No Relationship Between SSRIs in Pregnancy and Stillbirths or Neonatal Mortality
 Much has been written about the use of selective serotonin reuptake inhibitor (SSRI) antidepressants during pregnancy. In a review of 920,620 births in Denmark (1995 to 2008) that Jimenez-Solem published this year in the American Journal of Psychiatry, no link was found between any of the SSRIs used in any trimester and risk of stillbirth or neonatal mortality. The only exception was a possible association of three-trimester exposure to citalopram and neonatal mortality.
Much has been written about the use of selective serotonin reuptake inhibitor (SSRI) antidepressants during pregnancy. In a review of 920,620 births in Denmark (1995 to 2008) that Jimenez-Solem published this year in the American Journal of Psychiatry, no link was found between any of the SSRIs used in any trimester and risk of stillbirth or neonatal mortality. The only exception was a possible association of three-trimester exposure to citalopram and neonatal mortality.
Editor’s Note: These new data may be of importance to women considering antidepressant continuation during pregnancy when there is a high risk for a depressive relapse. A maternal depressive episode (like other stressors such as anxiety or experiencing an earthquake) during pregnancy does convey adverse effects to the child, so appropriate evaluation of the risk/benefit ratio or staying on an antidepressant through a pregnancy is important.
Folic Acid Supplementation Not Linked To Cancer
 Folic acid is often recommended for patients with difficult-to-treat depression and for pregnant women. A recent study suggested that when taken before and in the first weeks of pregnancy, the vitamin supplement can reduce the risk of autism in the child. However, some concern was raised after a 2007 study that suggested a possible link between folic acid and cancer risk. New research indicates that cancer is not a risk of folic acid supplementation.
Folic acid is often recommended for patients with difficult-to-treat depression and for pregnant women. A recent study suggested that when taken before and in the first weeks of pregnancy, the vitamin supplement can reduce the risk of autism in the child. However, some concern was raised after a 2007 study that suggested a possible link between folic acid and cancer risk. New research indicates that cancer is not a risk of folic acid supplementation.
In a meta-analysis that analyzed data from 13 different trials of folic acid that included a total of over 49,000 patients, no increased risk of cancer was found in patients taking folic acid. The meta-analysis was published this year in the Lancet.
Editor’s Note: In addition to folic acid’s beneficial effects during pregnancy, it can also enhance the effects of antidepressants and mood stabilizers. The dose typically recommended for depression is 1mg for women and 2mg for men.
Fifteen percent of the population has an inefficient form of the enzyme methylenetetrahydrofolate reductase (MTHFR), which converts folate to methylfolate. For treatment of depression in these individuals, l-methylfolate should be used instead of regular folic acid.
Antiepileptic Drugs for Bipolar Disorder Do Not Increase Risk of Suicidal Behavior
![]() A 30-year observational study published by Andrew Leon and colleagues in the American Journal of Psychiatry has found that anticonvulsants used in epilepsy and for bipolar depression (carbamazepine, lamotrigine, and valproate) do not increase suicidal behavior in bipolar patients.
A 30-year observational study published by Andrew Leon and colleagues in the American Journal of Psychiatry has found that anticonvulsants used in epilepsy and for bipolar depression (carbamazepine, lamotrigine, and valproate) do not increase suicidal behavior in bipolar patients.
Editor’s Note: The FDA gave a warning in 2009 that these anticonvulsants were associated with suicidal ideation. This was based on studies of a mixed group of psychiatry and neurological patients in acute placebo-controlled studies, where suicidal ideation is typically a reason for exclusion from the study. Leon et al. used more powerful longitudinal methods to compare the risk of suicidal ideation in individuals taking and not taking anticonvulsants and found no such increase in suicidal behavior.
This is like the FDA warning for antidepressants and suicide, which was based on data from placebo-controlled clinical trials in acute depression (where suicidal patients are excluded). When investigators used the same longitudinal methods as Leon et al. in the anticonvulsant study, they found that antidepressants actually reduced suicidal behavior by 30%.
The bottom line is that the use of anticonvulsants for bipolar disorder should not be discouraged based on the FDA warning about suicidal ideation in mixed neurological and psychiatric patients. In bipolar patients, anticonvulsants do not increase the risk of suicidal behaviors, i.e. suicidal acts or completed suicides.
Despite the FDA Warning to the Contrary: Antidepressants Do Not Increase Suicidality
In 2007, the FDA began labeling antidepressants with a warning that patients aged 18-24 were at risk for increased suicidality during the first weeks of treatment. New evidence shows antidepressants actually have beneficial effects on suicide risk in adults. A study of all published and unpublished data on the SSRI fluoxetine (Prozac) and the SNRI venlafaxine (Effexor) published in 2012 by Gibbons et al. in the Archives of General Psychiatry showed that these antidepressants substantially reduced suicidal thoughts and behavior in adults and produced no increase in suicidal thoughts or behavior in children and adolescents.
