Cannabidiol (CBD) does not make cannabis safer
Amir Englund et al reported in Neuropsychopharmacology in A randomised, double-blind, cross-over trial of cannabis with four different CBD:THC ratios that CBD did not protect against the adverse effect of THC. These included impaired delayed verbal recall ( p?=?0.001) and induced positive psychotic symptoms on the PANSS ( p?=?2.41?×?10–5).
Editors Note: Not only does marijuana impair memory, it is a risk factor the onset of bipolar disorder and schizophrenia. When pot is used by a person with a unipolar or bipolar mood disorder, there are increases in depression and anxiety and an overall less favorable course of illness. If a person with a mood disorder uses heavy amounts of marijuana, they could consider buying N-acetylcysteine (NAC) 500mg and increasing the dose to 1,000mg twice a day within a week as this has been shown to decrease drug use compared to placebo in adolescents and young adults using and abusing pot. Most people who sell pot, are not well-informed about its dangers and just want to make money.
Cannabidiol Reduces the Anxiety Induced by Simulated Public Speaking in Treatment-Naïve Social Phobia Patients
M M Bergamaschi, et al reported in Neuropsychopharmacology volume 36, pages 1219–1226 (2011) that the one of the ingredient in cannabis, the diol or cannabidiol (CBD), containing none of the usual THC which make up the vast majority of plant-based marijuana, reduces the anxiety Induced by simulated public speaking in treatment-naïve social phobia patients. They used “CBD (600?mg) in powder, ?99.9% pure (kindly supplied by STI-Pharm, Brentwood, UK and THC-Pharm, Frankfurt, Germany),… dissolved in corn oil.” This CBD has shown efficacy in other anxiety disorders and is FDA approved for one form of seizure disorder. This pure form of CBD is very expensive and usual preparations of available cannabis contain mostly THC and only minute amounts of CBD. Thus, the generalizability of these results to people using the widely available preparations of cannabis is extremely unlikely.
In Animal Model, Long-Term THC Exposure Interferes with Cortical Control of the Nucleus Accumbens

In an article in the journal Biological Psychiatry, researchers Eun-Kyung Hwang and Carl R. Lupica reported that in rats, long-term use of THC (tetrahydrocannabinol) weakens input from the cortex to the reward area of the brain, the nucleus accumbens (NAc). Long-term THC use also strengthens connections to the NAc from emotional control (limbic) regions, such as the basolateral amygdala and ventral hippocampus. Hwang and Lupica reason that this shift from cortical control of the NAc to limbic control likely contributes to the cognitive and psychiatric symptoms associated with cannabis use.
Editor’s Note: Street marijuana largely contains THC rather than CBD, the beneficial, anxiety-reducing component of cannabis. Cannabis products are being decriminalized, but it is important to remember that those with THC are linked to cannabis use disorder and increased susceptibility to psychiatric illness. Patients with bipolar disorder who use marijuana also have a more adverse course of illness than those who do not use it.
One Hit of THC Tied to Psychotic Symptoms in Adults with No History of Mental Illness

In a meta-analysis published in the journal Lancet Psychiatry, researcher Guy Hindley and colleagues reported that in otherwise healthy adults, a single dose of THC (equivalent to smoking one joint) produced transient psychotic symptoms.
The meta-analysis included 9 studies with a total of 196 participants. The researchers included studies in which participants took tetrahydrocannabinol (THC, the psychoactive component in marijuana) or placebo, and psychotic symptoms were measured.
The researchers also sought out studies in which cannabidiol or CBD was given in combination with THC, but there were not enough of these to derive significant results. CBD does not produce schizophrenia-like symptoms on its own, and some think it may have anti-psychotic effects, but findings on this topic have been mixed.
Taking THC had a large effect size on total psychotic symptoms and negative symptom severity (such as emotional flatness or avolition). It also had an effect on positive symptom severity (for example, hallucinations or delusions). The effects were larger with intravenous administration than with inhaled administration, and tobacco smokers had less severe positive symptoms.
Of four studies that included CBD, only one found that CBD reduced THC-induced psychotic symptoms.
