DRAMATIC PROPHYLACTIC RESPONSE TO NIMODIPINE: A Case Report
(This is an invited contribution by Robert Westhead.)
This 50 year old man had a lifetime of incapacitating rapid cycling (10 days up and 10 days down) bipolar I disorder, but then for the past 4 years has had a complete remission on nimodipine (60mg QID). He remains on lithium (800mg), and of his other long-term medications, he has titrated quetiapine down from 800mg to 50mg and has discontinued phenelzine.
He had previously failed to respond to combinations of:
· Lithium
· Anticonvulsant mood stabilizers (including divalproex sodium, lamotrigine, carbamazepine and pregablin)
· Atypical antipsychotics (including quetiapine, aripiprazole and lurasidone)
· Antidepressants (including SSRIs eg citalopram and sertraline, NSRIs eg venlaflaxine and mirtazapine, and a MAOI eg phenelzine)
· Thyroxine
· Propranolol
· Clonazepam
He wanted to highlight this dramatic response to nimodipine in combination with lithium as this dihydropyridine calcium channel blocker is not well known or frequently used for its prophylactic effectiveness.
He noted that as well as stopping the rapid cycling, the nimodipine has provided complete relief from comorbid social anxiety symptoms and remediated cognitive and memory impairment.
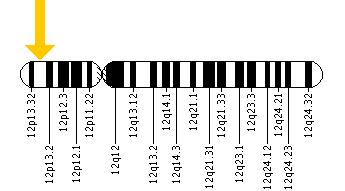
This response to nimodipine potentially also has pathophysiological implications. Nimodipine directly blocks the CACNA1C calcium influx gene that has repeatedly been associated with vulnerability to depression, bipolar disorder, and schizophrenia in gene wide association studies. This patient does not know whether he carries this gene variant, but assays for it are routinely available as performed by the company Genomind.
Thus, it remains an open question as to whether those who have the CACNA1C variant would be more responsive to nimodipine compared to those without the variant. Certainly, the efficacy of this agent in treatment of patients with bipolar disorder deserves further consideration and study.
Nimodipine Decreases Frontal and Parietal Cortical Activity During Working Memory in Healthy Subjects
At a recent scientific meeting, researcher Kristin Bigos and colleagues described the effects of nimodipine, a treatment for brain hemorrhage, on the brain during working memory tasks. Nimodipine is a dihydropyridine L-type calcium channel blocker. Calcium channel blockers prevent calcium from entering cells in the heart and blood vessel walls, and they are often used to treat high blood pressure.
Nimodipine acts on the CACNA1C calcium influx gene. Certain genetic variations in this gene (particularly the rs1006737 A allele) have been linked to vulnerability to bipolar disorder, schizophrenia, depression, and autism. Carriers of the risk allele also have higher CACNA1C mRNA expression in the dorsolateral prefrontal cortex and exhibit more activity in the frontal and parietal regions of the brain during working memory tasks, suggesting inefficient brain processing in these regions. Bigos and colleagues found that 60mg/day of nimodipine decreased frontal and parietal cortical activity by 39.1% and 42.8%, respectively, during a working memory task, suggesting that nimodipine improved the efficiency of memory processing. Nimodipine’s positive effects were greater in those participants who had the CACNA1C risk allele.
Editor’s Note: Using a placebo-controlled off-on-off-on study design (meaning patients took placebo for a period, then nimodipine, then placebo again and nimodipine again), this editor (Robert M. Post), Peggy J. Pazzaglia and colleagues found that nimodipine had positive effects in both mania and depression in patients with bipolar disorder (described in the 2008 book Treatment of Bipolar Disorder: A Casebook for Clinicians and Patients by Robert M. Post and Gabriele S. Leverich). In a large randomized study of patients with bipolar disorder presented by Haroon R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry, lithium was associated with about a 50% response rate while the combination of lithium and nimodipine was associated with a 73% response rate.
It remains to be seen whether people with bipolar disorder who have the CACNA1C risk gene would respond better to nimodipine than those without the risk gene, and whether it would improve working memory more in the subgroup with the risk gene.
