Preventing Illness in the Offspring of a Parent with Bipolar Disorder
A 2018 article by researcher Robert Freedman and colleagues in the American Journal of Psychiatry reported that prenatal nutritional supplements can reduce mental illness in at-risk offspring. The article made a good case for supplementation with folate, phosphatidylcholine, and vitamins A and D.
Here we describe some additional ways to minimize risk of mental illness in children who are at risk for bipolar disorder or other mental illnesses.
Some efforts at prevention can begin even before a child is conceived. Avoiding smoking or drinking alcohol and maintaining a nutritious diet to prevent inflammation and excessive weight gain before conception could reduce adverse epigenetic effects on the offspring. Epigenetics refers to environmental influences on gene transcription. The impact of life experiences such as a mother or father’s substance use is not registered in their child’s DNA sequence, but can influence the structure of the child’s DNA or its packaging.
Maternal good health and wellbeing during pregnancy has also been shown to improve neonatal health and functioning.
Once a child is born, they can be encouraged in healthy habits, including a nutritious diet, good sleeping habits, regular vigorous exercise, and mindfulness/meditation training (which pediatric psychiatrist James Hudziak has suggested should be universal).
For a child who is beginning to develop mood or behavioral symptoms, more intensive intervention may be prudent. Research supports the effectiveness of family interventions such as family-focused therapy (FFT) for youth with depression, cyclothymia, or bipolar disorder not otherwise specified (BP-NOS) and a family history of bipolar disorder. Researcher David J. Miklowitz described the effects of this intervention in a 2013 article in the Journal of the American Academy of Child and Adolescent Psychiatry.
Depression in children 3 to 6 years of age is as common as depression in older children (with rates around 1–2%), and robust improvements have been observed when families engage in parent child interaction therapy (PCIT) with a focus on emotional development. In PCIT, parents are coached while interacting with their children and encouraged to establish warm interactions while setting appropriate limits. In a study by Joan L. Luby and colleagues published in the American Journal of Psychiatry in 2018, using PCIT modified to include an emotional development component improved depression and associated symptoms in children aged 3 to 11, and it also improved mothers’ mood and behavior. Read more
Nimodipine Decreases Frontal and Parietal Cortical Activity During Working Memory in Healthy Subjects
At a recent scientific meeting, researcher Kristin Bigos and colleagues described the effects of nimodipine, a treatment for brain hemorrhage, on the brain during working memory tasks. Nimodipine is a dihydropyridine L-type calcium channel blocker. Calcium channel blockers prevent calcium from entering cells in the heart and blood vessel walls, and they are often used to treat high blood pressure.
Nimodipine acts on the CACNA1C calcium influx gene. Certain genetic variations in this gene (particularly the rs1006737 A allele) have been linked to vulnerability to bipolar disorder, schizophrenia, depression, and autism. Carriers of the risk allele also have higher CACNA1C mRNA expression in the dorsolateral prefrontal cortex and exhibit more activity in the frontal and parietal regions of the brain during working memory tasks, suggesting inefficient brain processing in these regions. Bigos and colleagues found that 60mg/day of nimodipine decreased frontal and parietal cortical activity by 39.1% and 42.8%, respectively, during a working memory task, suggesting that nimodipine improved the efficiency of memory processing. Nimodipine’s positive effects were greater in those participants who had the CACNA1C risk allele.
Editor’s Note: Using a placebo-controlled off-on-off-on study design (meaning patients took placebo for a period, then nimodipine, then placebo again and nimodipine again), this editor (Robert M. Post), Peggy J. Pazzaglia and colleagues found that nimodipine had positive effects in both mania and depression in patients with bipolar disorder (described in the 2008 book Treatment of Bipolar Disorder: A Casebook for Clinicians and Patients by Robert M. Post and Gabriele S. Leverich). In a large randomized study of patients with bipolar disorder presented by Haroon R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry, lithium was associated with about a 50% response rate while the combination of lithium and nimodipine was associated with a 73% response rate.
