Ambien Linked to Emergency Room Visits, Among Other Risks
Zolpidem, better known by one of its trade names, Ambien, is widely prescribed for the short-term treatment of insomnia. It can sometimes cause adverse reactions, particularly among women and the elderly. The Substance Abuse and Mental Health Services Administration (SAMHSA) has reported that over a recent 5-year period, emergency department visits for adverse reactions to zolpidem increased by almost 220%.
Peter Delaney, Director of SAMSHA’s Center for Behavioral Health Statistics and Quality, suggested that doctors should consider alternative strategies for treating insomnia, including improving sleep hygiene by avoiding caffeine, exercising regularly, and sleeping in a quiet, dark room. He also suggested that doctors should be aware of what other medications a patient is taking, and ideally all of a patient’s prescriptions should be collected from the same pharmacy, so the pharmacist can act as a second pair of eyes identifying possible drug interactions.
Women and men metabolize zolpidem differently, and according to Sam Fleishman of the American Academy of Sleep Medicine, many women can still be impaired by the drug 8 hours after taking it. In 2013, after reports of adverse reactions to zolpidem increased, the Federal Drug Administration (FDA) required manufacturers of drugs containing zolpidem to reduce the recommended dose for women by half, from 10 mg to 5 mg, or 12.5 mg to 6.25 mg for the extended-release version. The FDA also suggested halving the dosage prescribed to the elderly, and reducing the recommended dose for men.
Some of the adverse reactions to drugs containing zolpidem include daytime drowsiness, dizziness, hallucinations, sleepwalking, and even “sleep driving.” When combined with antianxiety medications, narcotic pain relievers, or alcohol, zolpidem’s sedative effects can be enhanced to dangerous levels.
Proven Treatments for Fibromyalgia and Chronic Fatigue Syndrome
At the 2012 meeting of the Collegium Internationale Neuro-Psychopharmacologicum (CINP), a symposium was held to discuss fibromyalgia and chronic fatigue syndrome, two illnesses that remain mysterious.
Fibromyalgia
Fibromyalgia is more common in women than in men and is characterized by aching all over, decreased sleep, stiffness upon waking, and most prominently, being tired all day, as well as a host of other symptoms including headache, dizziness, and gastrointestinal upset. Researcher Siegried Kasper suggested that treating fibromyalgia requires more than just medication. His approach is known as MESS, which stands for medication, exercise, sleep management, and stress management.
Medications to treat the illness include milnacipran (not available in the US), duloxetine (Cymbalta, a serotonin-norepinephrine reuptake inhibitor or SNRI), or pregabalin (Lyrica), and if tolerated, low doses of the tricyclic amitriptyline (Elavil).
According to Kasper, SSRIs and anti-inflammatory drugs don’t work, and benzodiazepines decrease the deepest phase of sleep (stage 4) and can exacerbate the syndrome.
Recommended exercise is moderate, graded (to a pulse of about 120, or at a level where the patient can still talk, but can’t sing), and should be done in the early morning rather than the late afternoon where it might interfere with sleep.
Good sleep hygiene is recommended, such as keeping the same sleep schedule every day and abstaining from caffeine (even in the morning).
Working on developing active coping strategies for stressors that are likely to occur is a good idea. Mindfulness and other meditative techniques may also be helpful. Joining a support group (that encourages exercise rather than discouraging it) was also recommended.
Chronic Fatigue Syndrome
At the CINP meeting researcher Simon Wessely discussed chronic fatigue syndrome (CFS), which has many overlaps with fibromyalgia. He reported that careful controlled study of more than 15,000 individuals has not indicated that the illness is associated with a viral infection. Just as many people with and without chronic fatigue syndrome were found to be infected with a virus.
However, like the myth that vaccines cause autism, the myth that chronic fatigue is associated with a virus remains popular despite the lack of evidence. A large randomized study validated Wessely’s treatment techniques, but he has continued to be vilified for the position that the illness is not virally based. The study showed that patients who participated in cognitive behavior therapy and graded exercise improved more than those who received conventional medical management.
Wessely thought the most important cognitive change to make was accepting that exercise is not harmful for patients with chronic fatigue syndrome, and is in fact helpful and therapeutic. Many older treatment approaches had advocated rest, rest, and more rest, or even “intensive rest.” However, Wessely indicated that this would be counter-productive, as the patient would lose muscle mass and cardiovascular conditioning, and would become even more tired and chronically fatigued.
Activity Monitoring Discriminates Between BP Kids and ADHD Kids
At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Gianni Faedda of the Lucio Bini Mood Disorders Center reported that monitoring of activity, sleep, and circadian-rhythm disturbances can be used to distinguish children with a diagnosis of bipolar illness (who showed more hyperactivity and less sleep), from children with ADHD and control children without illness.
Track Your Moods with Life Charting
If you have unipolar depression or bipolar disorder and are having trouble stabilizing your mood, we recommend nightly charting of mood, medications and side effects on the easy-to-use Monthly Mood Chart Personal Calendar (pictured below) or the National Institute of Mental Health Life Chart (NIMH-LCM), both of which are available for download.
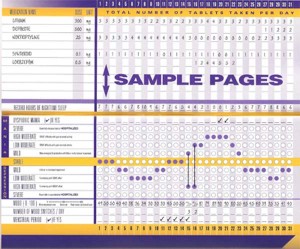
Sample Mood Chart
Click on the Life Charts tab above to download the personal calendar, which includes space for rating mood, functioning, hours of sleep, life events, side effects, and other symptoms such as anxiety. Then bring the chart to each visit with your physician to help in the assessment of treatments.
Life charting can help determine which medications are working partially and need to be augmented further, and which need to be eliminated because of side effects. Since there are now many potential treatments for depression and bipolar disorder (some FDA-approved and some not), a careful assessment of how well each new treatment works for a particular patient is essential to finding the optimal treatment regimen.
Treating Generalized Anxiety Disorder
Generalized anxiety disorder (GAD) is a prevalent illness often associated with considerable discomfort and dysfunction. It often co-occurs with bipolar disorder. Traditional treatments of the primary syndrome (occurring in the absence of bipolar disorder) involve serotonin-selective antidepressants and serotonin-noradrenergic reuptake inhibitors such as venlafaxine (Effexor) or duloxitine (Cymbalta). While these are often useful and lead to considerable improvement, they often do not lead to full remission of somatic or accompanying symptoms of insomnia.
Alternative treatment possibilities include the anticonvulsant pregabalin (Lyrica), which has been found effective in four placebo-controlled studies in GAD. A poster presentation by Joshi et al. at the American Psychiatric Association meeting in San Francisco in May 2009 also reported that pregabalin was more effective in reducing sleep disturbance than venlafaxine. Pregabaline is FDA-approved for seizures and fibromyalgia, but not for GAD or pain syndromes. Another treatment possibility is quetiapine (Seroquel), where not only have there been positive efficacy in placebo-controlled studies of patients with GAD, but the patients also experienced improvement in sleep.
Read more