Making Lithium Treatment More Tolerable For Patients
 In a slideshow at Psychiatric Times, Chris Aiken describes seven ways to improve lithium’s tolerability. Since many researchers, including BNN Editor-in-Chief Robert M. Post, have suggested that lithium should be used more often as a treatment for bipolar disorder, ways of making its side effects more manageable are of great interest. Here we summarize Dr. Aiken’s seven points and add a few perspectives of our own.
In a slideshow at Psychiatric Times, Chris Aiken describes seven ways to improve lithium’s tolerability. Since many researchers, including BNN Editor-in-Chief Robert M. Post, have suggested that lithium should be used more often as a treatment for bipolar disorder, ways of making its side effects more manageable are of great interest. Here we summarize Dr. Aiken’s seven points and add a few perspectives of our own.
Aiken writes that “when it comes to the side effects that matter most to patients—sedation, weight gain, and cognition—lithium’s tolerability ranks right behind lamotrigine.” In fact, lithium plus lamotrigine is an excellent combination, as lithium excels at preventing manias while lamotrigine excels at depression prevention.
Post’s philosophy is that many of lithium’s side effects can be avoided in the first place through judicious dose titration. He suggests gradually increasing dosage, and stopping before side effects become difficult, or reducing a dosage that has already become a problem. The idea is to avoid lithium side effects even if blood levels of lithium remain below clinically therapeutic levels. Post suggests using lithium at whatever dose is not associated with side effects.
Many of lithium’s positive therapeutic effects emerge at low doses, and if this improvement is insufficient, the rest of the needed efficacy can be achieved by adding other medications. As noted above, lamotrigine is a good option for break-through depression, as is lurasidone. For breakthrough mania, the mood stabilizers valproate and carbamazepine or an atypical antipsychotic can be added to lithium.
A little-appreciated option for enhancing lithium’s mood stabilizing effects is nimodipine, a dihydropyridine calcium blocker. It has both antimanic and antidepressant efficacy without lithium’s side effects. Research showed that a year on the combination of lithium and nimodipine was more effective than a year of either drug alone.
If a patient taking lithium experiences a tremor at a dose that is not fully effective, nimodipine can be added in order to lower the lithium dose enough to eliminate the tremor.
Nimodipine specifically blocks the calcium influx gene CACNA1C that has been repeatedly been associated with the vulnerability to bipolar disorder and depression.
If side effects do occur on lithium, they can often be managed. The following suggestions are adapted from Aiken’s article with input from Post. Read more
More News About Genetic Risk for Bipolar Disorder
In a 2017 article in the Journal of Clinical Psychiatry, researcher Paul E. Croarkin and colleagues describe findings from their study of genetic risk factors for early-onset bipolar disorder. The researchers focused on single nucleotide polymorphisms (SNPs), which are variations in a single base pair of a DNA sequence. SNPs are normal variations or copying errors that occur when DNA is replicated. Croarkin and colleagues tracked 8 SNPs that had been linked to bipolar disorder in previous studies. They examined 69 patients from a study of early-onset mania, 732 adult patients with bipolar disorder (including 192 with early-onset illness), and 776 healthy controls. The researchers compared patients with early-onset illness to controls, and also looked for connections between specific SNPs and early-onset illness.
The SNPs analyzed in the study map to three genes that have repeatedly been associated with the risk for bipolar disorder in other studies. These include CACNA1C (one of several genes that create calcium channels), ANK3, and ODZ4. Croarkin and colleagues determined that the presence of these SNPs, particularly the ones that involved the CACNA1C gene, were associated with early-onset bipolar disorder.
Editor’s Note: These findings may lead to better treatment for early-onset bipolar disorder. The CACNA1C calcium influx gene that has repeatedly been connected to bipolar illness can be blocked by the calcium channel blocker nimodipine. Nimodipine has lithium-like effects in mania and depression in adults. One case report by Pablo A. Davanzo in the Journal of Child and Adolescent Psychopharmacology described success using nimodipine and the thyroid medication levothyroxine to treat a 13-year-old boy with very rapid cycling bipolar disorder that had previously failed to respond to multiple medications.
Nimodipine deserves further study in children showing symptoms of bipolar disorder. The company Genomind provides testing for the CACNA1C gene. We hope it will soon be determined whether the presence of this SNP predicts a good response to nimodipine.
