The Risk-Benefit Ratio Encourages the Use of Antidepressants in Unipolar Depression
Wednesday we reviewed new data that shows that despite the FDA warning that antidepressants can increase suicidal ideation among young people in the first few months they are taken, antidepressants actually reduce acute suicidal ideation and decrease suicidal acts. As we described last year in our article on five myths about antidepressants, antidepressant treatment in recurrent unipolar depression is important to patients’ long-term wellbeing, cognitive functioning, and even life expectancy.
Untreated depression, and particularly untreated recurrent depression, carries high risks not only for lethality by suicide, but also for increases in medical mortality, particularly from cardiovascular disease. In addition to these medical risks, data from many studies suggest that a higher number of prior depressions is associated with increased cognitive dysfunction, and recent large data sets from a case registry in Denmark indicate that patients with four or more prior unipolar or bipolar depressive episodes have double the risk of receiving a diagnosis of dementia in old age. Thus, depressions are dangerous for a patient’s psychological, medical, and cognitive health.
Antidepressants Are Highly Effective in Depression Prevention
In 1992 researcher John Davis completed a meta-analysis of all antidepressant data available at the time in unipolar depression studies and not only found that antidepressant continuation was more effective than placebo in reducing the likelihood of later depressions, but also calculated that the statistical likelihood that this finding was due to chance was minuscule, i.e., p<10-34. John Geddes and colleagues in a meta-analysis in 2003 indicated that there was an approximate 70% reduction in the risk of depressive recurrences with antidepressant continuation compared with discontinuation.
Treatment of a first or second episode of unipolar depression is recommended for six to nine months following achievement of remission. After a third episode, all treatment guidelines of which this editor is aware recommend long-term preventive treatment with antidepressants, particularly if episodes have been severe or close together temporally. This long-term antidepressant continuation for prophylaxis is much like long-term treatment of high blood pressure or high cholesterol recommended for those with or at high risk for cardiovascular disease.
There is some evidence that cognitive behavior therapy reduces the risk for depressive recurrence in those discontinuing antidepressant treatment, but it appears maximally beneficial to engage both psychotherapeutic and pharmacological treatment to prevent future episodes. Read more
Antidepressants Prevent Suicide in Patients with Unipolar Depression
Researcher A. Kahn reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in Boca Raton in 2011 that severely depressed and suicidal patients taking citalopram (Celexa) or a combination of citalopram and low dose lithium experienced improvements in depression and suicidal thoughts. This study was unusual because most clinical trials exclude actively suicidal patients. In the group of subjects receiving citalopram plus lithium (300 mg/day and achieving 0.5 mEq/l or higher), there were several indications of better anti-suicide effects than in those on citalopram alone. The authors concluded that with appropriate doses, antidepressants plus lithium may prospectively reduce suicidal thoughts, and that it is possible to conduct clinical trials in severely depressed and suicidal patients if adequate safety measures are included.
Surprisingly, improvement in suicidal ideation preceded improvement in depressed mood per se.
Editor’s note: The study reported here suggests that in those with high suicidal ideation scores at baseline, antidepressants with or without lithium may quickly bring about anti-suicidal effects on thoughts, desires, and behaviors. Whether these effects occur reliably in studies in other groups of patients and in younger individuals remains to be established.
These data are an interesting contrast to data on antidepressant use in those with low levels of suicidality at baseline. A number of studies have suggested that in children and adolescents who were exposed to an antidepressant, a small percentage experienced increases in suicidal ideation in the first two months of treatment compared to patients taking placebo. This led to a Federal Drug Administration (FDA) warning (directed at all patients taking antidepressants) that increases in suicidal ideation and action may occur upon starting antidepressants.
It is important to note that the warning does not refer to completed suicides; the data set that led to the FDA warning included no completed suicides. More than 70% of those with suicidal ideation do not make an attempt, and the vast majority of attempts do not result in a completed suicide.
Most of the studies that found the slight increase in suicidal ideation in some patients after beginning antidepressant treatment actively excluded acutely suicidal patients. Since the study of citalopram and lithium above used a population of severely depressed and suicidal patients and found that antidepressants improved suicidality, it appears important to consider a patient’s baseline state when considering psychiatric interventions. In another example, there is an interesting difference between the way depressed patients and non-depressed normal volunteers respond to one night’s sleep deprivation: depressed patients often show dramatic improvement, while normal volunteers tend to feel worse.
More Evidence that Antidepressants Prevent Suicide in Unipolar Depression
A new study by DeLeon published in the Journal of Clinical Psychiatry in 2011 found that during periods of life when unipolar patients were taking antidepressants (compared to times when they were not taking them) the patients experienced 20% fewer suicidal acts or completed suicides. Read more
Thyroid Augmentation May Improve Depression in Women with Treatment-Resistant Bipolar Depression
 We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
We have previously written about a study of supra-physiological doses of levothyroxine (a synthetic version of the hormone T4 sold under the brand name Synthroid) performed by Mike Bauer and colleagues in Dresden, Germany and at UCLA. Sixty-three patients were initially treated with an antidepressant and/or a mood stabilizer for one week during a single-blind phase. Then the six-week double-blind phase of the study began, in which patients were given either adjunctive T4 (in the form of levothyroxine ) or placebo, and this was followed by an additional six weeks of open treatment with T4. Patients were started at 100mcg and increased on a weekly basis to 200 and then 300mcg/day.
