Evidence-Based Psychotherapies for Young Children
 As many as 7–10% of children under the age of 5 have mood or behavioral problems, and this risk is even higher when a parent has a mood disorder. However, many families are not able to access treatment for these children due to their location, a lack of providers, or insurance problems.
As many as 7–10% of children under the age of 5 have mood or behavioral problems, and this risk is even higher when a parent has a mood disorder. However, many families are not able to access treatment for these children due to their location, a lack of providers, or insurance problems.
A 2016 article by Mary Margaret Gleason and colleagues in the journal Technical Report in Pediatrics summarizes psychotherapeutic treatments for children that are supported with rigorous evidence. Some of these include infant-parent psychotherapy, video feedback for positive parenting, attachment biobehavioral catch-up (or ABC, in which caregivers are taught to re-interpret the signals of children who previously experienced maltreatment, providing nurturing in response), parent-child interaction therapy, and programs that combine parenting support with illness prevention, such as the Incredible Years series (for behavioral difficulties), the New Forest Programme (for attention-deficit hyperactivity disorder or ADHD), and Helping the Noncompliant Child (for oppositional behavior).
Gleason and colleagues suggest that pediatricians should take the lead in assessing young children and recommending appropriate psychotherapeutic approaches.
One resource available to parents is our own Child Network. It consists of an online portal where parents can provide weekly ratings of their children’s symptoms. These can be provided to the child’s physician to facilitate diagnosis and to clinicians to more effectively evaluate the results of treatment. The data provided to the Child Network will in turn help us understand how children are being treated in the community. There a few initial forms to fill out, but the weekly rating process is quick and can provide a great picture of a child’s wellbeing over time, including evaluating the effectiveness of any treatments.
Offspring of Bipolar Parents Have More Psychiatric Illness
 A 2017 study from the Czech Republic found that children and adolescents with at least one parent with bipolar disorder had much higher lifetime rates of mood and anxiety disorders than their peers who did not have a parent with bipolar disorder. The offspring of bipolar parents also had lower quality of life, less social support, poorer self-perception, poorer relationships with their peers and parents, and more difficult home lives than those whose parents did not have bipolar disorder.
A 2017 study from the Czech Republic found that children and adolescents with at least one parent with bipolar disorder had much higher lifetime rates of mood and anxiety disorders than their peers who did not have a parent with bipolar disorder. The offspring of bipolar parents also had lower quality of life, less social support, poorer self-perception, poorer relationships with their peers and parents, and more difficult home lives than those whose parents did not have bipolar disorder.
The study by Michal Goetz and colleagues in the Journal of Child and Adolescent Psychopharmacology reported that 86% of the children of bipolar parents would be diagnosed with a psychiatric disorder in their lifetime. Similarly, David Axelson and colleagues from the Pittsburgh Bipolar Offspring Study reported in the American Journal of Psychiatry in 2015 that 74.2% of children with a parent with bipolar disorder would receive a lifetime psychiatric diagnosis, and a 2006 study by Myrna M. Weissman in the American Journal of Psychiatry found that the offspring of a unipolar depressed parent were three times more likely to have a psychiatric illness than offspring of nondepressed parents over 20 years of follow-up. Another study by this editor (Robert M. Post) and colleagues in the Bipolar Collaborative Network published in the Journal of Affective Disorders in 2016 found that a third of children at high risk due to a parent’s bipolar diagnosis would go on to have a psychiatric illness.
The Goetz study included a total of 86 participants between the ages of 7 and 18. Half had a parent with bipolar disorder and half did not. One limitation of the study was its recruitment procedure. Parents with bipolar disorder who enrolled their children in the study may have done so out of concern for their offspring’s mental health, increasing illness rates in the group with bipolar parents. Researchers were also aware of parents’ diagnoses, which may have affected their ratings of the young people’s symptoms. Despite these limitations, the study and its predecessors still suggest that psychiatric illness in a parent puts children at very high risk for a psychiatric illness themselves and can affect their wellbeing in a variety of ways.
Goetz and colleagues suggest that there is a need for proactive and complex care of families with psychiatric illness. They suggest that good communication is needed between adult and youth psychiatric services, with physicians who treat adults with bipolar disorder inquiring about those patients’ children and referring them to specialized psychiatric services for youth.
Editor’s Note: I not only endorse the conclusions of Goetz and colleagues, but would further recommend that parents with a diagnosis of bipolar disorder or unipolar depression discuss their children’s mood and behavior with their own psychiatrists and the children’s primary care physicians.
Parents of children aged 2 to 12 may enroll in our own Child Network, a secure online portal where they can record weekly ratings of their children’s symptoms and share these with their physicians.