It remains to be seen whether people with bipolar disorder who have the CACNA1C risk gene would respond better to nimodipine than those without the risk gene, and whether it would improve working memory more in the subgroup with the risk gene.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
White Matter Abnormalities in Obesity
Researcher Ramiro Reckziegel and colleagues reported at a recent scientific meeting that white matter is abnormal in obese adults with bipolar disorder. In a 2018 article in the journal Schizophrenia Bulletin, Reckziegel reported that body mass index (BMI) was associated with reduced fractional anisotropy, a measure of brain fiber integrity, in the cingulate gyrus in patients with bipolar disorder. This finding implies that obesity may play a role in white matter microstructure damage in the limbic system.
White Matter Abnormalities Linked to Irritability in Both Bipolar Disorder and DMDD
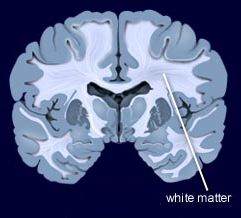 At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
Risk of Suicide in People with Bipolar Disorder: Lowest with Lithium, Highest with Antidepressants
Researcher Markku Lähteenvuo and colleagues reported in the journal JAMA Psychiatry in early 2018 that long-acting injectable antipsychotics and lithium were best at preventing re-hospitalization in 18,018 bipolar patients in Finland who received an average of more than 7 years of follow up. Lähteenvuo and colleagues have now gone on to analyze suicide data from the same cohort of patients with bipolar disorder, and report that those taking lithium had the lowest rate of suicide, while those taking valproate had the next lowest suicide rate. Those patients with bipolar disorder who were treated with antidepressants had the greatest suicide rate. The suicide rate was particularly high for those once-hospitalized patients taking the MAO inhibitor antidepressant meclobemide, which is not approved for use in the US. Increased rates of suicide were also seen with use of sedatives and benzodiazepines.
Editor’s Note: Evidence continues to mount that lithium should be the definitive first line therapy in bipolar disorder for a multitude of reasons (as this editor Robert M. Post reviewed in an open-access article in the journal Neuropsychopharmacology in 2017). Still, lithium is not often prescribed for people with bipolar disorder in the US, and this does not seem to be in these patients’ best interests.
Use of antidepressants in bipolar disorder has remained controversial, but it is common in clinical practice despite a lack of evidence that it is effective, and the presence of some evidence that it is actually harmful. Antidepressant use in a person with bipolar disorder may cause switching into mania, cycle acceleration, dysphoria induction, and even suicide.
Clinicians should take these data seriously and overcome the impulse (leftover from treating unipolar depression) to use unimodal antidepressants as first line or adjunctive therapy for bipolar depression. Antidepressants are only effective in the long term in about 15% of patients with bipolar depression, and now it appears antidepressant use also carries an additional risk of suicide.
American Academy of Pediatrics Recommends Parents Avoid Spanking and Verbal Abuse
The American Academy of Pediatrics (AAP) has issued a policy statement calling for an end to corporal punishment, including spanking. These forms of punishment are tied to negative outcomes in every developmental area.
Children spanked regularly at age 3 had increased aggression risk by age 5. They also had more negative behaviors and lower vocabulary scores at age 9. Abusive behavior raises stress hormones and is associated with mental health struggles.
Verbal abuse should also be avoided. Verbal abuse includes punishment that shames, humiliates, threatens, frightens, or ridicules a child. Use of time outs, removal of privileges, and other forms of quiet discipline are recommended alternatives.
Editor’s Note: In our research network, the Bipolar Collaborative Network, we found that verbal abuse by itself (without the physical or sexual abuse that often accompany it) is associated with an earlier age of onset of bipolar disorder and a more difficult course of illness.
Family focused therapy (FFT) and other forms of family therapy are highly recommended for children of a parent with bipolar illness. These children are at high risk for a variety of psychiatric diagnoses, and those already experiencing depression, cyclothymia (mood swings between high and low) or a diagnosis of bipolar disorder not otherwise specified (BP-NOS) are much improved with FFT compared to treatment as usual. FFT teaches family members to recognize symptoms of illness for what they are rather than interpreting them as deliberate hostility, increases family communication and problem solving, and leads to good long-term outcomes.
