Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
Treatment Plans for Maladaptive Impulsive Aggression in Children
Maladaptive impulsive aggression often co-occurs with other psychiatric illnesses in children, so it can be difficult to find treatment solutions. A symposium at the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry yielded some suggestions. Read on for an overview of impulsive aggression and possible treatment plans.
At the symposium, held in New York Oct. 26-31, 2010, panelists called maladaptive aggression the “fever” of child psychiatry (because it is common but also nonspecific) and described the phenomenon as “the language of the inarticulate.” The panelists drew a distinction between impulsive aggression, which describes behavior that is unplanned, unprofitable, and poorly controlled, and another phenomenon, predatory aggression, which describes behavior that is planned, sometimes profitable, and highly controlled.
The speakers on the panel indicated that impulsive aggression is related to other psychiatric syndromes including depression, attention deficit hyperactivity disorder (ADHD), mania, conduct disorder, oppositional defiant disorder, anxiety, post-traumatic stress disorder (PTSD), borderline personality disorder, autism, and schizophrenia. This raises problems for drug development, as Tom Laughren of the Federal Drug Administration (FDA) indicated in one talk at the symposium, because when new treatments are developed, they are studied in the context of only one primary disorder. Read more
Atypical Antipsychotics with the Lowest Risk of Weight Gain
 There is a major problem of overweight and obesity in the US, with about 50% of the population affected. Patients with mood disorders, and particularly bipolar disorder, appear to be at increased risk for weight gain, which often accompanies depression. Thus, it is important that when treating these patients, doctors prescribe medications with low likelihood of weight gain.
There is a major problem of overweight and obesity in the US, with about 50% of the population affected. Patients with mood disorders, and particularly bipolar disorder, appear to be at increased risk for weight gain, which often accompanies depression. Thus, it is important that when treating these patients, doctors prescribe medications with low likelihood of weight gain.
Among the atypical antipsychotics that are widely used not only in schizophrenia but also in bipolar disorder and sometimes as adjunctive treatments in unipolar depression, there are wide differences in potential for weight gain and alterations in metabolic indices such as cholesterol, triglycerides, and blood glucose. Clozapine and olanzapine convey the greatest risk for abnormalities in these indices; risperidone and quetiapine convey moderate risk, and aripiprazole and ziprasidone are the least likely to affect metabolic indices. Newly approved lurasidone also has a mild side-effects profile.
The atypical ziprasidone (Geodon) appears to be truly weight-neutral and to have minimal impact on metabolic indices, but is not widely used due to two potential complications, neither of which must necessarily cause problems. One is the difficulty of dose titration with this drug. Surprisingly, low doses of the drug may be somewhat activating. (Atypicals are usually sedating.) Studies suggest that starting treatment with higher doses or increasing doses more quickly may be better tolerated. So rather than starting at 20mg twice a day, 40mg twice a day with rapid increases towards the range of 80mg twice a day may be associated with better tolerability. Read more
Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
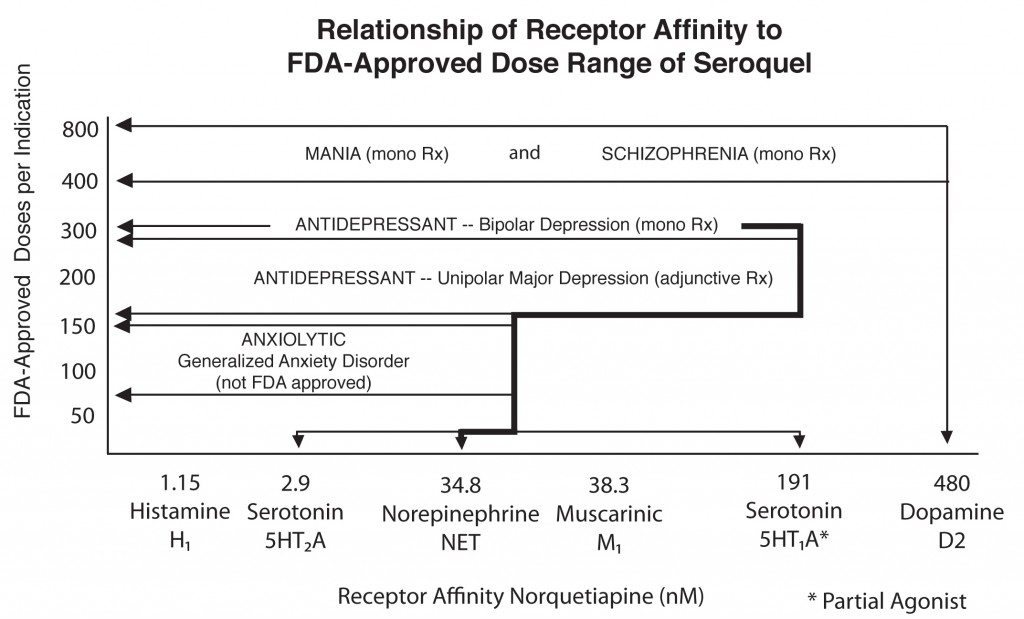
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Read more
Reconsidering Ziprasidone (Geodon) for Kids with Bipolar Disorder
Ziprasidone has shown efficacy in pediatric BP I disorder (ages 10 to 17). Its metabolic profile is the most benign of the atypical antipsychotics, including being the only one that does not produce weight gain in children. None of the other metabolic indices increased either.
This drug is currently rarely used in children because of concerns about its effects on electrocardiogram (EKG), which have rarely been seen in clinical practice. Perhaps the overall assessment of its risk/benefit ratio should be re-evaluated.
We’ve posted before about ziprasidone’s benign side effects profile.


