Omega-3 Fatty Acids Improve ADHD
 A 2017 systematic review and meta-analysis found that omega-3 fatty acid supplementation improves symptoms of attention-deficit hyperactivity disorder (ADHD) in children and adolescents. The article by Jane Pei-Chen Chang and colleagues in the journal Neuropsychopharmacology identified seven randomized controlled trials in which omega-3 fatty acids improved clinical symptoms of ADHD, and three trials in which omega-3s improved cognitive measures associated with attention.
A 2017 systematic review and meta-analysis found that omega-3 fatty acid supplementation improves symptoms of attention-deficit hyperactivity disorder (ADHD) in children and adolescents. The article by Jane Pei-Chen Chang and colleagues in the journal Neuropsychopharmacology identified seven randomized controlled trials in which omega-3 fatty acids improved clinical symptoms of ADHD, and three trials in which omega-3s improved cognitive measures associated with attention.
The meta-analysis also found that children and adolescents with ADHD have lower than normal levels of the omega-3s DHA and EPA, in addition to lower total levels of omega-3s measured in blood and cheek tissues.
Chang and colleagues suggest that omega-3 fatty acid supplementation is a potentially helpful and largely risk-free treatment option for ADHD in children and adolescents.
Eye Movement Desensitization and Reprocessing Can Improve PTSD
A 2014 meta-analysis of clinical trials showed that the therapeutic technique known as eye movement desensitization and reprocessing (EMDR) can reduce symptoms of post-traumatic stress disorder (PTSD). The meta-analysis also established that longer durations of EMDR treatment correlated with better outcomes.
The meta-analysis by Ying-Ren Chen and colleagues in the journal PLOS One evaluated 26 randomized controlled trials of EMDR in people with PTSD. Chen and colleagues found that EMDR reduced PTSD symptoms, depression, anxiety, and subjective distress.
EMDR is a psychotherapeutic technique intended to reduce the distress that a patient feels about a traumatic memory. The patient is encouraged to recall the traumatic event while focusing on an external stimulus. Typically this would mean using their eyes to track the therapist’s hand moving back and forth from left to right. This process can help patients reprocess the trauma and alleviate the stress that they feel upon recalling the traumatic memory.
Chen and colleagues found that EMDR sessions that lasted longer than one hour were more effective than those that lasted less than an hour. Another finding that was that groups led by therapists who were experienced in PTSD group therapy were more effective than groups led by therapists without that experience.
Other more recent research has established that traumatic memories can be reprocessed or even extinguished by making use of the memory reconsolidation window. Five minutes to one hour after a patient engages in active emotional recall of a traumatic memory, a window of time opens in which that memory is subject to reinterpretation and revision.
An experienced therapist can create a safe environment for a patient to recall traumatic events and find alternative ways of interpreting the experience—for example, by focusing on their strength in surviving the experience. This process resembles EMDR in many ways, but without the eye movements.
In a 2017 article in the journal Psychiatry Research, BNN Editor-in-Chief Robert M. Post and colleague Robert Kegan discuss the possibility of using the reconsolidation window to reprocess stressors that led to a depressive episode.
Proton Pump Inhibitors Linked to Gastric Cancer
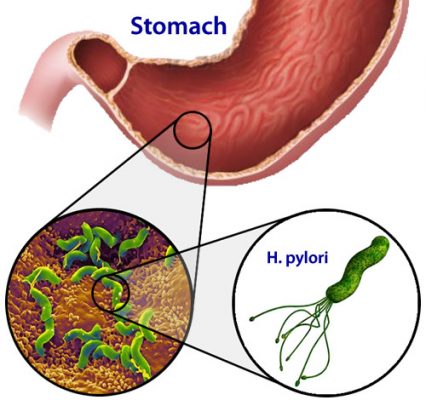 Proton pump inhibitors (PPIs), a type of medication used to reduce gastric acid, have been linked to gastric cancer in a new study by Ka Shing Cheung and colleagues. A 2017 article in Gut, the journal of the British Society of Gastroenterology, reports that receiving PPIs to treat stomach infections from the bacterium Helicobacter pylori increases the risk of later gastric cancer.
