RTMS Improves Working Memory In Patients With Schizophrenia
 Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Editor’s Note: Since many patients with bipolar disorder also have deficits in prefrontal-based memory and performance even when euthymic, it will be important to see if rTMS would also be helpful in these patients. RTMS at 20 Hz increases neuronal activity as measured by PET scan of the prefrontal cortex and other regions of the brain, and this lasts for at least 48 hours after each treatment.
Since many patients with schizophrenia and bipolar disorder show deficits in prefrontal activity at baseline, the normalization of these alterations could relate to the memory improvement. This proposition could be tested relatively easily.
Oxytocin Improves Social Cognition In Schizophrenia
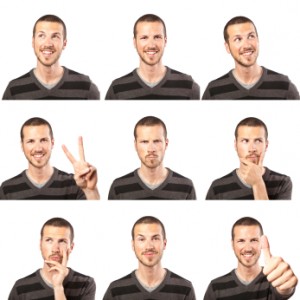 Researcher Josh Woolley and colleagues at the University of California, San Francisco have found that intranasal oxytocin (at doses of 40 IU) improved social cognition in patients with schizophrenia when compared with placebo. Oxytocin is a hormone that facilitates social bonding. Social cognition refers to the way we understand what emotions other people are communicating through facial expression, voice, etc.
Researcher Josh Woolley and colleagues at the University of California, San Francisco have found that intranasal oxytocin (at doses of 40 IU) improved social cognition in patients with schizophrenia when compared with placebo. Oxytocin is a hormone that facilitates social bonding. Social cognition refers to the way we understand what emotions other people are communicating through facial expression, voice, etc.
Interestingly, less complicated aspects of social cognition like recognizing affect and distinguishing between sincerity and sarcasm were not affected by the oxytocin treatment. However, more complex types of social inference (such as decoding whether an actor intended sarcasm versus telling a white lie) were substantially improved. These tasks evaluate “theory of mind”—the ability to attribute mental states to oneself and others, and to recognize that another person’s mental state may be different from one’s own. These abilities are sometimes lacking in those with schizophrenia and other disorders, such as autism. Given that these abilities have been related to real world social functioning, Woolley and colleagues suggest that oxytocin could, for example, help these individuals to make more friends.
Adjunctive Topiramate Is Effective In Schizophrenia
 Many patients with schizophrenia do not reach full remission on antipsychotic drugs alone. The anticonvulsant drug topiramate (Topamax) has shown some promise as an adjunctive treatment for schizophrenia. To clarify the results of studies of topiramate, researcher Christoph Correll and colleagues performed a meta-analysis of nine randomized, placebo-controlled clinical trials of the drug. They found that when topiramate was added to antipsychotic treatment, it improved both positive and negative symptoms of schizophrenia, and it also led to reduced weight.
Many patients with schizophrenia do not reach full remission on antipsychotic drugs alone. The anticonvulsant drug topiramate (Topamax) has shown some promise as an adjunctive treatment for schizophrenia. To clarify the results of studies of topiramate, researcher Christoph Correll and colleagues performed a meta-analysis of nine randomized, placebo-controlled clinical trials of the drug. They found that when topiramate was added to antipsychotic treatment, it improved both positive and negative symptoms of schizophrenia, and it also led to reduced weight.
Editor’s Note: Topiramate might also be useful for patients with schizophrenia who have the common comorbidities of alcohol and cocaine abuse, since in other studies of patients with these primary disorders, topiramate was helpful.
Aspirin added to Regular Treatment Reduces Symptoms of Schizophrenia
Most drugs used to treat schizophrenia target dopamine and serotonin receptors in the brain. While these are effective in many patients, relapse is common and side effects can be severe. Researchers are looking for ways to target other mechanisms that cause schizophrenia, and inflammation seems to be one of these. There is evidence that a treatment as simple as aspirin, when added to regular treatment with antipsychotics, can improve schizophrenia by targeting inflammation.
In a 2010 study by Laan et al. published in the Journal of Clinical Psychiatry, patients with moderate or severe schizophrenia were given either placebo or aspirin (acetylsalicylic acid, 1000mg) in addition to their regular treatments every day for three months. The patients who received aspirin showed a significant reduction in the positive symptoms of schizophrenia, and to a lesser extent the negative symptoms, compared to those who received placebo. Cognitive function was not improved. The effect size (Cohen d) for the total scale score was 0.5, which is considered a “medium” effect and one that is clinically relevant.
The reductions in symptoms were greater in those patients who had more altered immune function.