Overall, T4 had no statistically significant effect that differentiated it from placebo, but among women, there was a significantly greater degree of improvement in the Hamilton Rating Scale for Depression scores for those on T4 (-42.4%) than for those on placebo (-16.6%), p= .018.
Editor’s note: This study is the first randomized, placebo-controlled trial of supra-physiological doses of T4. A small series of reports in the literature from several different investigative groups had previously suggested efficacy of this compound in rapid cycling and treatment-resistant patients. Read more
Moclobemide May Help Depression and Post-Partum Blues
Monoamine oxidase inhibitors (MAO-Is) are a type of antidepressant that is often effective for people with anxious depression or comorbid panic attacks, especially when other antidepressants don’t work. This may be because MAO-Is work on all three neurotransmitter systems implicated in depression: dopamine, norepinephrine, and serotonin.

In a recent study presented at the 65th Annual Scientific Convention of the Society of Biological Psychiatry, Julia Sacher et al. found that six weeks of therapeutic doses of the MAO-I moclobemide (at doses of 300 mg twice a day) significantly decreased monoamine oxidase A, as measured by PET scans in brain regions implicated in mood disorders. In a comparison of moclobemide, placebo, and the herbal preparation St. John’s Wort, only moclobemide had a significant effect. Read more
rTMS for Adolescent Depression
In an abstract presented at the 65th Annual Scientific Convention of the Society of Biological Psychiatry, Christopher Wall reported that treatment with rTMS (10 Hz at 120% of motor threshold) was successful in the treatment of adolescent depression.
These data from an open (as opposed to blind) study deserve further and more systematic investigation. Alternatives to antidepressant drug treatment are desirable for adolescents with depression since increases in suicidal ideation are a potential side effect during the first two months after initiation of pharmacological antidepressant treatment in teens. (Suicidal ideation and actions among adolescents decrease with longer-term antidepressant treatment, especially when it is used in conjunction with cognitive/behavioral psychotherapy.) Children and adolescents treated with antidepressants may also be at higher risk for switching into mania than adults treated with antidepressants.
Editor’s Note: The rTMS parameters used in this study are the same as those used successfully in adults with depression in the two large positive multi-center sham-controlled studies (one by industry and one by the National Institute of Mental Health) mentioned in yesterday’s article.
Anti-Alzheimers’s Drug Memantine (Namenda) May Augment the Antidepressant Effects of Lamotrigine
 At the 65th Annual Scientific Convention of the Society of Biological Psychiatry in May, Amit Anand reported that the anti-Alzheimer’s drug memantine (20 mg/day) was superior to placebo in augmenting the acute antidepressant effects of lamotrigine. These data are of particular interest since one of the assumed mechanisms of action of lamotrigine is to decrease the release of glutamate.
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry in May, Amit Anand reported that the anti-Alzheimer’s drug memantine (20 mg/day) was superior to placebo in augmenting the acute antidepressant effects of lamotrigine. These data are of particular interest since one of the assumed mechanisms of action of lamotrigine is to decrease the release of glutamate.
Memantine is a drug approved for the treatment of Alzheimer’s disease and is a partial antagonist (blocker) of glutamate NMDA receptors. This suggests that the dual actions of inhibiting glutamate’s release pre-synaptically (with lamotrigine) and blocking glutamate receptor activity post-synaptically (with memantine) combine to produce a better effect than that of lamotrigine alone.
5 Myths About Unipolar Depression
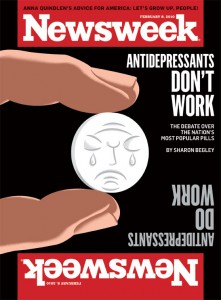 Early this year, news stories such as Newsweek’s “The Depressing News About Antidepressants” and “Antidepressant Drug Effects and Depression Severity” in the Journal of the American Medical Association (JAMA) created an inadequate picture of the seriousness of clinical depression, and the importance of preventing recurrent episodes with long-term antidepressant treatment. (For a rebuttal, see Psychiatric Times.)
Early this year, news stories such as Newsweek’s “The Depressing News About Antidepressants” and “Antidepressant Drug Effects and Depression Severity” in the Journal of the American Medical Association (JAMA) created an inadequate picture of the seriousness of clinical depression, and the importance of preventing recurrent episodes with long-term antidepressant treatment. (For a rebuttal, see Psychiatric Times.)
The consequences of this distorted depiction of depression and its treatment are potentially dire for individuals’ health. Some of the popular myths about depression deserve critical review so that patients can make more informed decisions about their own treatment.
Myth 1: Depression is all in your mind
Myth 2: Depression is over-treated
Myth 3: Antidepressant efficacy barely exceeds that of placebo
Myth 4: Antidepressants should be stopped as soon as possible
Myth 5: Depression is a minor medical problem
Myth 1: Depression is all in your mind
This might seem valid, since depression is classified as a mental illness. But depression is not abstract, imaginary, or lacking a solid physical foundation. There is now overwhelming evidence that depression coincides with disturbances in multiple brain and body systems.



