The Gold Standard in Bipolar Disorder Treatment
Last year our Editor-in-Chief Robert M. Post participated in a symposium at the annual meeting of the American Psychiatric Association on the best treatments for bipolar disorder. An article in Psychology Today describes some of the conclusions of the expert panel.
Treatment Approaches to Childhood-Onset Treatment-Resistant Bipolar Disorder
Dear readers interested in the treatment of young children with bipolar disorder and multiple other symptoms: In 2017, BNN Editor Robert M. Post and colleagues published an open access paper in the journal The Primary Care Companion for CNS Disorders titled “A Multi-Symptomatic Child: How to Track and Sequence Treatment.” The article describes a single case of childhood-onset bipolar disorder shared with us via our Child Network, a research program in which parents can create weekly ratings of their children’s mood and behavioral symptoms, and share the long-term results in graphic form with their children’s physicians.
Here we summarize potential treatment approaches for this child, which may be of use to other children with similar symptoms.
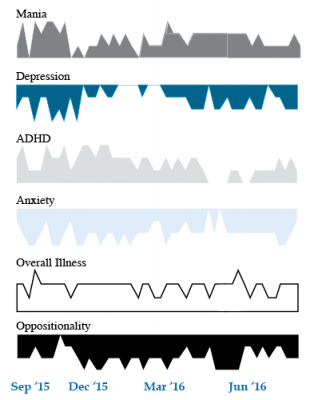
We present a 9-year-old girl whose symptoms of depression, anxiety, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania were rated on a weekly basis in the Child Network under a protocol approved by the Johns Hopkins School of Medicine Institutional Review Board. The girl, whose symptoms were rated consistently for almost one year, remained inadequately responsive to lithium, risperidone, and several other medications. We describe a range of other treatment options that could be introduced. The references for the suggestions are available in the full manuscript cited above, and many quotes from the original article are reprinted here directly.
As illustrated in the figure below, after many weeks of severe mania, depression, and ADHD, the child initially appeared to improve with the introduction of 4,800 micrograms per day of lithium orotate (a more potent alternative to lithium carbonate that is marketed as a dietary supplement), in combination with 1 mg per day of guanfacine, and 1 mg per day of melatonin.
Despite continued treatment with lithium orotate (up to 9,800 micrograms twice per day), the patient’s oppositional behavior worsened during the period from November 2015 to March 2016, and moderate depression re-emerged in April 2016. Anxiety was also generally less severe from December 2015 to July 2016, and weekly ratings of overall illness remained in the moderate severity range (not illustrated).
In June 2016, the patient began taking risperidone (maximum dose 1.7 mg/day) instead of lithium, and her mania improved from moderate to mild. There was little change in her moderate but fluctuating depression ratings, but her ADHD symptoms got worse.
The patient had been previously diagnosed with bipolar II disorder and anxiety disorders including school phobia, generalized anxiety disorder, and obsessive compulsive disorder.
Given the six weeks of moderate to severe mania that the patient experienced in October and November 2015, she would meet criteria for a diagnosis of bipolar I disorder.
Targeting Symptoms to Achieve Remission
General treatment goals would include: mood stabilization prior to use of ADHD medications, a drug regimen that maximizes tolerability and safety, targeting of residual symptoms with appropriate medications supplemented with nutraceuticals, recognition that complex combination treatment may be necessary, and combined use of medications, family education, and therapy.
Mood Stabilizers and Atypical Antipsychotics to Maximize Antimanic Effects
None of the treatment options in this section are approved by the US Food and Drug Administration for use in children under 10 years of age, so all of the suggestions are “off label.” Further, they may differ from what other investigators in this area of medicine would suggest, especially since evidence-based medicine’s traditional gold standard of randomized placebo-controlled clinical trials is impossible to apply here, given the lack of research in children with bipolar disorder.
As we share in the original article, reintroducing lithium alongside risperidone could be effective, as “combinations were more effective than monotherapy in a study [by] Geller et al. (2012), especially when they involved an atypical antipsychotic such as risperidone. This might include the switch from lithium orotate to lithium carbonate,” the typical treatment for bipolar disorder, on which more research has been done. “Combinations of lithium and valproate were also more effective than either [drug alone]…in the studies of Findling et al. (2006),” and many patients needed stimulants in addition.
“Most children also needed combinations of mood stabilizers (lithium, carbamazepine, valproate) in the study [by] Kowatch et al. (2000).” In a 2017 study by Berk et al. of patients hospitalized for a first mania, randomization to lithium for one year was more effective than quetiapine on almost all outcome measures.