Choline Treatment For Pregnant Mothers And Newborns Improves Babies’ Cognition and Normalizes a Risk Factor for Schizophrenia
Deficiencies in GABA inhibition have been linked to the risk of schizophrenia (and perhaps bipolar disorder). GABA receptors are initially excitatory but switch to being inhibitory early in life. Choline derived from phosphatidylcholine or from eggs and meat in the diet is important in increasing GABA receptor development and maturity.
Ross et al. reported this year in the American Journal of Psychiatry that in a placebo-controlled study in which mothers took phosphatidylcholine in the last 2 trimesters of pregnancy (at doses of 3,600mg in the morning plus 2,700mg in the evening) and infants took 100mg/day for 12 weeks, the infants who received choline showed better neuronal inhibition than infants who did not receive choline on a P50 test of auditory evoked potential, in which the brain’s response to a series of beeps is recorded. An overactive P50 response is a sign of deficiencies in GABA inhibition.
In infants with a common gene variant in the alpha 7 nicotinic receptor that makes it function less well (which also may be a risk factor for the development of schizophrenia), the choline regimen normalized the P50 test, while placebo had no effect. However, in a recent study by Cabranes et al. published in Psychiatry Research, there was no association of the alpha 7 gene variant and schizophrenia or bipolar disorder, although patients with bipolar disorder and patients with schizophrenia did perform differently on the P50 evoked potential test than controls did.
Editor’s Note: In an editorial by Judy Rapoport that accompanied the Ross et al. study, the difficulty of using the findings in clinical practice are discussed. Meck et al. showed in 1999 that choline supplementation enhanced spatial memory, and in several cases nutritional supplements can have beneficial effects on the brain. Rapoport notes the success of perinatal folate in preventing neural tube defects and the likelihood that Vitamin D supplementation can prevent some cases of schizophrenia.
However, extrapolating the choline findings of Ross et al. to clinical practice, especially given the lack of association of the alpha 7 gene variation to psychiatric illness in the study by Cabranes et al., might be premature. Instead, Rapoport recommends a good diet and prevention of infection as first steps for treatment. Choline supplementation would be roughly equivalent to three eggs a day.
Creative People More Likely to Have Mental Illness
According to a large family study of people with severe mental disorders that was published by Kyaga et al. in the British Journal of Psychiatry last year, people with bipolar disorder and siblings of people with schizophrenia or bipolar disorder were much more likely to be working in creative professions than people without severe mental illness.
Kyaga talked to Medscape Medical News about the study:
“I think the study stresses the importance of treating all patients individually, and with the aim of finding the optimal treatment with regards to effectiveness, while minimizing the adverse effects that medication can have on positive aspects of psychiatric disorders,” Dr. Kyaga said.
“We often encounter the suggestion that lithium reduces creativity in patients with bipolar disorder and that adherence therefore is difficult. Now we can say that it is true that bipolar disorder is in fact associated with increased creativity, but we also know from previous research that terminating treatment with lithium in bipolar disorder will, in the long run, disrupt creative behavior,” he continued.
“We therefore need to pay close attention to what patients tell us while being treated, so that we can find a regimen that will work for them to prevent the disastrous consequences of severe psychiatric disorder, while providing them opportunities to uphold their creative behaviors in the long run,” Dr. Kyaga said.
Aspirin May Help Reduce Schizophrenia Symptoms
An article by Laan et al. published in the Journal of Clinical Psychiatry in 2010 suggested that aspirin may reduce symptoms of schizophrenia spetrum disorders in patients being treated with antipsychotics.
Aspirin is an anti-inflammatory drug. We’ve written before about the possible use of aspirin in bipolar disorder and about the role of inflammation in mental illness.
New Atypical Antipsychotic Lurasidone Has a Good Metabolic Profile
 Andre Pikalov and colleagues from Sunovion Pharmaceuticals Inc. reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 on the weight and metabolic effects seen in short- and long-term trials of the atypical antipsychotic lurasidone (Latuda) in schizophrenia. The studies compared lurasidone to olanzapine (Zyprexa, at 15mg), haloperidol (Haldol, at 10mg), and placebo. Doses of lurasidone ranged from 20-120mg administered once daily. Short-term treatment for six weeks was associated with changes in weight and metabolic indices similar to those of placebo, while participants taking olanzapine gained substantial amounts of weight and had increases in triglycerides and cholesterol. Changes in glucose and hemoglobin A1C were similar on lurasidone, haloperidol, and placebo, but higher on olanzapine. In the long-term sample, mean weight gain on lurasidone at 12 months was 0.71 kg and metabolic parameters remained relatively unchanged.