Being able to predict who will get bipolar disorder is a long way off. However, there are some clear risk factors. Young people from families that have had several generations of bipolar disorder or related disorders are at increased risk for bipolar disorder. This risk increases for children who experience adversity in childhood, such as abuse or neglect. The presence of early mild symptoms of mania, depression, or disruptive behavior further increase this risk.
For doctors, a patient’s clinical history of these three types of risk factors can help identify whether they are at increased risk of developing bipolar disorder. Patients with several risk factors should be observed closely and treated with psychotherapy or medication as needed.
Parents of children between the ages of 2 and 12 who have shown some signs of mood or behavioral symptoms are encouraged to join our Child Network. We provide a secure online platform where parents record their children’s symptoms of anxiety, depression, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania on a weekly basis. Symptoms are charted over time in a graphical depiction that can be shared with the child’s doctor. For more information, see page 11 of this issue. To join, visit our website bipolarnews.org and click on the tab for the Child Network.
Gene CACNA1C is Associated with Early-Onset Bipolar Disorder
Several genes have previously been implicated in bipolar illness. In a recent study, researchers at the Mayo Clinic, led by Paul Croarkin, compared variations in three genes (CACNA1C, ANK3, and ODZN) across 69 children aged 6–15 with mania, a 776-person control group from the Mayo Biobank database, and 732 adults with bipolar disorder (some with onset in childhood and adolescence and some with onset in adulthood, also from the Biobank). All participants were Caucasian, to minimize confounding by population stratification. The researchers found that the minor allele of rs10848632 in CACNA1C was associated with childhood onset of bipolar disorder. The haplotype (or sequence of nucleotides) T-G-G-T was the one associated with risk. Genetic risk scores were also associated with early onset of illness.
Editor’s Note: In research by Michael McCarthy and colleagues, CACNA1C has been linked to abnormal circadian rhythms in bipolar disorder and to responsiveness to lithium treatment. Together, these data suggest the importance of studying the calcium channel blocker nimodipine (which blocks calcium influx through CACNA1C) in childhood-onset bipolar disorder. A 1999 case report by Pablo A. Davanzo and colleagues described a teenager with ultra rapid cycling bipolar disorder (multiple mood switches/day) that did not respond to a host of conventional medications, who improved dramatically on nimodipine, reaching remission. This author (Robert M. Post) has also seen confirmed responsivity in adults with rapid cycling bipolar disorder (reported in the 2008 book Treatment of Bipolar Illness: A Casebook for Clinicians and Patients, by Post and Gabriele S. Leverich).
Calcium Channel May Be Responsible for Circadian Rhythm Abnormalities in Bipolar Disorder
Genetic variation in L-type calcium channel genes have been linked to bipolar disorder. Since calcium plays an important role in circadian rhythms, abnormalities in the calcium channel in bipolar disorder could explain some of the circadian rhythm disturbances patients with bipolar disorder exhibit. New research by Michael McCarthy and colleagues shows that calcium channels in general, and the gene CACNA1C in particular, affect signaling pathways that regulate circadian rhythms in both human and animal cells. The researchers also found that calcium channels affected how lithium changes circadian rhythms, suggesting a mechanism by which the treatment may work. They suggest that drugs that affect the L-type calcium channel may be promising treatments for bipolar disorder.
Editor’s Note: The L-type calcium channel blocker nimodipine has had antidepressant, antimanic, and anticycling effects in some patients with bipolar disorder in small studies both by Peggy Pazzaglia and colleagues (including this author Robert Post) and a larger randomized study by Haroon R. Chaudhry.
The clinical effects of nimodipine results thus align with studies linking the CACNA1C gene to bipolar illness and its early onset, increased expression of the gene in the brain of bipolar patients in autopsy studies, increased levels of calcium in white cells of bipolar patients, and a variety of other neurobiological phenomena observed in normal controls carrying the risk gene.
The new link found between CACNA1C and circadian rhythms further links the L-type calcium channel abnormality and bipolar disorder, as well as the therapeutic effects of the L-type calcium channel blocker nimodipine. This drug deserves further study, especially in those with the genetic variation in CACNA1C that has been linked to bipolar disorder.