Targeting ADHD
“[The increased] severity of [the child’s] ADHD despite improving mania speaks to the…utility of adding a stimulant to the regimen that already includes…guanfacine,” which is a common non-stimulant treatment for ADHD. “This would be supported by the data of Scheffer et al. (2005) that stimulant augmentation for residual ADHD symptoms does not [worsen] mania, and that the combination of a stimulant and guanfacine may have more favorable effects than stimulants alone.”
However, the consensus in the field is that mood stabilization should be achieved first, before low to moderate (but not high) doses of stimulants are added. “Thus, in the face of an inadequate response to the lithium-risperidone combination in this child, stimulants could be deferred until better mood stabilization was achieved.”
Other Approaches to Mood Stabilization and Anxiety Reduction
“The anticonvulsant mood stabilizers (carbamazepine, lamotrigine, and valproate) each have considerable mood stabilizing and anti-anxiety effects, at least in adults with bipolar disorder. With inadequate mood stabilization of this patient on lithium and risperidone, we would consider the further addition of lamotrigine.
Lamotrigine appears particularly effective in adults with bipolar disorder who have a personal history and a family history of anxiety (as opposed to mood disorders), and it has positive open data in adolescents with bipolar depression and in a controlled study of maintenance (in teenagers 13–17, but not in preteens 10–12) (Findling et al. 2015). With better mood stabilization, anxiety symptoms usually diminish…, and we would pursue these strategies [instead of using] antidepressants for depression and anxiety in young children with bipolar disorder.”
“Carbamazepine appears to be more effective in adults with bipolar who have [no] family history of mood disorders,” unlike lithium, which seems to work better in people who do have a family history of mood disorders.
“While the overall results of oxcarbazepine in childhood mania were negative, they did exceed placebo in the youngest patients (aged 7–12) as opposed to the older adolescents (13–18) (Wagner et al. 2006).
“There are long-acting preparations of both carbamazepine (Equetro) and oxcarbazepine (Oxtellar) that would allow for all nighttime dosing to help with sleep and reduce daytime side effects and sedation. Although data [on] anti-manic and antidepressant effects in adults are stronger for carbamazepine than oxcarbazepine,” there are good reasons to consider oxcarbazepine. First, there is the finding mentioned above that oxcarbazepine worked best in the youngest children. Second, there is a lower incidence of severe white count suppression on oxcarbazepine. Third, it has less of an effect on liver enzymes than carbamazepine. However, low blood sodium levels are more frequent on oxcarbazepine than carbamazepine.
Other Atypical Antipsychotics That May Improve Depression
Playing Tackle Football Before Age 12 May Be Bad for the Brain
A 2017 study found that men who began playing American tackle football before age 12 were more likely to have depression, apathy, problems with executive functioning, and behavioral issues in adulthood than their peers who began playing football after age 12. Duration of football play did not seem to matter—those men who stopped playing football after high school were just as likely to be affected in adulthood as those who went on to play football in college or professionally.
The study by Michael L. Alosco and colleagues was published in the journal Translational Psychiatry. It included 214 men (average age 51) who had played football in their youth, but not other contact sports. The men reported their own experiences with depression, apathy, cognitive function, and behavioral regulation. Those who began football before age 12 were twice as likely to report impairment in behavioral regulation, apathy, and executive function than those who began playing later. Those who started younger were also three times more likely to have clinical depression in adulthood than those who started older.
According to Alosco and colleagues, between ages 9 and 12, the brain reaches peak maturation of gray and white matter volume, and synapse and neurotransmitter density also increases. The repeated head injuries that can occur during youth football play during this time may disrupt neurodevelopment, with lasting negative effects.
One drawback to the study was that recruitment was not random—men who volunteered for the study might have done so due to a recognition of their own cognitive problems. However, the results suggest more study is needed, and caution is encouraged when making decisions about youth football participation. Some youth football leagues have begun placing greater limits on the type of contact allowed during play.
Children Who Are Bullied Have Poorer Mental Health
A 2017 study of twins between the ages of 11 and 16 found that being bullied around age 11 caused anxiety, depression, hyperactivity and impulsivity, inattention, and conduct problems, some of which lasted for years. Participants recorded their experiences with physical or verbal bullying, social manipulation, and property attacks (trying to break one’s belongings, for example).
The effects of bullying decreased over time. The bullied children were still significantly more anxious than their non-bullied twins two years later, but this difference faded by the five-year mark. However, paranoid thoughts and cognitive disorganization did persist for 5 years.
The twin study design helped researchers zone in on the causal effect bullying might have on the children’s mental health, rather than other factors the twins shared, such as genetics or family environment. The study included 11,108 twins born in England and Wales.
The research by Timothy Singham and colleagues was published in the journal JAMA Psychiatry. Interestingly, the researchers found that prior mental health difficulties increased children’s likelihood of being bullied, such that being bullied could be considered a symptom of preexisting vulnerabilities. Singham and colleagues suggest that in addition to interventions to reduce bullying and address familial factors that might make children susceptible to bullying, children should also be taught resilience skills.
