Transcranial Near-Infrared Light May Treat Brain Injury and Neurodegeneration
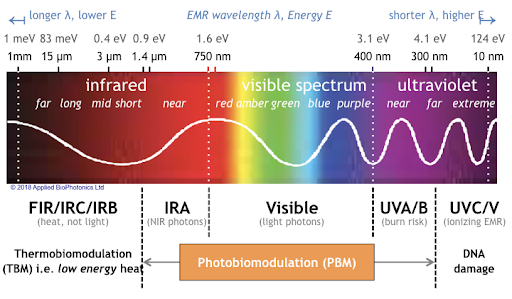
At the 2021 meeting of the Society of Biological Psychiatry, there was a symposium on treatment with near-infrared light chaired by researchers Paolo Cassano and Dan Iosifescu. The treatment is known as transcranial photobiomodulation (PBM) with near-infrared light. A device worn on the head delivers infrared light that penetrates the cerebral cortex and can modulate cortical excitability. It has a variety of effects including promoting neuroplasticity, improving oxygenation, and decreasing inflammation and oxidative stress.
A number of studies exploring the possibility that PBM could be used as a clinical treatment for conditions such as depression, brain injury, or dementia were presented at the symposium.
Researcher Lorelei Tucker discussed promising findings from an animal model in which rats with stroke or brain injuries showed improvement after being treated with PBM.
Cassano discussed studies aimed at refining which brain areas should be targeted with PBM and how much light should be delivered in order to improve depression. In double-blind, sham-controlled studies in people with major depression, targeting the dorsolateral prefrontal cortex with PBM improved their symptoms.
Researcher Benjamin Vakoc discussed a study of low-level light therapy (LLLT) using near-infrared light compared to a sham procedure in 68 people with moderate traumatic brain injury. The researchers used magnetic resonance imaging (MRI) to assess changes in white matter in the brain over time in people recovering from an acute brain injury. Patterns of changes in white matter were different for those who received LLLT compared to those who received the sham procedure.
Researcher Linda Chao described a very small study to determine whether PBM could improve symptoms of dementia. Four patients received typical dementia care while four others underwent home treatments with the commercially available Vielight Neuro Gamma device, which delivers PBM via both the scalp and an insert in the nose. After 12 weeks, the PBM group showed improvements in cognition and brain connectivity.

Editor’s Note: We will be watching the literature to follow advances in this promising novel method of neuromodulation.
Left Prefrontal Strokes Linked to Depression

In a 2021 article in the journal Stroke, researcher Julian Klingbeil and colleagues reported that left, but not right, ventrolateral prefrontal stroke lesions were associated with increased risk of depression at six months post-stroke.
The study included 270 participants who had their first-ever stroke. Six months following their strokes, 19.6% of the participants had depression. Those who scored higher on a scale of depression and anxiety symptoms in the first month after their stroke were more likely to have depression six months after the stroke.
The researchers identified a cluster of locations for stroke lesions, mostly within the left ventrolateral prefrontal cortex, that they linked to depression symptoms six months post-stroke. Klingbeil and colleagues hope that recognizing lesions in this region as risk factors for depression will help with early diagnosis of depression among people who recently had a stroke.
Editor’s Note: Antidepressants have been shown to improve post-stroke recovery of neurological functional (and depression) that is caused by the cutoff of blood supply during a stroke (ischemia). Patients and their family members should talk with their neurologist about treatment of ischemic strokes with antidepressants, especially when the lesions occur on the left side of the brain.
Increased Oxygen Improves Depression

At a recent scientific meeting, researcher R. Haim Belmaker reported that giving mildly to moderately depressed adults a nasal tube that delivers extra oxygen overnight for four weeks produced dramatic antidepressant effects. A total of 55 participants aged 18–65 years old were randomized to receive either normal room air (made up of about 21% oxygen), or hyperoxia (air containing about 35% oxygen). There was greater improvement on several different depression rating scales, including the Hamilton Depression Rating Scale, the Clinical Global Impression Scale, and the Sheehan Disability Scale, among those who received hyperoxia than among those who received normal air.
According to Belmaker, 69% of the patients who were treated with oxygen-enriched air improved on the CGI scale, compared to only 23% patients who were treated with room air. Limitations of the study were its small sample size and the lack of a clear biological mechanism for the effects of increased oxygen.