Editor’s Note: Longer-term use of marijuana in adolescents and young adults doubles the risk of psychosis, and other data suggest that chronic use of marijuana at high doses can be associated with new onset of a diagnosis of bipolar disorder or schizophrenia. As cannabis products are being decriminalized around the US, it is worth noting some of the risks of marijuana use, particularly marijuana with a high level of THC.
How the Chemicals in Marijuana Work in the Brain
Raphael Mechoulam, who first synthesized THC, the main ingredient in marijuana, gave the history of marijuana and its receptors in the central nervous system in a plenary talk at the 2014 meeting of the International College of Neuropsychopharmacology. In Syria hundreds of years ago the drug was named ganzigunnu, meaning “the drug that takes away the mind.” It has also been called azalla, meaning “hand of the ghost.” Among the 100 compounds in marijuana, the best-known ingredient is delta-9-tetrahydrocannabinol (delta-9 THC), which produces most of the actions of the drug. There is another active ingredient, cannabidiol (CBD), which has calming and anti-anxiety effects, but is present in very low levels.
The brain has cannabinoid receptors that respond to ingredients in marijuana in addition to other chemicals produced in the brain. They modulate calcium ions and decrease the release of many neurotransmitters.
THC acts at CB-1 receptors, producing the high. The CB-1 receptor is synthesized on demand, post-synaptically, and is transferred to the pre-synaptic terminal where it decreases calcium and transmitter release. Consistent with marijuana’s appetite-stimulating properties (“the munchies”), if the CB-1 receptor is blocked in animals, they lose their appetite and die of hunger.
There are also low levels of CB-2 receptors in the brain, whose activation does not cause a high, and whose levels may increase dramatically in pathological situations. Activation of the CB-2 receptor is anti-inflammatory and, in the same way that the immune system acts against foreign proteins, CB-2 acts as a protector against non-proteins.
CBD does not bind to any cannabinoid receptors, but its actions are blocked by cannabinoid antagonists.
There are two chemicals in the brain (endogenous ligands) that act at cannabinoid receptors—anandamide and 2-arachidonoylglycerol (2-AG). They are soluble only in lipids (not in water), and have never been given to people. In animals, 2-AG has neuroprotective effects, decreases the size of a stroke by 60%, and increases recovery from stroke.
Marijuana and CBD in particular have also had beneficial effects in people. Marijuana decreases the nausea and vomiting associated with chemotherapy in children, has anti-inflammatory effects in rheumatoid arthritis (decreasing inflammatory marker TNF alpha), and has anti-diabetes and anti-convulsant effects.
In 2012, researcher F. Markus Leweke and colleagues showed that CBD was about as effective as the atypical antipsychotic amisulpiride in alleviating the psychotic symptoms of schizophrenia. CBD’s other effects include reducing anxiety and improving psoriasis by increasing DNA methylation (Pucci et al. 2013).
It seems possible that some of these myriad effects of marijuana and endogenous ligands at CB receptors could be exploited for clinical therapeutics, as Mechoulam endorses, but when and how that will take place remains an unanswered question.
Editor’s Note: Despite all these potential positives of CBD, it should be noted that its levels are very low in marijuana, and that heavy smoking of marijuana has substantial adverse effects. These include low motivation, a doubling of the risk of psychosis, a hastening of the onset of bipolar disorder and schizophrenia, and cognitive impairment, as well as some changes in brain structure seen via magnetic resonance imaging (MRI). It may be becoming legal in many states, but is a bad idea for those at high risk for mood, anxiety, or bipolar disorders or for schizophrenia.
Synthetic Marijuana Comes with Serious Risks, Including Risks to Fetus
Synthetic marijuana, otherwise known as spice, skank, or K2, is not only vastly more potent than the tetrahydrocannabinol (THC) in marijuana plants, but it also lacks cannabidiol (CBD), the calming, antipsychotic substance also present in the plants. This makes spice much more likely to induce major psychiatric effects.
New evidence links use of spice during pregnancy to a tragic birth defect, anencephaly, or absence of the cerebral cortex. It can also lead to the later development of attention-deficit hyperactivity disorder, learning disabilities, memory impairment, depression, and aggression.
of spice during pregnancy to a tragic birth defect, anencephaly, or absence of the cerebral cortex. It can also lead to the later development of attention-deficit hyperactivity disorder, learning disabilities, memory impairment, depression, and aggression.