Recent Cannabis Use Linked to Greater Symptoms of Anxiety and Mood Disorders and Less Response to Treatment
 In a 2018 systematic literature review published in the Journal of Clinical Psychiatry, researcher George Mamman and colleagues reported that across 12 studies of people with anxiety and mood disorders, participants who had used cannabis in the previous six months had more symptoms than those who had used less cannabis or no cannabis during that period.
In a 2018 systematic literature review published in the Journal of Clinical Psychiatry, researcher George Mamman and colleagues reported that across 12 studies of people with anxiety and mood disorders, participants who had used cannabis in the previous six months had more symptoms than those who had used less cannabis or no cannabis during that period.
The 12 studies reviewed included a total of 11,959 participants. Four studies looked at post-traumatic stress disorder (PTSD), one at panic disorder, five at bipolar disorder, and 2 at depressive disorder. In addition to finding that recent cannabis use was associated with greater symptoms, the authors of the review also found that in 10 of the 12 studies, recent cannabis use was associated with less symptom improvement in response to treatment for bipolar disorder, depression, and PTSD; including both medication and psychotherapy.
In bipolar disorder, cannabis use was associated with greater symptom severity. Cannabis use for more than one year was linked to more recurrences of mania and shortened time to a recurrence. Compared to participants with no prior use of cannabis, those with a cannabis use disorder had more depressive symptoms, including sleep troubles and loss of interest in activities one had previously enjoyed.
In PTSD, any cannabis use at the beginning of the analysis period and sustained use of cannabis over time were both linked to greater symptom severity in the four months following the beginning of the analysis.
Mammen and colleagues cautioned that these results are limited based on the differences in measurements across the 12 studies, the inpatient populations under study, and the uncontrolled nature of the cannabis the participants accessed on their own time. However, the authors suggest that the findings may inform patients’ and doctors’ conversations about whether or not to use cannabis.
Early Intervention Works in Schizophrenia: Also Needed in Bipolar Disorder
For twenty years, evidence has shown that early intervention can ameliorate many of the adverse consequences of schizophrenia. In a 2018 article in the journal Annual Review of Clinical Psychiatry titled “Transforming the treatment of schizophrenia in the United States: The RAISE Initiative,” Lisa B. Dixon and colleagues described the importance of early intervention in schizophrenia. RAISE stands for Recovery After an Initial Schizophrenia Episode. Dixon and colleagues emphasize that shortening the time that a patient’s psychosis goes untreated, which averages 74 months, is critical to achieving good outcomes. In parallel to these consistent findings, researchers of bipolar disorder (including this editor Robert M. Post and colleagues) have found that an increased length of the interval before treatment is initiated in childhood-onset bipolar disorder is associated with a poor outcome in adulthood.
The RAISE program consists of four interventions: personalized psychopharmacology using a computerized decision support system, individual resilience therapy, family psychoeducation and therapy, and supportive employment and education. Compared with patients receiving standard treatments, patients who participated in the RAISE program showed greater improvements on almost all measures, including the Heinrichs-Carpenter Quality of Life Scale (main outcome), the Calgary Depression Scale for Schizophrenia, the Positive and Negative Syndrome Scale, treatment duration, and engagement in work and school. Moreover, the improvements were more substantial among patients with a shorter duration of untreated psychosis.
Editor’s Note: These findings are of great importance in their own right, but they also have great implications for treatment and research efforts in bipolar disorder. A 2013 randomized study by Lars Kessing and colleagues published in the British Journal of Psychiatry found that in bipolar patients hospitalized for a first or second episode of mania, two years of comprehensive treatment with psychotherapy, pharmacotherapy, and illness education that included mood monitoring and early symptom recognition was vastly superior to typical treatment, and this held true even six years later. In a 2014 article in the Journal of Clinical Psychiatry and a 2016 article in the journal Bipolar Disorders, researcher Jan Marie Kozicky and colleagues reported that in patients hospitalized with a first episode of mania, cognitive functioning and brain imaging abnormalities, respectively, returned to normal over the next year only if the patients experienced no further mood episodes. The message is clear: we must treat the first episode of mania comprehensively to avoid long-term deterioration, which occurs as a function of the number of episodes of mania or depression a patient experiences. However, this early multimodal approach is rarely taken in the US.