Andre Pikalov and colleagues from Sunovion Pharmaceuticals Inc. reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 on the weight and metabolic effects seen in short- and long-term trials of the atypical antipsychotic lurasidone (Latuda) in schizophrenia. The studies compared lurasidone to olanzapine (Zyprexa, at 15mg), haloperidol (Haldol, at 10mg), and placebo. Doses of lurasidone ranged from 20-120mg administered once daily. Short-term treatment for six weeks was associated with changes in weight and metabolic indices similar to those of placebo, while participants taking olanzapine gained substantial amounts of weight and had increases in triglycerides and cholesterol. Changes in glucose and hemoglobin A1C were similar on lurasidone, haloperidol, and placebo, but higher on olanzapine. In the long-term sample, mean weight gain on lurasidone at 12 months was 0.71 kg and metabolic parameters remained relatively unchanged.
Editor’s note: Multiple posters at the meeting composed a substantial body of evidence concerning acute and long-term studies of lurasidone, which shows that the drug has a weight and metabolic profile relatively similar to placebo and more favorable than that of olanzapine.
Although lurasidone has not been studied acutely or in the long term in patients with bipolar disorder, the safety profile of this drug in schizophrenia indicates that it may eventually be useful for acute and long-term treatment strategies in bipolar disorder. All typical and atypical antipsychotic drugs that have been approved for treatment of schizophrenia have subsequently been shown to have efficacy in acute mania, and given lurasidone’s similar actions in blocking dopamine receptors, there is little reason to expect that this drug will be any different. The results of actual studies of this drug in mania and depression are eagerly awaited.
The Evolving Omega-3 Fatty Acid Story: The Icing on the Cake (And Why It Shouldn’t Be Eaten)
 Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
In a recent review of the literature, John Davis and Joe Hiblen found that diets that include high levels of omega-3 fatty acids are associated with decreased incidence of depression, suicide, and cardiovascular disease. The researchers performed a meta-analysis of all the prospective depression treatment studies of omega-3 fatty acids compared to placebo. They found that EPA had antidepressant effects in humans, with moderate effect size and a high degree of statistical significance. DHA, however, did not appear to have an antidepressant effect, and pure DHA was even associated with some worsening of depression.
Editor’s note: This meta-analysis helps clarify some of the ambiguities in the literature about the antidepressant efficacy of the omega-3 fatty acids, clarifying that EPA alone is an effective antidepressant. The one study that did not find antidepressant effects with EPA was carried out by the Bipolar Collaborative Network, in which I am an investigator. Our study, published in an article by Keck et al., showed that 6g of EPA was not significantly more effective than placebo in bipolar depression or in rapid cyclers. However, there is some indication that 6g may be too high a dose of EPA, and most of the recommendations now suggest using 1-2g of either EPA or an EPA/DHA combination. Read more
New Atypical Antipsychotic Lurasidone Appears To Improve Schizophrenia Without Weight-Gain Side Effects
 A study by a research group that included Antony Loebel of pharmaceutical company Sunovion; Steven Potkin of the University of California, Irvine; and Herbert Meltzer from Vanderbilt University summarizes data on a new atypical antipsychotic FDA-approved for treatment of schizophrenia. This agent, lurasidone (Latuda), was studied in a double-blind, placebo-controlled six-week trial in patients with schizophrenia.
A study by a research group that included Antony Loebel of pharmaceutical company Sunovion; Steven Potkin of the University of California, Irvine; and Herbert Meltzer from Vanderbilt University summarizes data on a new atypical antipsychotic FDA-approved for treatment of schizophrenia. This agent, lurasidone (Latuda), was studied in a double-blind, placebo-controlled six-week trial in patients with schizophrenia.
The drug is a new psychotropic agent that has a high affinity for dopamine D2 receptors and serotonin 5HT2A, 5HT1A, and 5HT7 receptors. (New data suggest that antagonistic effects on 5HT7 receptors may be related to antidepressant efficacy.)
In the study, patients were randomized to receive lurasidone at 80mg/day, lurasidone at 160mg/day, quetiapine XR at 600mg/day, or placebo. Evening dosing was used. Both dose levels of lurasidone resulted in significant degrees of improvement compared with quetiapine XR and placebo.
The side effects profile for lurasidone was also promising; patients were no more likely to gain weight on lurasidone than on placebo, while there was a mean 2kg weight increase on quetiapine XR. In addition, total cholesterol and triglycerides on both doses of lurasidone were similar to that on placebo, in contrast to small but significant increases on quetiapine XR.
There were significant increases in levels of prolactin (a hormone related to lactation, sex function, and bone demineralization) on lurasidone at both 80mg (+ 0.8mg/dl) and 160mg (+ 3mg/dl), while small decreases in prolactin were observed on quetiapine XR (-0.3 mg/dl) and on placebo (-0.8 mg/dl).
The data suggest that lurasidone is effective in the treatment of patients with acute exacerbation of schizophrenia, with significant effects occurring as early as day 4. This study had a low rate of adverse events. Read more