Childhood Physical Abuse Predicts Response to IV Ketamine

At a recent scientific meeting, researcher Alan Swann reported the results of a study of intravenous ketamine in people with treatment-resistant depression. The 385 participants, who received four infusions of IV ketamine at a dosage of 0.5 mg/kg, could be grouped into three based on their type of response to the treatment.
One group had moderate depression at baseline and showed little change. A second group with severe baseline depression also showed minimal improvement. A third group who also had severe baseline depression had a rapid and robust antidepressant response to the treatment. This group had high scores relating to physical abuse on the Childhood Trauma Questionnaire (CTQ), but did not differ on other clinical variables. Swann and colleagues concluded, “Our outcomes show that IV ketamine should be considered as a primary treatment option for adults presenting with severe, treatment resistant depression and a self-reported history of childhood physical abuse. IV ketamine may not be as effective for moderately depressed individuals irrespective of childhood maltreatment.”
Early Precursors of Mood Disorders in Young Children of Parents with Bipolar or Unipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Caroline Vandeleur presented findings from a 13-year study of children in Switzerland who have a parent with bipolar disorder or major depressive disorder. In contrast to findings from the US presented by Danella Hafeman, Vandeleur and colleagues found no evidence of psychopathology in 4 year-olds. They did find that in 7-year-olds, children of a parent with major depressive disorder were four times more likely to have a separation anxiety disorder. In an overall sample of 449 children with a mean age of 10 who were followed up for 13 years, major depression tended to be preceded by anxiety disorders. Participants who went on to be diagnosed with bipolar disorder had earlier symptoms of depression, subthreshold hypomania, conduct disorders, and drug abuse. These were especially common in those who had a parent with bipolar disorder.
Editor’s Note: These data indirectly confirm other observations in which children at high risk for mood disorders in the US showed earlier signs of psychopathology than those in other countries including the Netherlands and Canada.
AiTBS Superior to ECT in Small Study

Researchers Erica Jensen and Nolan Williams reported in abstracts of a paper that they were to present at the 2020 meeting of the Society of Biological Psychiatry in May that daily sessions of accelerated intermittent theta burst transcranial stimulation (aiTBS) over five or more days produced better results in 15 patients hospitalized for depression and suicidality than in matched patients who received electro-convulsive therapy.
AiTBS is a form of repeated transcranial magnetic stimulation (rTMS), in which a magnetic coil is applied to a patient’s scalp, producing electrical changes in the brain.
The aiTBS treatment was delivered to the left dorsolateral prefrontal cortex. It consisted of 1800 pulses per session, at 80% of a patient’s resting motor threshold with a 50-minute inter-session interval.
The patients in the study were matched (for age, gender, and treatment resistance) to patients who were hospitalized and given ECT. Among patients who received aiTBS and were discharged after an average of 8.4 days, there was an 86% response rate and a 73% remission rate. Among the patients who received ECT, who were discharged after an average of 22.3 days, there was a 53% response rate and a 40% remission rate. With further ECT, response and remission rates increased to 73% and 67%. Time to remission was 3.5 days with aiTBS and 31.3 days for ECT. The investigators concluded conservatively, “Our results suggest that aiTBS could have comparable efficacy to ECT, with potentially faster resolution of acute severe depression.”
Editor’s Note: ECT has been the gold standard treatment for severe depression and suicidality and now we may have a platinum comparator. If these findings are replicated, they could represent a paradigm shift in the treatment of severe depression. Hopefully, this novel form of rTMS will be fast-tracked for approval by the Food and Drug Administration (FDA).
Cannabis Use in Adolescence Linked to Depression and Suicidality in Young Adulthood

In a meta-analysis published in the journal JAMA Psychiatry in 2019, researcher Gabriella Gobbi and colleagues analyzed findings from 11 studies including a total of 23,317 participants and found that cannabis use in adolescence (before age 18) was associated with a significantly increased risk of depression, suicidality, and suicide attempts in young adulthood (between 18 and 32 years of age).
The researchers did not find a link between cannabis use and anxiety.
Editor’s Note: Cannabis use is not as harmless as many teens may believe.