Proton pump inhibitors (PPIs), a type of medication used to reduce gastric acid, have been linked to gastric cancer in a new study by Ka Shing Cheung and colleagues. A 2017 article in Gut, the journal of the British Society of Gastroenterology, reports that receiving PPIs to treat stomach infections from the bacterium Helicobacter pylori increases the risk of later gastric cancer.
The study relied on a territory-wide health database in Hong Kong. Out of 63,397 subjects, 153 developed gastric cancer after being treated for Helicobacter pylori. PPI treatment was associated with a 2.4-fold increase in risk of gastric cancer, while treatment with histamine-2 receptor agonist drugs did not increase cancer risk.
Editor’s Note: PPIs are widely used in psychiatric patients. Care should be taken with their long-term use.
An Inflammatory State Impedes Treatment for Bipolar Disorder
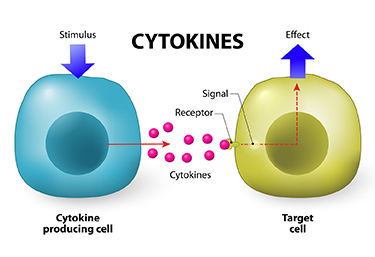 A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
Researcher Francesco Benedetti and colleagues report that high levels of inflammatory cytokines (a type of small proteins) predicted a worse response to treatment with sleep deprivation and light therapy for bipolar depression. This treatment typically brings about a rapid antidepressant response.
Benedetti and colleagues measured 15 immune-regulating compounds in 37 patients who were experiencing an episode of bipolar depression and 24 healthy volunteers. Among those participants with bipolar disorder, 84% had a history of non-response to medication. Twenty-three of the 37 patients, or 62%, responded to the sleep deprivation/light therapy combination. Those who did not had higher levels of five cytokines: interleukin-8, monocyte chemoattractant protein-1, interferon-gamma, interleukin-6, and tumor necrosis factor-alpha.
Body mass index was correlated with cytokine levels and also reduced response to the treatment.
The finding supports a link between the immune system and mood disorders. Evaluating a patient’s level of inflammation may, in the future, allow doctors to predict the patient’s response to a given therapy. Patients with high levels of inflammation might benefit most from treatments that target their immune system.
FDA Approves New Higher Dose of Valbenazine for Tardive Dyskinesia
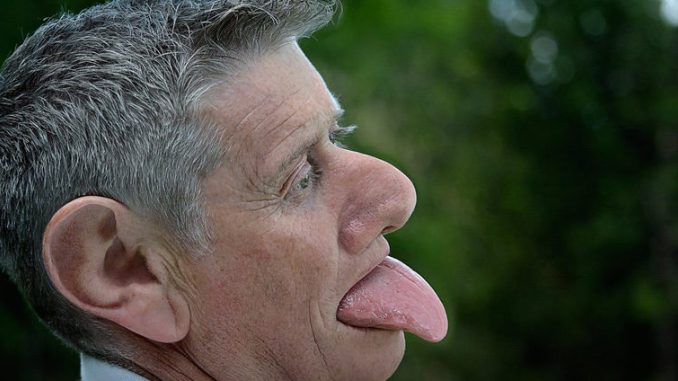
The US Food and Drug Administration has approved an 80 mg capsule dose of valbenazine (Ingrezza) for tardive dyskinesia (jerky, involuntary movements of the face, especially the mouth and tongue, fingers and body that can be a side effect of antipsychotic medication). Valbenazine, a selective vesicular monoamine transporter 2 inhibitor, was the first drug FDA-approved for tardive dyskinesia. The FDA initially approved a dosage of 40 mg/day in April 2017. The 80 mg/day dose was approved in October 2017.
The new approval was based on a 6-week clinical trial in which 80 mg of valbenazine improved tardive dyskinesia significantly compared to placebo. Improvement continued over 48 weeks of treatment.