Gene for Calcium Channel Linked to Bipolar Disorder in Several Ways
No one gene explains the risk of developing bipolar disorder. Many genes are involved, each with a small effect. However, the effects of one particular gene have been validated in multiple different ways. The gene is called CACNA1C, and it codes for one subunit of the dihydropyridine L-type calcium channel. Calcium channels are structures on the membranes of neurons that allow calcium to enter cells and alter their excitability.
Different people can have different variants of the CACNA1C gene, depending on which nucleotides appear there: valine (Val) or methionine (Met). One particular variant (known as the Met/Met single nucleotide polymorphism, rs1006737) has been associated with executive function deficits compared to the Val/Val variant in multiple tests in patients with bipolar disorder. Executive function refers to abilities like planning, organizing, and retaining information. This was reported by Soeiro-de-Souza et al. in the journal Acta Psychiatrica Scandinavica in 2013.
Importantly, CACNA1C has also been linked to risk of bipolar disorder, a finding that was replicated in several large genome-wide association studies (GWAS). Autopsy studies of people who had been diagnosed with bipolar disorder show more calcium channels in their brains. The Met/Met variant of the CACNA1C gene also lets more calcium ions into cells. Those who have the gene variant also show differences in some brain structures known to be involved in the modulation of emotions compared to those without the variant.
In addition to these findings, more than a dozen studies report increased intracellular calcium in the white blood cells of people with bipolar disorder compared to controls. To the extent that these increases in intracellular calcium reflect changes in neurons, this would be consistent with the findings about CACNA1C. High levels of calcium influx and the associated intracellular calcium may increase cellular excitability and potentially dysregulate normal neuronal functioning.
The final piece of evidence linking altered calcium channel regulation to bipolar disorder is a direct therapeutic test of a drug that blocks calcium influx through the dihydropyridine L-type calcium channel. There is evidence that nimodipine, which selectively blocks dihydropyridine L-type calcium channels, has therapeutic effects in bipolar disorder.
Genetic Risk Factors for Onset of Bipolar Disorder
A Genetic Risk Factor For Bipolar Disorder: The CACNA1C Gene
In an abstract presented at the 5th Biennial Conference of the International Society for Bipolar Disorders, Sophia Frangou reported on the CACNA1C polymorphism, a genetic variation that has been associated with the risk of developing bipolar disorder in several genome-wide association studies that search for links between genes and illnesses. Frangou found that those people with the genetic variation had increased volume in some parts of the brain, including the right hypothalamus and the right amygdala, and decreased volume in others, including the putamen, as well as alterations in the functional connectivity of different cortical areas.
These data may be related to findings that calcium influx may play a role in bipolar disorder. In people with the genetic variation, the risk allele binds to a subunit of the voltage-dependent calcium channel, which modulates the influx of calcium from the outside to the inside the neuron.
Increased amounts of calcium are consistently found in the white cells and platelets of patients with bipolar disorder compared to controls. Moreover, the drug nimodipine, a dihydropyridine L-type calcium channel blocker, is effective in the prevention of manic and depressive episodes in a subgroup of patients, particularly those with cycling patterns that are ultra-rapid (4+ episodes per month) or ultradian (including a mood switch within a 24-hour period 4+ times per month). A large randomized study of patients with bipolar disorder presented by H.R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry also found that while lithium was associated with a 50% response rate, the combination of lithium and nimodipine was associated with a 73% response rate, again suggesting the additional efficacy of blocking L-type calcium channels.
Immune Abnormalities May Predict Onset of Bipolar Disorder in Children at High Risk
At the 5th Biennial Conference of the International Society for Bipolar Disorders E. Mesman discussed connections between immunity and bipolar disorder. Mesman and colleagues followed offspring of parents with confirmed bipolar disorder for 12 years and compared them to children in the general population. In the children of bipolar parents they found higher levels of immune markers called cytokines (PTX3 and sCD25) in circulating monocytes, a type of white blood cell. In the children of bipolar parents they also found a high inflammatory setpoint in the monocytes. T-effector and T-regulatory cells were also different in the offspring of bipolar parents.