Links Between Mixed Depression, Insulin Resistance, Inflammation, and Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre discussed links between obesity, diabetes, and cardiovascular problems; increased inflammation; and decreased functioning of the neural networks involved in cognition.
He and his colleagues analyzed 121 studies that included empirical research and meta-analyses. McIntyre and colleagues found that patients with higher levels of inflammatory markers have more insulin resistance and cognitive dysfunction. A meta-analysis revealed that the inflammatory markers IL-6, TNF alpha, and CRP were significantly elevated in people with bipolar disorder compared to normal controls, while IL-1B was not.
People with depression who had a few manic traits (mixed depression) were particularly likely to have insulin resistance and elevated levels of pro-inflammatory markers.
People with mixed depression have increases in inflammation and increased incidence of cardiovascular disorder. People experiencing a first episode of mixed depression who are overweight show increased signs of brain aging.
In studies McIntyre and colleagues analyzed, diabetes or pre-diabetes occurred in 50% of depressed patients, and these patients had the greatest amount of cognitive dysfunction.
Treatment
McIntyre noted that taking the antipsychotic drug lurasidone for bipolar depression worked best in both adults and children who had elevated levels of CRP at baseline. The fast-acting antidepressant ketamine also works well in those who show baseline inflammation .
The anti-diabetes drug liraglutide (Victoza, Saxenda) improves mixed depression symptoms and cognition in obesity, diabetes, and mixed depression. Liraglutide belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists or incretin mimetics. They work by increasing insulin release from the pancreas and decreasing excessive glucagon release.
McIntyre now routinely uses liraglutide for cognitive deficits in patients with obesity or diabetes, including patients with mixed depression. It is injected under the skin at 0.6 mg daily, then the dosage is increased to 1.2 mg and then 1.8 mg. Victoza reduces major cardiovascular events in those with type 2 diabetes. The higher-dose Saxenda (3mg) can be used for weight control.
Another anti-diabetes drug, pioglitazine, has also been reported to be helpful in bipolar depression.
McIntyre found that the antibody infliximab, which can be used as an intravenous treatment for chronic inflammation and works by blocking the effects of TNF-alpha, did not improve depression, but did improve cognition.
McIntyre also supports the use of acetyl-L-carnitine, a potential adjunctive treatment that can reverse the insulin resistance that often occurs with obesity and thus could theoretically improve cognition.
McIntyre described preliminary literature suggesting the effectiveness of drugs such as statins, calcium channel blockers, and biguanides such as the diabetes treatment metformin in reducing inflammation.
Bariatric surgery to reduce the size of the stomach was another option discussed by McIntyre. He said the intervention is safe for patients with bipolar disorder and can help them recover cognitive function.
McIntyre noted that offspring of a mother with obesity have decreased response to sensory cues, reward preference, cognitive control, and motor control. Obesity and the inflammation that goes along with it apparently affect offspring via epigenetic mechanisms, meaning obesity may change the structure of inherited DNA (without changing its sequence).
Meta-Analysis Finds Omega-3 Fatty Acids Do Not Reduce Cardiovascular Disease Risk
 In a 2018 meta-analysis published in the journal JAMA Cardiology, researcher Theingi Aung and colleagues found that across 10 studies including a total of 77,197 participants, omega-3 fatty acid supplementation did not reduce risk of coronary heart disease in people at high risk. This newer finding conflicts with a 2017 advisory from the American Heart Association that suggested omega-3 fatty acid supplementation might prevent cardiovascular disease.
In a 2018 meta-analysis published in the journal JAMA Cardiology, researcher Theingi Aung and colleagues found that across 10 studies including a total of 77,197 participants, omega-3 fatty acid supplementation did not reduce risk of coronary heart disease in people at high risk. This newer finding conflicts with a 2017 advisory from the American Heart Association that suggested omega-3 fatty acid supplementation might prevent cardiovascular disease.
When it comes to mood disorders, it has been similarly difficult to pin down whether omega-3 fatty acids are helpful. Data on omega-3 fatty acid supplements for the prevention of depression have been ambiguous, with small numbers of studies and variations in study design that make it difficult to draw strong conclusions about whether these supplements can improve or prevent depression.