Cannabinoid Gel Treats Fragile X Syndrome
Fragile X syndrome is a genetic disorder characterized by developmental problems such as intellectual disabilities, cognitive impairment, and behavioral and learning challenges. Zynerba Pharmaceuticals announced in 2017 that a cannabinoid gel they have produced improved symptoms of fragile x syndrome in children and adolescents when applied daily to the upper arm.
Multiple cannabinoids are derived from cannabis plants, and include cannabidiol, which likely conveys some of the plant’s positive effects, and tetrahydrocannabinol (THC), which lends marijuana its psychoactive or psychomimetic effects, such as delusion or delirium. Cannabidiol is the active ingredient in the gel, and no THC was found in participants’ blood tests after using the gel.
The open study of 20 patients aged 6 to 17 years found that the participants showed improvement on a scale measuring anxiety, depression, and mood after 12 weeks of using the gel. The gel also appeared to improve aberrant behaviors including social avoidance, temper tantrums, repetitive movements, and hyperactivity. Treatment began at a dose of 50mg per day, and could be increased up to 250 mg per day within the first six weeks of the study. The dose then remained stable for the next six weeks.
Zynerba Pharmaceuticals hope to begin controlled clinical trials in 2018, with the goal of attaining approval for the drug from the US Food and Drug Administration. Other companies are also competing to garner the first FDA approval of a cannabis-based drug. Many of the drugs currently in development are intended to target neurological or behavioral conditions.
Pediatric Bipolar Disorder Diagnoses Much More Common in US than England
 A 2014 article by Anthony James and colleagues in the Journal of the American Academy of Child and Adolescent Psychiatry reported that hospitalizations for pediatric bipolar disorder are 72.1 times higher in the US than in England.
A 2014 article by Anthony James and colleagues in the Journal of the American Academy of Child and Adolescent Psychiatry reported that hospitalizations for pediatric bipolar disorder are 72.1 times higher in the US than in England.
The researchers determined that there were 100.9 diagnoses of pediatric bipolar disorder per 100,000 people in the US, but only 1.4 cases per 100,000 people in Britain. The discrepancy in diagnoses for adult bipolar disorder and for other childhood psychiatry illnesses were smaller but still notable: While 158.2 adults per 100,000 in the US were diagnosed with bipolar disorder, only 22.1 adults per 100,000 in England received such a diagnosis, making the diagnosis of bipolar disorder in adults 7.2 times more common in the US. Diagnoses of childhood attention-deficit hyperactivity disorder (ADHD) were 13.0 times more common in the US than in England, while cases of childhood depression were 4.2 times more common in the US.
James and colleagues hypothesized several potential reasons for the dramatic difference in diagnosis rates at hospital discharge of bipolar disorder in children in the US versus England. The lower hospitalization rates for pediatric bipolar disorder in England may reflect the better availability of community or outpatient treatment options there. Diagnostic practices may also differ. James and colleagues suggested that in the US, pediatric diagnoses of bipolar disorder are often used to describe children and adolescents with irritability and frequent mood shifts, whereas English diagnostic practices rely more on episodic bouts of euphoria to diagnose bipolar disorder in children.
However, children in the US may simply be more likely to have a variety of childhood psychiatric disorders than those from England.
Editor’s Note: Epidemiological data support the view that bipolar disorder not otherwise specified (BP-NOS), which is often the earliest manifestation of bipolar disorder, is indeed much more common in the US than multiple other countries.
Even if there are some diagnostic differences that contribute to the immense 72.1 fold higher rates of hospitalization for childhood bipolar in the US compared to Britain, one cannot overlook the findings that these children are requiring hospitalization for something resembling bipolar disorder and are in need of treatment. Read more
FDA Approves Lurasidone for Bipolar Depression in Children and Adolescents
 In March 2018, the US Food and Drug Administration approved the antipsychotic drug lurasidone (Latuda) for the treatment of bipolar depression in children and adolescents aged 10–17 years. Lurasidone was already approved for adults with bipolar depression, as an add-on treatment to the mood stabilizers lithium and valproate, and for schizophrenia in people aged 13 years and up.
In March 2018, the US Food and Drug Administration approved the antipsychotic drug lurasidone (Latuda) for the treatment of bipolar depression in children and adolescents aged 10–17 years. Lurasidone was already approved for adults with bipolar depression, as an add-on treatment to the mood stabilizers lithium and valproate, and for schizophrenia in people aged 13 years and up.
A 6-week clinical trial in 347 youth compared lurasidone (in doses ranging from 20 to 80 mg/day) to placebo and found that those who received lurasidone showed significant improvements in depression compared to those who received placebo. The average dose was below 40 mg/day. The research by Melissa P. DelBello and colleagues was published in the Journal of the American Academy of Child and Adolescent Psychiatry in 2017.