Taking SSRI Antidepressants May Increase Stroke Risk
 A Taiwanese study published in the Journal of Clinical Psychiatry in 2017 finds that taking selective serotonin reuptake inhibitor (SSRI) antidepressants can increase risk of stroke. The study by Chin-Hong Chan and colleagues analyzed eight years of data from Taiwan’s National Health Insurance Research Database, comparing people who had taken SSRIs for at least two consecutive months to those who had not. First onset strokes were more common among people who had taken SSRIs, and the higher stroke rates in this group persisted for three years after exposure.
A Taiwanese study published in the Journal of Clinical Psychiatry in 2017 finds that taking selective serotonin reuptake inhibitor (SSRI) antidepressants can increase risk of stroke. The study by Chin-Hong Chan and colleagues analyzed eight years of data from Taiwan’s National Health Insurance Research Database, comparing people who had taken SSRIs for at least two consecutive months to those who had not. First onset strokes were more common among people who had taken SSRIs, and the higher stroke rates in this group persisted for three years after exposure.
Ischemic strokes (which occur when a blood vessel carrying blood to the brain is obstructed) were more common than hemorrhagic strokes (which occur when a weak blood vessel ruptures). Younger adult participants exposed to SSRIs were more likely to have strokes, while people older than 65 saw only a slight increase in stroke risk from taking SSRIs. More strokes occurred during the first three years of SSRI treatment than later in treatment.
Chan and colleagues suggest that these strokes are caused by cerebral microbleeding or by overcorrection of hemostasis, the process by which the body slows or stops bleeding by constricting blood vessels and coagulating blood.
Best Antidepressants for Post-Stroke Depression
 A recent meta-analysis in the journal BMJ Open analyzes the efficacy and tolerability of 10 different antidepressants given to treat depression following a stroke. The meta-analysis incorporated data from 12 trials and a total of 707 participants. Reboxetine was the most effective antidepressant, followed by paroxetine, doxepin, and duloxetine. Sertraline, fluoxetine, and nefiracetam failed to outperform placebo in the treatment of post-stroke depression.
A recent meta-analysis in the journal BMJ Open analyzes the efficacy and tolerability of 10 different antidepressants given to treat depression following a stroke. The meta-analysis incorporated data from 12 trials and a total of 707 participants. Reboxetine was the most effective antidepressant, followed by paroxetine, doxepin, and duloxetine. Sertraline, fluoxetine, and nefiracetam failed to outperform placebo in the treatment of post-stroke depression.
In terms of tolerability, paroxetine had the least side effects and led to significantly fewer discontinuations than doxepin, citalopram, and fluoxetine. After paroxetine, the most tolerable drugs were sertraline and nortriptyline. The least tolerable drug was citalopram.
Researchers led by Yefei Sun suggested that paroxetine might be the best antidepressant to prescribe after a stroke due to its efficacy and good tolerability. Fluoxetine might be the worst due to its poor efficacy and poor side effects profile.
Editor’s Note: Multiple randomized controlled trials suggest that antidepressants can be helpful for anyone who has a stroke, both to decrease depression and to improve neurological and functional outcomes.
Vagus Nerve Stimulation Improves Depression When Other Treatments Fail
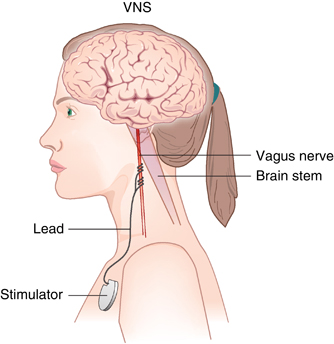 Vagus nerve stimulation (VNS) has been approved by the US Food and Drug Administration as an adjunctive therapy for treatment-resistant unipolar and bipolar depression since 2005. The treatment consists of a pacemaker-like device implanted under the skin in the chest that delivers regular, mild electrical pulses to the brain via the left vagus nerve.
Vagus nerve stimulation (VNS) has been approved by the US Food and Drug Administration as an adjunctive therapy for treatment-resistant unipolar and bipolar depression since 2005. The treatment consists of a pacemaker-like device implanted under the skin in the chest that delivers regular, mild electrical pulses to the brain via the left vagus nerve.