Effects of THC on gestation may occur as early as two weeks after conception, meaning by the time a woman realizes she is pregnant, the fetus may have been harmed by exposure to the drug.
Other new finding associate use of spice with acute coronary syndrome and the kind of acute kidney injury that can lead to the organ shutting down.
Editor’s Note: It has now been found that synthetic marijuana, or spice, can lead to psychosis, delirium, acute coronary syndrome (heart attack) in young people, and now kidney dysfunction, in addition to causing birth defects if used by pregnant women. Not only is spice made up of more potent THC without the calming effects of CBD, but it is often laced with unknown contaminants, which are likely the cause of the heart and kidney damage.
Smoking regular marijuana is bad enough—it doubles the risk of psychosis and may precipitate the onset of schizophrenia. It may also cause long-lasting effects on cognitive function. Since many states are legalizing marijuana, it is important to know the risks. In any case the risks are much more serious with the synthetic product, and synthetic marijuana should be avoided at all costs.
Mobile Apps and Other Technologies May Make It Easier to Track Mood Symptoms Longitudinally
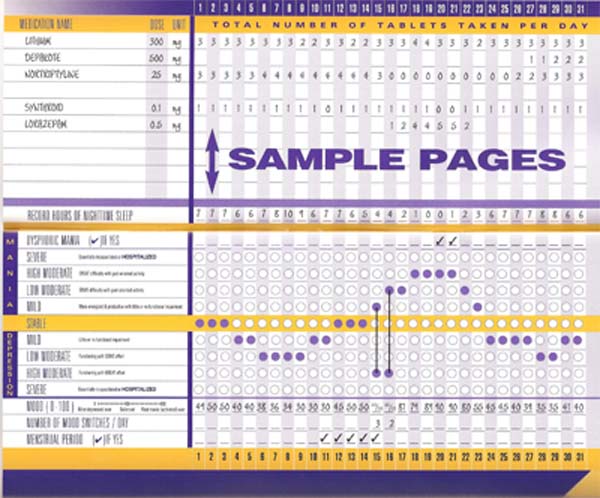
Multiple investigative groups at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011 reported on the use of mobile phones or other automated processes to provide a more detailed ongoing record of a patient’s mood fluctuations and response to treatment. A particularly notable study by Nolen and colleagues described an electronic version of the life chart method (e-LCM) that would be accessible via internet, and which could be integrated with the patient’s file and used for research. These investigators developed software for a patient version and a clinician version. The web-based version is not yet available for patient use.
Editor’s Note: Until this and other useful electronic monitoring procedures become available, we recommend using the written version of a life chart to provide daily assessments of mood, side effects, and comorbid symptoms in order to provide a detailed numerical and graphic record with which to judge treatment response. This method is extremely valuable in developing new treatment approaches for those with treatment-resistant illness, and if patients keep these records, physicians will have optimal and detailed input in order to assess response and make treatment recommendations.
My Mood Monitor provides another available approach. This system was developed primarily as a screening instrument, but also includes a longitudinal monitoring component. It is not designed for daily monitoring, but can be used repeatedly with a minimal interval of one week between ratings.
We’ve written before about depressioncheck, My Mood Monitor’s iPhone app that can quickly screen for mood and anxiety disorders.
Sleep Apnea Common Among Rapid Cyclers
Kellen and colleagues presented a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, in which they reported that 21% of patients with rapid cycling bipolar disorder have confirmed sleep apnea. Since many patients who screened positive for sleep apnea on the study’s sleep questionnaire did not undergo follow-up sleep studies to confirm the diagnosis, it is estimated that up to 40% of rapid cycling patients may, in fact, have sleep apnea.
Editor’s note: Given such a high incidence of sleep apnea among rapid cycling bipolar patients, it would be prudent for patients and clinicians to be alert to the possibility of sleep apnea and follow up with appropriate sleep studies. Sleep apnea can cause daytime fatigue, cognitive dysfunction, and treatment resistance, so its identification and treatment with continuous positive airway pressure (CPAP) may be enormously beneficial to a substantial number of rapid cycling bipolar patients. A just-published article by Sukys-Claudino in Sleep Medicine presents findings that compared to placebo, the anti-Alzheimer’s drug donepezil (Aricept) started at 5mg/day for 2 weeks and then increased to 10 mg given twice a day (20 mg/day total) helped all measures of sleep apnea including daytime sleepiness.