There are many effective psychotherapeutic interventions for children with anxiety and mood disorders that should be sought for a child with symptoms that impair his or her functioning. Two evidence-based treatments are Family Focused Therapy, which incorporates family members into treatment so that they better understand the illness and can be supportive of the affected child, and cognitive behavioral therapy, in which negative patterns of thoughts and behaviors are challenged and patients are taught more effective problem-solving skills. When childhood psychiatric illness is recognized and treated appropriately, the results are often excellent, and it is possible that heading off the illness early may even prevent the development of more severe illness later in the child’s life.
Generic Seroquel XR Approved
 Earlier this year, the US Food and Drug Administration approved a generic version of Seroquel XR tablets (Quetiapine Fumarate Extended-Release Tablets), which are used to treat both depression and mania in bipolar disorder, schizophrenia, and to augment the effects of antidepressants in unipolar depression. Also known as quetiapine, the generic tablets will be available in 50 mg, 150 mg, 200 mg, 300 mg, and 400 mg doses.
Earlier this year, the US Food and Drug Administration approved a generic version of Seroquel XR tablets (Quetiapine Fumarate Extended-Release Tablets), which are used to treat both depression and mania in bipolar disorder, schizophrenia, and to augment the effects of antidepressants in unipolar depression. Also known as quetiapine, the generic tablets will be available in 50 mg, 150 mg, 200 mg, 300 mg, and 400 mg doses.
Seroquel XR is taken once per day several hours before bedtime in the acute treatment for bipolar depression (300 mg/day), mania or mixed episodes (300–600 mg/day) or their prevention (400 mg/day); or paired with antidepressants to treat unipolar depression (150–300 mg/day).
The generic tablets, which are expected to be more affordable than Seroquel XR, are produced by Pharmadax Inc.
Untreated Episodes of Bipolar Disorder Worsen Over Time, But Prevention is Possible
A 2017 literature review by researcher Lars V. Kessing and Per K. Andersen in the journal Acta Psychiatrica Scandinavica reports that the greater a patient’s number of previous episodes of bipolar disorder, the more likely that patient is to have a more difficult course of illness and poorer outcomes. The number of episodes was associated with more rapid recurrences, duration and severity of episodes, more automatic episodes (i.e. not triggered by stress), risk of dementia, treatment resistance, lack of recovery between episodes, and brain volume losses.
In an article in the journal Bipolar Disorders in 2016, BNN Editor-in-Chief Robert M. Post described the value of preventive treatment in reducing episodes and protecting the brain from the damage that accompanies them.
Given that episodes, stressors, and bouts of substance abuse can affect the way genes are transcribed via a phenomenon known as epigenetics, preventing these occurrences could lead to an easier course of illness and improved outcomes. Patients should provide their physicians with feedback about their response to prior medications and any side effects they experience over time so that their medication regime can be adjusted until it is maximally effective.
Patients with severe illness and multiple previous episodes may need a complex medication regimen that includes multiple types of medications that target different systems of neurotransmitters.
This philosophy of treatment is presented in several publications, including the 2008 book Treatment of Bipolar Illness: A Casebook for Clinicians and Patients by Post and Gabrielle Leverich, and more recently in the article “Treatment of Bipolar Depression: Evolving Recommendations” in the journal Psychiatric Clinics of North America. An open access article by Post, “New Perspectives on the Course and Treatment of Bipolar Disorders,” published in the journal Edizioni Minerva Medica S.p.A. in 2017, describes the need for early and sometimes complex combination therapy, including the non-intuitive idea that more medications (carefully prescribed) can actually produce fewer side effects than large doses of a single medication.
Another good resource for patients is a daily personal calendar that can be used to track ongoing symptoms, side effects, and response to medications. We offer several types of these calendars free here. My Mood Monitor, or What’s My M3, is a validated screening instrument that can detect depression, anxiety disorders, and mania in response to weekly self-reports. It is available online and as an app, and can be used to track illness course and response to treatment.
Systematic Review Finds Bupropion is Effective for ADHD in Young People
 A 2016 systematic review by Qin Xiang Ng in the Journal of Child and Adolescent Psychopharmacology found that the antidepressant bupropion (Wellbutrin) can improve attention deficit hyperactivity disorder (ADHD) in children and adolescents.
A 2016 systematic review by Qin Xiang Ng in the Journal of Child and Adolescent Psychopharmacology found that the antidepressant bupropion (Wellbutrin) can improve attention deficit hyperactivity disorder (ADHD) in children and adolescents.
The review identified 25,455 studies of bupropion for ADHD, but only six included children. All six studies showed that bupropion improved ADHD symptoms in children and adolescents. Head-to-head trials of bupropion and methylphenidate (one of the most common medications to treat ADHD, which most people know by the name Ritalin) found the drugs had similar efficacy rates, although a large double-blind, placebo-controlled multicenter study found that bupropion had a smaller effect size than methylphenidate.