The protective effect on suicidality in adults was mediated by mood, i.e. the patients’ mood improved and they became less suicidal. Children’s mood also improved on the antidepressants, but their risk of suicidal ideation did not change.
Editor’s Note: These are important findings. When the FDA box warning on antidepressants and suicidal ideation appeared, antidepressant treatment of youth decreased without an accompanying increase in psychotherapy, and the actual suicide rate in youth increased.
We now know that childhood-onset depression carries a bigger risk for a poor outcome in adulthood than adult-onset illness. In parallel, greater numbers of depressions are associated with more impairment, disability, cognitive dysfunction, medical comorbidities, treatment resistances, and neurobiological abnormalities.
It is important to treat illness in young people in order to prevent these difficulties, and the suicide warning should not deter the use of antidepressants. Patients should be careful about suicidal ideation in the first several months after starting an antidepressant, as other data suggest that this is a time of slightly increased risk of suicidal thoughts in children and adolescents.
Vitamin D3 Is Low In Children And Adolescents With Mania, But Supplements Help
Vitamin D3 is low in children and adolescents with mania, but taking a supplement could help. Vitamin D3, which we absorb via food and sunlight, is converted by the liver to a form called 25-OH-D. In a small study, Elif Sikoglu et al. found that children and teens with mania had lower levels of 25-OH-D in their blood compared to typically developing youth of similar ages. This deficit was associated with lower brain GABA levels measured with magnetic resonance spectroscopy. GABA dysfunction has been implicated in the manic phase of bipolar disorder. An 8-week trial of Vitamin D3 supplements significantly reduced manic symptoms and tended to increase GABA levels.
Editor’s Note: Other data have suggested that children with psychosis have low Vitamin D3, and in a recent clinical trial in adults, Vitamin D3 supplementation improved antidepressant response more than placebo. Many children in the US are Vitamin D deficient. Test them and, if necessary, treat them, especially if they have bipolar disorder.
Vitamin D3 has Positive Effects in Depressed Patients on Prozac
A recent study of patients taking fluoxetine (Prozac) for major depression found that adding 1500 IU of vitamin D3 to their treatment regimen improved their response significantly. The article was published in the Australian and New Zealand Journal of Psychiatry.
According to the Mayo Clinic:
The term “vitamin D” refers to several different forms of this vitamin. Two forms are important in humans: ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Vitamin D2 is synthesized by plants. Vitamin D3 is synthesized by humans in the skin when it is exposed to ultraviolet B (UVB) rays from sunlight. Foods may be fortified with vitamin D2 or D3.
Editors Note: Here is another augmenting agent that could be considered for the treatment of those with residual depression. While vitamin D has not been studied directly in bipolar depression, we could ask, “Why not try it?” Other nutritional supplements in this category might be folate and N-acetylcysteine.
Vitamin D supplements are definitely indicated for the large percentage of those in the US who are vitamin D deficient. Given the data from this randomized trial, vitamin D3 could be considered in those with normal levels of vitamin D as well.
Folic Acid During Pregnancy May Lower Autism Risk
 A study of 85,000 children in Norway that was recently published in the Journal of the American Medical Association showed that women who took folic acid during pregnancy were 40% less likely to have a child who developed autism.
A study of 85,000 children in Norway that was recently published in the Journal of the American Medical Association showed that women who took folic acid during pregnancy were 40% less likely to have a child who developed autism.
A summary of the research by National Public Radio explained:
Folic acid is the synthetic version of a B vitamin called folate. It’s found naturally in foods such as spinach, black-eyed peas and rice. Public health officials recommend that women who may become pregnant take at least 400 micrograms of folic acid every day to reduce the chance of having a child with spina bifida.
The folic acid’s effect reduced the most severe cases of autism but did not seem to have an effect on the incidence of more mild forms, such as Asperger syndrome. The benefits were seen in those women who had been taking folic acid for 4 weeks before conception and continued to take the supplement during the first 8 weeks of pregnancy.
Family Environment, Cognitive Functioning, and Quality of Life Among Depressed Adolescents with Bipolar Disorder
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, Arman Danielyan presented a poster on psychosocial, cognitive, and behavioral characteristics of youth in a depressive phase of bipolar disorder. These adolescents had lower scores on a variety of measures.
Adolescents with bipolar depression had significantly lower scores on 7 of 10 family environment scales measuring the quality of family interaction, communication, and emotional tone. They also exhibited significant impairment in cognitive function, particularly executive functioning, and all domains of psychosocial health were substantially lower than US normative data.
The authors concluded that bipolar depression affects multiple domains of adolescents’ lives including their cognitive, psychosocial, and family functioning. This suggests that the involvement of the whole family in the treatment process would be beneficial.
The impaired cognitive functioning these young people face is associated with lower quality of life, and ways of addressing this better are clearly needed.