A 2016 systematic review by Paola Bozzatello and colleagues in the Journal of Clinical Psychiatry found only seven studies of omega-3 fatty acid supplementation in bipolar disorder. The studies had small sample sizes and widely varying dosage parameters, so the evidence that can be drawn from them is not strong, but the review did find a modest benefit on bipolar depression (but not mania) when omega-3 fatty acids were added to a treatment regimen, compared to treatment as usual.
The same review found that studies of omega-3 fatty acid supplementation in unipolar depression also varied widely, and thus it was difficult to draw inferences from them. Some meta-analyses found no benefit to omega-3 fatty acid supplementation, while others suggested that omega-3s could improve depression. The review found that the type of omega-3 fatty acids used might matter. Supplementation with EPA seemed to improve depression more than supplementation with DHA. The review also cited a 2014 comprehensive meta-analysis by Giuseppe Grosso and colleagues in the journal PLoS One that analyzed the findings from 19 studies in people with depression or depressive symptoms. Grosso and colleagues found that people with more severe depression seemed to benefit more from omega-3s.
Inflammation Associated With Duration of Untreated Unipolar Depression
Researcher Sophia Attwells and colleagues reported at a 2018 scientific meeting that the longer the time that a patient went without treatment for depression, the more inflammation they exhibited on positron emission tomography (PET) scans. Attwells and colleagues used the PET scans to assess the total distribution volume of TSPO, which is a marker of brain microglial activation, a form of inflammation.
Strikingly, in participants who had untreated major depressive disorder for 10 years or longer, TSPO distribution volume was 29–33% greater in the prefrontal cortex, anterior cingulate cortex, and insula than in participants who were untreated for 9 years or less. TSPO distribution volume was 31–39% greater in these three important regions of gray matter in participants with long durations of untreated major depressive disorder than in healthy control participants.
Editor’s Note: In schizophrenia, the duration of untreated interval (DUI) is associated with a poor prognosis, but not with inflammation. Researcher Yvette Sheline has also reported that less time on antidepressants compared to more time treated with them was associated with greater hippocampal volume loss with aging in patients with major depression.
Given Attwells and colleagues’ remarkable finding about the adverse effects of the DUI in depression, including inflammation and brain volume loss, and other findings that associate more episodes with poorer functioning, cognition, and treatment responsiveness, physicians and patients should think hard about committing to long-term antidepressant treatment to prevent episodes, beginning early in the course of illness.
This editor (Robert M. Post) would propose that if a second depressive episode occurs after a first depression that responded well to treatment, this would be an appropriate time to start antidepressant prophylaxis. Most guidelines suggest that prophylaxis be started after a third episode, but these recommendations generally do not account for newer data on the pernicious effects of experiencing repeated depressive episodes. In addition to causing dysfunction and disability, going through four depressive episodes doubles the risk of dementia in old age, and this risk increases further with each successive episode, according to researcher Lars Kessing.
Having too many depressions is bad for the brain. In Kessing’s studies, two episodes of unipolar or bipolar depression did not increase the risk of dementia compared to the general population, while four depressions did. One could compare the effects of repeated depressions on the brain to the effects of heart attacks on the heart muscle. A heart might still function well after one or even two heart attacks, but the chances of significant loss of function and the risk of congestive heart failure increase as a function of the number of heart attacks. After even one heart attack, most patients change their lifestyle and/or go on prophylactic medications to reduce risk factors such as elevated blood pressure, cholesterol, triglycerides, weight, blood sugar, and smoking. The benefits of reducing heart attacks are a no brainer. Trying to prevent recurrent depression with pharmacotherapy and adjunctive psychotherapy after a second depressive episode should be a no brainer too.
In addition, if antidepressants are not effective enough in preventing depressions, lithium is an option, even in unipolar depression, for preventing both episodes and suicide. The evidence of efficacy in both instances is very strong according to an article by Mohammed T. Abou-Saleh in the International Journal of Bipolar Disorders in 2017. The renowned psychiatrist Jules Angst’s recommendation as to when to start lithium treatment was that if a patient had had one episode or more in the previous five years in addition to the present episode, then they were likely to have two further episodes in the following five years, and lithium prophylaxis would be recommended.