In schizophrenia, Dixon and colleagues noted that: “After the RAISE study reports were made available, Congress allocated additional funding to the community mental health …program, leading to growth in the number of…programs across the United States; they were expected to reach 48 states in 2018.”
The contrast between these efforts in schizophrenia and their virtual absence in bipolar disorder is incomprehensible and tragic. Studies in early schizophrenia have been funded for 25 years, while almost none have been funded in bipolar disorder, even in recent years. Community mental health programs for early schizophrenia will soon exist in 48 states; for patients with bipolar disorder there are no programs available in any state that I am aware of. The incidence of bipolar is about three times that of schizophrenia, and the long-term outcomes are often as devastating in bipolar disorder as in schizophrenia. There is a high incidence of drug abuse; social, educational and occupational deficits; and suicide in bipolar disorder. Early intervention with the many safe supplements, nutraceuticals, and well-tolerated drugs that are currently available to adult patients should be studied in young people with bipolar disorder, but such studies neither being funded nor conducted.
The reality is that childhood-onset bipolar disorder is poorly recognized and treated in the US, largely because of a paucity of treatment-related studies and knowledge about the best options for these young patients. If a reader of the BNN knows how to influence advocacy groups, leaders in the Substance Abuse Mental Health Services Administration (SAMHSA) and the National Institutes of Mental Health (NIMH), or influential politicians, it would be useful to take the initiative in bringing some of these deficits and disparities to their attention. Something must be done; ideas about how to do it are welcome. My own efforts to get funding for a childhood-onset bipolar research network in collaboration with such luminaries in the field as David Miklowitz (UCLA), Kiki D. Chang (Stanford University), Boris Birmaher (University of Pittsburg), Benjamin Goldstein (Stonybrook Research Institute), Eric Youngstrom (UNC, Chapel Hill), Soledad Romero (Hospital Clinic of Barcelona), and Josefina Castro Fornieles (University of Barcelona) have not been successful. We will keep trying, but the field needs to reach beyond the many investigators who are advocating for more treatment research to other people with more influence.
Antioxidant N-Acetylcysteine Improves Working Memory in Patients with Psychosis
 In a 2017 article in the journal Psychological Medicine, researcher Marta Rapado-Castro and colleagues reported that among 58 patients with bipolar disorder or schizophrenia and symptoms of psychosis, those who took two grams per day of the antioxidant n-acetylcysteine (NAC) showed improvements in working memory after six months compared to those who took placebo over the same study period.
In a 2017 article in the journal Psychological Medicine, researcher Marta Rapado-Castro and colleagues reported that among 58 patients with bipolar disorder or schizophrenia and symptoms of psychosis, those who took two grams per day of the antioxidant n-acetylcysteine (NAC) showed improvements in working memory after six months compared to those who took placebo over the same study period.
Antipsychotic medications can typically reduce psychotic symptoms such as delusions or hallucinations, but cognitive symptoms such as problems with learning, memory, or information processing may remain. NAC, which is sold over-the-counter as a nutritional supplement, seemed to improve these symptoms.
The researchers suggest that larger studies of NAC are needed, particularly to determine whether giving NAC to patients during their first episode of psychosis could prevent cognitive decline from occurring at all during the course of their illness.
NAC has been found to have a range of benefits, including reducing substance abuse and interfering with habit-based behaviors such as compulsive hair-pulling, obsessive-compulsive disorder, and gambling.
Researcher Michael Berk, a co-author of the study, reported in the journal Biological Psychiatry in 2008 that NAC could also improve depressive symptoms in bipolar disorder and negative symptoms in schizophrenia.
Editor’s Note: Since cognitive deficits are common in both schizophrenia and bipolar disorder, using NAC in addition to antipsychotic medications could be a useful tool to address these types of symptoms.