A 2017 study by Scott T. Aaronson and colleagues in the American Journal of Psychiatry reports that over a 5-year period, people with treatment-resistant depression who received VNS did better than those who received treatment as usual. The 795 participants at 61 US sites had either a depressive episode that had lasted for at least two years or had had three or more depressive episodes and had failed to respond to at least four treatments, including electroconvulsive therapy (ECT). Over five years, those who received VNS had higher response rates (67.6% versus 40.9%) and higher remission rates (43.3% versus 25.7%) compared to those who received treatment as usual.
While the study by Aaronson and colleagues was non-blind and non-randomized, it suggests that VNS could be helpful in the long-term management of treatment-resistant unipolar and bipolar depression.
Editor’s Note: VNS was FDA-approved for treatment-resistant seizures in patients aged 12 and older in 1997 and for children 4 years and older in 2017. It was also approved for cluster headaches in 2017. Insurance coverage and reimbursement for VNS is typically available for these neurological conditions, but not for the treatment of depression. This is an unfortunate example of the stigmatization of psychiatric illness—when an FDA-approved device can be kept from people in need of treatment.
One Night of Sleep Deprivation Can Rapidly Improve Depression
 One night of sleep deprivation can bring about rapid improvement in depression symptoms the following day. A 2017 meta-analysis by Elaine M. Boland and colleagues in the Journal of Clinical Psychiatry summarizes the findings from 66 studies of sleep deprivation for unipolar and bipolar depression and finds that the technique produced a response rate of 45% in randomized controlled studies.
One night of sleep deprivation can bring about rapid improvement in depression symptoms the following day. A 2017 meta-analysis by Elaine M. Boland and colleagues in the Journal of Clinical Psychiatry summarizes the findings from 66 studies of sleep deprivation for unipolar and bipolar depression and finds that the technique produced a response rate of 45% in randomized controlled studies.
It did not seem to matter whether patients experienced full or partial sleep deprivation, whether they had unipolar or bipolar depression, or whether or not they were taking medication at the time. Age and gender also did not affect the results of the sleep deprivation.
Extending the Effects
While sleep deprivation can rapidly improve depression, the patient often relapses after the next full night of sleep. There are a few things that can prevent relapse or extend the efficacy of the sleep deprivation. The first is lithium, which has extended the antidepressant effects of sleep deprivation in people with bipolar disorder.
The second strategy to prevent relapse is a phase change. This means going to sleep early in the evening the day after sleep deprivation and gradually shifting the sleep schedule back to normal. For example, after an effective night of sleep deprivation, one might go to sleep at 6pm and set their alarm for 2am. Then the next night, they would aim to sleep from 7pm to 3am, the following night 8pm to 4am, etc. until the sleep wake cycle returns to a normal schedule.
A 2002 article by P. Eichhammer and colleagues in the journal Life Sciences suggested that repetitive transcranial magnetic stimulation (rTMS), electromagnetic stimulation of the scalp over the prefrontal cortex, could help maintain improvement in depression following a night of partial sleep deprivation for up to four days.
Bright light therapy may also help. Read more
Inflammation Predicts Poor Response to Sleep Deprivation with Light Therapy
A 2017 article by Francesco Benedetti and colleagues in the Journal of Clinical Psychiatry reports that people with bipolar depression who have higher levels of certain inflammatory markers may have a poor antidepressant response to the combination of sleep deprivation and light therapy, compared to those with lower levels of inflammation.
The study included 37 participants with bipolar disorder who were in the midst of a major depressive episode. Of those, 31 participants (84%) had a history of poor response to antidepressant medication. The patients were treated with three cycles of total sleep deprivation and light therapy within one week, a combination that can often bring about a rapid improvement in depression.
Depression improved in a total of 23 patients (62%) following the therapy. Blood analysis showed that compared to those who had a good response, the non-responders had higher levels of five intercorrelated inflammatory markers: IL-8, MCP-1, IFN-gamma, IL-6, and TNF-alpha. Those with higher body mass index had more inflammation, indirectly decreasing response to the therapy.