While these findings were present in children who had already become ill with bipolar disorder, they were also present in those who had yet to experience a mood disorder, suggesting that these immune and inflammatory markers may ultimately be an important risk marker for the onset of bipolar disorder.
Editor’s Note: These are among the first studies suggesting that immune and inflammatory abnormalities may precede the onset of bipolar disorder. Many studies have shown that patients with active bipolar disorder show more inflammation, including increases in inflammatory markers interleukin 1 (IL-1), interleukin 6 (IL-6), C reactive protein (CRP), and tumor necrosis factor alpha (TNFa). The new data are of considerable importance not only because inflammation could serve as a marker of illness onset, but also because inflammation could become a potential target for therapeutics (i.e. using anti-inflammatory and immune-suppressing agents to treat bipolar disorder).
Dopamine D2 and D3 Agonist Pramipexole May Enhance Cognitive Function in Bipolar I Disorder
Anil Malhotra from the Zucker Hillside Hospital found that pramipexole (Mirapex), a dopamine D2 and D3 agonist used in the treatment of Parkinson’s disease, improved measures of processing speed and working memory in euthymic bipolar patients (whose average age was 42) when compared with placebo in an adjunctive clinical trial.
Editor’s Note: Bipolar patients in a euthymic phase have consistently been shown to have some degree of cognitive dysfunction that is typically correlated with the number of prior depressive and/or manic episodes they have experienced. This is one of the first studies to directly target this cognitive dysfunction with a pharmacotherapeutic agent.
Pramipexole may be of additional value among depressed patients, because in two small, placebo-controlled studies, one led by Carlos Zarate at the National Institute of Mental Health and one led by Joseph F. Goldberg in New York, pramipexole has been shown to exert acute antidepressant effects in bipolar patients in the depressive phase of the illness. The new data from Malhotra raise the possibility that there could be a two-for-one benefit when pramipexole is used in the depressive phase of bipolar illness—improvement in both depression and cognition.
Other approaches to improving cognition in patients with bipolar disorder
The Role of Calcium in Genetic Vulnerability, Pathophysiology, and Treatment Of Bipolar Illness
One of the most consistent findings in biological psychiatry is that levels of intracellular calcium in blood elements (platelets and white cells) are higher than normal in patients with mood disorders, particularly bipolar disorder. These data are now supported by genome-wide association studies that have identified a relationship between alterations in a calcium channel and vulnerability to bipolar illness. The specific alteration is in the alpha-IC subunit of the L-type calcium channels, otherwise referred to as CACNA1C. These findings were initially reported by one group funded by the Welcome Trust, a charitable organization that funds health research, in a series of studies that included thousands of patients and controls. Investigator Pamela Sklar later replicated these findings in another large independent sample.
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry, investigator Tyson Tragon reported that there were higher levels of CACNA1C in the cingulate cortex in autopsy specimens of those with bipolar illness than in controls. In a study of mice, some of which had the gene for the glutamate receptor subunit GLuR6 knocked out (i.e. production of the gene was artificially limited), the researchers found that the L-type dihydropyridine calcium channel blocker nimodipine decreased hyperactivity, amphetamine super-sensitivity, risk-taking behavior, and aggression in those with the gene removed. The dihydropyridine-type drugs like nimodipine also decreased stress-related immobilization in the wild type (the animal with normal genes) but not the knockout animals (the ones lacking GLuR6). These data suggest that alterations in a subunit of the dihydropyridine-responsive L-type calcium channel are a risk factor for bipolar illness, a brain abnormality in those who have the illness, and relevant to behavioral/pharmacological models.
Several research groups have noted that treatment with the L-type calcium channel blocker nimodipine (Nimotop) can sometimes have positive effects in mania and depression in those poorly responsive to lithium carbonate. This has been documented by Pazzaglia and Post in double blind off-on-off-on clinical trials (i.e. during off trials patients received placebo and during on trials patients received nimodipine, but the raters were unaware which pill the patient had received). In several instances, a positive response continued when the patient was switched from nimodipine to another dihydropyridine, isradapine (DynaCirc), but not when patients were switched to a different L-type calcium channel blocker, the phenylalkylamine verapamil (sold under the names Calan, Covera, Isoptin, and Verelan), which acts at a slightly different site on the channel. Read more