Editor’s Note: In a previous BNN we reported on the efficacy of Family Focused Therapy (FFT), which was pioneered by David Miklowitz. This therapy is effective for adolescents and adults with bipolar disorder and for adolescents who are at high risk for the disorder because of two factors: having a parent with the disorder and having preliminary symptoms of bipolar disorder not otherwise specified (BP-NOS), depression, or an anxiety disorder. Kiki Chang, a respected authority on child and adolescent psychiatry, recommends FFT for children and adolescents with bipolar disorder and those at high risk for it.
N-acetylcysteine (NAC) Also Effective in Unipolar Depression
In 2008, Michael Berk and colleagues showed that N-acetylcysteine (NAC) is effective as an adjunctive treatment for bipolar depression. At the 2012 meeting of the International Congress of Neuropsychopharmacology, Berk reported that NAC (1000 mg twice a day) was also effective in unipolar depression, significantly beating placebo in a randomized double-blind 12-week study.
Editor’s Note: NAC has a broad spectrum of clinical efficacy in bipolar and unipolar depression, negative symptoms of schizophrenia (such as apathy and withdrawal), irritability in autism, trichotillomania (compulsive hair-pulling), gambling addiction, obsessive-compulsive disorder, and many substance-abuse disorders, such as cocaine, heroin, alcohol, and marijuana.
How can one substance do all this? NAC has antioxidant effects, it turns into glutathione (an antioxidant that is the body’s main defense against oxidative stress and free radicals), it has neuroprotective effects (causing neurite sprouting), and it re-regulates glutamate in the reward area of the brain, the nucleus accumbens. Berk believes it is NAC’s antioxidant properties that produce its positive effects in such a range of illnesses, while this editor (Robert M. Post) favors the glutamate mechanism (as discussed in BNN Volume 14, Issue 1 from 2010 and Volume 16, Issue 1 from 2012) as an explanation of NAC’s effects.
Whatever its mechanism turns out to be, NAC is worthy of consideration as an adjunctive treatment. It is readily available from health food stores without a prescription, relatively inexpensive (less than $20 for 100 pills), and relatively well-tolerated. Minor gastrointestinal upsets were the most common reported side effect in the Berk’s clinical trial. However, this editor has had one patient experience a worsening of psychosis.
Editor Robert M. Post’s Personal Opinion About NAC
With the usual caveat that all treatment strategies discussed in the BNN must be evaluated and administered by a physician, it may be useful to consider adding NAC to a treatment regimen for a patient struggling with recurrent unipolar or bipolar depression, and/or a comorbid substance use disorder. Using conventional treatments early in the course of these disorders for acute treatment and for long-term prevention would be the first approach. For less than satisfactory acute responses, conventional adjunctive treatments (as recommended in treatment guidelines elsewhere) might be considered along with NAC, which in some cases can have a delayed onset of action. (Three months may be required to see maximal effects in bipolar disorder.)
Genetic Markers of Response to Lithium
 At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
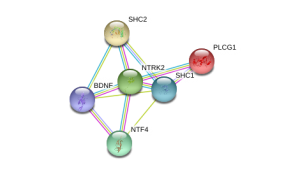
In his research Kelsoe found that a variant of the gene that codes for neurotrophic receptor type II (NTRK2), the receptor for brain-derived neurotrophic factor (BDNF), was associated with good response to lithium in patients with a family history of bipolar disorder or a history of euphoric mania. The “T” allele of rs1387923 was associated with better response to lithium retrospectively, and these results were replicated in a prospective study.
Editors Note: These data are among the first to indicate that genetic information could be used to make treatment decisions. Lithium increases BDNF and neurogenesis, thus it makes some sense that a variation in the BDNF receptor would affect clinical responsiveness to lithium.
In a similar vein, Janusz K. Rybakowski reported at the Society of Biological Psychiatry meeting on another possible predictor of long-term excellent response to lithium in bipolar disorder. Due to normal genetic variation, different people have different versions of BDNF. Rybakowski found that the patients with a version of BDNF known as Val66Val who had bipolar disorder performed significantly better on the Wisconsin Card Sorting Test, which evaluates abstract reasoning. However, he found that patients with a methionine amino acid in the place of one of the valine amino acids (resulting in a Val66Met allele, which is associated with minor cognitive difficulties) showed significantly better response to preventative treatment with lithium. It is noteworthy that these excellent lithium responders also performed better on a complex neuropsychological battery than those who were less good responders to lithium. The good responders’ performance on these tests was not different from healthy controls.
Editor’s Note: These data add to the possibility that prediction of lithium response is linked to common gene variations in neuroprotective factors or their receptors. It is interesting that the patients with the Val66Met allele, which works less efficiently, show the best long-term response to lithium. This is consistent with the view that lithium, which increases BDNF, is most effective in those who have a sluggish functioning of their BDNF due to having the Met allele. As we have written before, those with the Met allele have slight decrements in working memory, and in animal models, those with the Met allele show deficits in long-term potentiation (LTP), which suggest problems with long-term memory. Thus, using lithium to increase BDNF function in those with a “sluggish” variation in their BDNF makes sense and may ultimately be clinically useful.