In terms of side effects, methylphenidate was more likely to cause headaches than bupropion, but otherwise the drugs were similar.
Ng suggests that bupropion should be considered for the treatment of ADHD in children and adolescents, but more large trials of the drug are needed. Bupropion may also help children whose ADHD appears alongside conduct, substance abuse, or depressive disorders.
Short Telomeres Associated with Family Risk of Bipolar Disorder
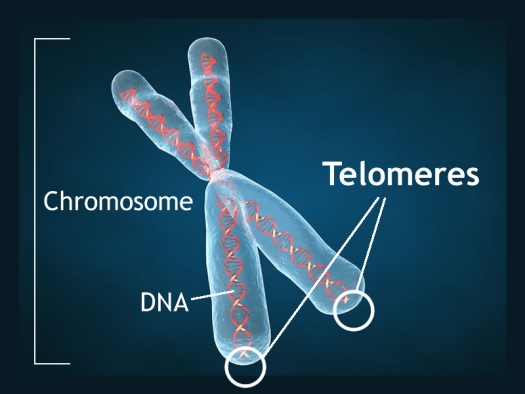
Telomeres are bits of genetic material at the end of each strand of DNA that protect chromosomes as they replicate. Short telomeres have been linked to aging and a variety of medical and psychiatric diseases. Stress and depressive episodes can shorten telomeres, while treatment with lithium can lengthen them.
Telomere length is a heritable trait, and a 2017 study by researcher Timothy R. Powell and colleagues suggests that shorter telomeres are a familial risk factor for bipolar disorder.
The study, published in the journal Neuropsychopharmacology, compared the telomere lengths of 63 people with bipolar disorder, 74 of their immediate relatives (49 of whom had no lifetime psychiatric illness, while the other 25 had a different mood disorder), and 80 unrelated people with no psychiatric illness. The well relatives of the people with bipolar disorder had shorter telomeres than the unrelated healthy volunteers.
Relatives (both well and not) and people with bipolar disorder who were not being treated with lithium both had shorter telomeres than people with bipolar disorder who were being treated with lithium.
Another finding was that longer telomeres were linked to greater volume of the left and right hippocampus, and improved verbal memory on a test of delayed recall. This study provides more evidence that taking lithium increases the volume of the hippocampus and has neuroprotective benefits for people with bipolar disorder.
Traumatic Events in Childhood Linked to Shorter Telomeres
Telomeres are bits of DNA at the end of chromosomes that protect the DNA as it replicates. Shorter telomeres have been linked to aging and increases in multiple types of medical and psychiatric disorders. A 2016 article in PNAS, the Proceedings of the National Academy of Sciences of the United States of America, reported that cumulative life adversity and particularly stressful or traumatic events in childhood, predict shorter telomere length.
The study by Eli Puterman and colleagues included 4,590 individuals from the US Health and Retirement Study who reported stressful events that had experienced. A single experience of adversity was not linked to short telomeres, but lifetime cumulative adversity predicted 6% greater odds of having shorter telomeres. This result was mainly explained by adversity that occurred in childhood. Each stressful or traumatic event in childhood increased the odds of short telomeres by 11%. These were mostly social or traumatic experiences rather than financial stresses.
Some Antacids Cause Kidney Damage with No Prior Symptoms
 Commonly used antacids such as Prevacid, Nexium, Prilosec, and Protonix can impair kidney function, according to a 2017 article in the journal Kidney International. These drugs, known as proton pump inhibitors or PPIs, should not be taken long-term without monitoring of kidney function. Other antacids that work by blocking histamine H2 receptors do not interfere with kidney function but may not work as well as PPIs.
Commonly used antacids such as Prevacid, Nexium, Prilosec, and Protonix can impair kidney function, according to a 2017 article in the journal Kidney International. These drugs, known as proton pump inhibitors or PPIs, should not be taken long-term without monitoring of kidney function. Other antacids that work by blocking histamine H2 receptors do not interfere with kidney function but may not work as well as PPIs.
Researcher Yan Xie and colleagues found that more than half of people who developed chronic kidney damage while taking PPIs showed no earlier acute signs of kidney dysfunction, meaning there may not be signs of kidney function loss until the damage is irreversible. Xie and colleagues suggest that patients and doctors should be more vigilant about monitoring the use of these medications, since waiting for outward signs of declining kidney function is not a reliable way of detecting damage.
More than 15 million Americans use prescription PPIs to reduce gastric acid, bringing relief to heartburn, ulcers, and acid reflux. Millions more buy PPIs over the counter without consulting a doctor about their use.