Clinical hints that a patient may be suffering from sleep apnea include loud snoring, long pauses between breaths, and non-restorative sleep. The likelihood of sleep apnea increases with age and with overweight or obesity.
Antioxidants May Be Deficient in Patients with Bipolar Disorder, NAC May Help
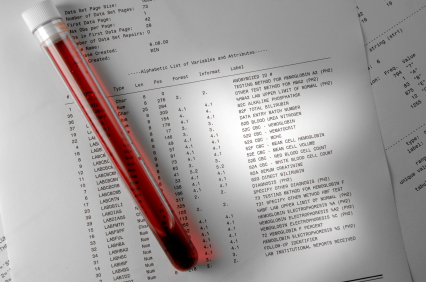
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Guy Goodwin and colleagues reported that relative to controls, blood from patients with bipolar disorder contained more total glutathione, a potent antioxidant, and a higher ratio of oxidized to reduced glutathione. Measurements of blood glutathione could eventually serve as a biomarker, suggesting when a diagnosis of bipolar disorder is likely.
Editor’s note: Glutathione is one of the major antioxidants in humans. Oxidized glutathione is a less active form, so the higher levels of oxidized glutathione compared to reduced glutathione in patients with bipolar disorder suggests they may have a relative deficiency of the active form. These data are consistent with reports that patients in manic and depressive phases of bipolar disorder have increased oxidative stress and free radicals that impair cellular functioning.
Together, these results highlight the potential utility of treatments that increase antioxidant activity. One option is N-acetylcysteine (NAC), which the body converts into glutathione. As previously noted in the BNN, Michael Berk reported in Biological Psychiatry in 2008 that NAC (1000 mg twice a day) appears to exert greater antidepressant effects over a period of 24 weeks than placebo when added into previously ineffective regimens in patients with bipolar disorder.
In another poster at the conference, Magalhaes and colleagues reported on NAC treatment for a subgroup of the bipolar patients in the study by Berk who were in a major depressive episode at the time of the study. They found that NAC had highly significant acute antidepressant effects of large magnitude in this subgroup of patients.
The glutathione data by Goodwin et al. provide a further rationale for consideration of the use of NAC in bipolar disorder, particularly in the acute and longer-term treatment of the depressive phases. As we reported in BNN Issue 1 from 2010, NAC also exerts positive effects in many illnesses that commonly occur comorbidly with bipolar disorder. These include cocaine and heroin addiction, gambling addiction, obsessive compulsive disorder (as an adjunct to selective serotonin reuptake inhibitors (SSRIs)), and trichotillomania (compulsive hair-pulling).
Valproate Can Cause Increases in Blood Ammonia
 Researcher C. Lewis reported in two posters presented at the Ninth International Conference on Bipolar Disorder (ICBD) in 2011 that in a study of patients treated with valproate, some increases in ammonia levels occurred. This condition, hyperamonaemia, was identified in 31 patients among those treated between 2005 and 2009 at the Cleveland Clinic in Cleveland, Ohio. High levels of ammonia are associated with a flapping tremor and, in some cases, encephalopathy with confusion, psychiatric symptoms, and motor incoordination.
Researcher C. Lewis reported in two posters presented at the Ninth International Conference on Bipolar Disorder (ICBD) in 2011 that in a study of patients treated with valproate, some increases in ammonia levels occurred. This condition, hyperamonaemia, was identified in 31 patients among those treated between 2005 and 2009 at the Cleveland Clinic in Cleveland, Ohio. High levels of ammonia are associated with a flapping tremor and, in some cases, encephalopathy with confusion, psychiatric symptoms, and motor incoordination.
The recommended management for hyperamonaemia is discontinuation of valproate and use of lactulose, a synthetic sugar that can lower ammonia levels. These approaches were not always used. Another option for patients who require valproate treatment is to supplement the drug with carnitine, which is available as a nutritional supplement. Lewis reported success in three such cases.
Editor’s Note: Patients on valproate presenting with a gross flapping tremor of the hands, confusion, or motor imbalance should be tested for hyperamonaemia and treated accordingly.