aging neuronal cells. This helped the cells resist damage from mounting pressure in the eye.
Williams and colleagues also found that a single application of gene therapy with the gene NMNAT1 also prevented glaucoma in the mice. NMNAT1 is the gene for an enzyme that makes NAD from vitamin B3. Gene therapy via an injection in the eye has been approved to treat some rare human eye disorders.
The researchers hope to eventually test vitamin B3 treatment in people with glaucoma and other neurodegenerative disorders.
Editor’s Note: Vitamin B3 may be beneficial for other conditions as well. High-dose niacin (500 mg and up) is a prescription treatment for high cholesterol, and especially the combination of high cholesterol and high triglycerides (blood fats). Niacin may also prevent hardening of the arteries and second heart attacks in men with heart or circulatory problems, and improve diabetes (type 1 and 2). There is some evidence that vitamin B3 can also improve symptoms of osteoarthritis, such as joint stiffness, pain, and swelling. In addition, people who consume more niacin have a lower risk of Alzheimer’s disease, though it is not clear that taking niacin supplements can prevent the illness.