The study analyzed Department of Veterans Affairs data from 125,596 new users of PPIs and 18,436 new users of H2 blockers. Acute, reversible symptoms of kidney damage, such as reduction in the urine being cleared from the body, fatigue, and swelling of the legs and ankles were seen in less than 20% of the PPI users. However, more than half of those who developed chronic kidney damage and end-stage renal disease never showed these warning signals beforehand. In contrast, only 7.67% of those taking H2 blockers had chronic kidney disease without acute symptoms, and 1.27% had end-stage renal disease, when kidneys can no longer clear waste from the body, and dialysis or a kidney transplant is required.
Xie and colleagues suggest carefully monitoring kidney function in people taking PPIs, even when there are no outward signs of problems. They also suggest carefully evaluating whether PPIs are necessary, since the risk of kidney damage is serious.
Methylphenidate Does Not Cause Mania When Taken with a Mood Stabilizer
 Methylphenidate is an effective treatment for attention-deficit hyperactivity disorder (ADHD). Ritalin may be the most commonly recognized trade name for methylphenidate, but it is also sold under the names Concerta, Daytrana, Methylin, and Aptensio. A 2016 article in the American Journal of Psychiatry reports that methylphenidate can safely be taken by people with bipolar disorder and comorbid ADHD as long as it is paired with mood-stabilizing treatment.
Methylphenidate is an effective treatment for attention-deficit hyperactivity disorder (ADHD). Ritalin may be the most commonly recognized trade name for methylphenidate, but it is also sold under the names Concerta, Daytrana, Methylin, and Aptensio. A 2016 article in the American Journal of Psychiatry reports that methylphenidate can safely be taken by people with bipolar disorder and comorbid ADHD as long as it is paired with mood-stabilizing treatment.
The study was based on data from a Swedish national registry. Researchers led by Alexander Viktorin identified 2,307 adults with bipolar disorder who began taking methylphenidate between 2006 and 2014. Of these, 1,103 were taking mood stabilizers including antipsychotic medications, lithium, or valproate, while 718 were not taking any mood stabilizing medications.
Among those who began taking methylphenidate without mood stabilizers, manic episodes increased over the next six months. In contrast, patients taking mood stabilizers had their risk of mania decrease after beginning treatment with methylphenidate.
Viktorin and colleagues suggest that 20% of patients with bipolar disorder may also have ADHD, so it is not surprising that 8% of patients with bipolar disorder in Sweden receive a methylphenidate prescription.
Mood-stabilizing drugs can worsen attention and concentration, so methylphenidate treatment can be helpful if it can be done without increasing manic episodes. However, Viktorin and colleagues suggest that due to the risk of increasing mania, anyone given a prescription for methylphenidate monotherapy should be carefully screened to rule out bipolar disorder.
The researchers confirmed that taking methylphenidate for ADHD while taking a mood stabilizer for bipolar disorder is a safe combination.
Alterations in Amino Acids in Blood That Affect Metabolism May Help Explain Chronic Fatigue
Chronic fatigue syndrome, more recently known as myalgic encephalopathy, is a debilitating and somewhat mysterious illness. However, a 2016 article in the Journal of Clinical Investigation Insight suggests that low blood levels of amino acids related to oxidative metabolism, the process by which oxygen is used to make energy from sugars, may play a role in the illness. High levels of amino acids related to the breakdown of proteins were also seen.
The study by Øystein Fluge and colleagues compared blood concentrations of 20 amino acids in 200 patients with chronic fatigue and 102 healthy participants. There were shortages in 6 amino acids that fuel oxidative metabolism in those with chronic fatigue, particularly women. Men with chronic fatigue had high levels of a different amino acid related to protein catabolism, the breaking down of complex molecules, a process that releases energy.
The differences between men and women with the illness might be because men use muscle tissue as a source for amino acids, while women, who have less muscle mass, use amino acids from blood as fuel.
The changes in both sexes suggest a functional impairment in pyruvate dehydrogenase (PDH), an enzyme that is important for the conversion of carbohydrates into energy. If PDH fails to work and cells turn elsewhere to create energy, muscles may suddenly weaken and lactate may build up, which patients experience as a burning in their muscles after the slightest exertion.
Fluge and colleagues are cancer researchers. They stumbled into chronic fatigue research when they noticed that people with chronic fatigue who were treated for cancer with the drug rituximab saw reductions in their fatigue. Rituximab, which is also used to treat some autoimmune diseases, is a monoclonal antibody directed at B cells. When it binds, it induces cell death. The researchers hope to clarify the link between the immune system and the problems with energy metabolism they have identified in people with chronic fatigue.