In the study, lurasidone was well-tolerated. Side effects included nausea, sleepiness, minimal weight gain, and insomnia. Lurasidone did not seem to affect glucose, triglycerides, cholesterol, or blood pressure.
Editor’s Note: This is the first drug to be approved for bipolar depression in this age range. This editor (Robert M. Post) has written extensively on the high incidence of childhood onset bipolar disorder in the US, and especially in the offspring of parents with bipolar disorder.
It is important to be alert to the possibilities of depression and bipolar disorder in children in the US (along with related illnesses such as anxiety, oppositional defiant disorder, and attention deficit hyperactivity disorder (ADHD)), as early-onset illness tends to have a more severe long-term course than adult-onset depression and bipolar disorder. A longer delay between the emergence of symptoms and the first treatment for bipolar disorder is also a risk factor for more severe depression, more time depressed, and a poorer outcome in adulthood.
Parents of children aged 2-12 who have mood or behavioral problems are encouraged to consider joining the Child Network at our website, bipolarnews.org (click on the tab for the Child Network). By participating in this research network, parents are able to make a weekly rating of the severity of their children’s symptoms of anxiety, depression, ADHD, oppositional behavior, and mania via the secure website. The ratings can then be shared with the child’s clinicians for easy visualization of the course of symptoms over time, which may help with treatment decisions.
Clinical Vignettes from Dr. Elizabeth Stuller
 Dr. Elizabeth Stuller, a staff psychiatrist at the Amen clinics in Washington, DC and CEO of private practice Stuller Resettings in Baltimore, MD, provided this editor (Robert M. Post) with several interesting anecdotal observations based on her wide clinical experience with difficult-to-treat mood disordered patients.
Dr. Elizabeth Stuller, a staff psychiatrist at the Amen clinics in Washington, DC and CEO of private practice Stuller Resettings in Baltimore, MD, provided this editor (Robert M. Post) with several interesting anecdotal observations based on her wide clinical experience with difficult-to-treat mood disordered patients.
- Stuller has used low-dose asenapine (Saphris), e.g. half a pill placed under the tongue, for depressed patients with alcohol use problems who have trouble getting to sleep. She has also used asenapine for rapid calming of agitated patients in her office.
- Stuller has also had success with the use of the atypical antipsychotic drug brexpiprazole (Rexulti) for patients with bipolar depression and low energy. She typically uses 0.5 mg/day for women and 1 mg/day for men. Stuller finds that there is little weight gain or akathisia with brexpiprazole.
- She has had success with the drug Nuedexta, which is a combination of dextromethorphan and quinidine and is approved for the treatment of sudden uncontrollable bouts of laughing or crying, known as pseudobulbar affect, which can occur as a result of neurological conditions or brain injuries. It is a combination of an NMDA antagonist and a sigma receptor agonist. Stuller starts with the 20mg dextromethorphan/10 mg quinidine dose once a day and increases to twice a day in week two. She finds it useful for behavioral effects of traumatic brain injury (TBI), anxiety resulting from the use of synthetic marijuana (sometimes called spice), and psychosis not otherwise specified. Stuller also finds that some patients appear to respond well to Nuedextra but not minocycline, or vice versa.
Editor’s Note: Note that these are preliminary clinical anecdotes conveyed in a personal communication, and have not been studied in clinical trials, thus should not be relied upon in the making of medical decisions. All decisions about treatment are the responsibility of a treating physician.
Nutritional Supplement ALC Improves Depression
A meta-analysis of 12 studies suggests that the nutrient acetyl-l-carnitine (ALC), when taken as a nutritional supplement, has antidepressant effects. The meta-analysis by researcher Nicola Veronese and colleagues appeared in the journal Psychosomatic Medicine in 2017. Veronese and colleagues found that in nine randomized controlled trials, ALC reduced depressive symptoms significantly compared to placebo. In three randomized controlled trials that compared ALC with established antidepressants, ALC showed similar effectiveness at reducing depressive symptoms while producing 79% fewer side effects. Doses of ALC ranged from 1 to 4 grams per day, and higher doses led to greater improvement.
In the comparisons with antidepressants, the other treatments included fluoxetine (Prozac), duloxetine (Cymbalta), and amisulpride (which is not approved by the US Food and Drug Administration).
Low ALC has been linked to depression. According to Veronese and colleagues, ALC deficiency can dysregulate the transport of fatty acids across the inner membrane of mitochondria. The researchers suggest several ways that ALC might contribute to an improvement in depression. One is that is seems to promote neuroplasticity in cerebral regions implicated in depression, such as the hippocampus. It could also work by increasing brain-derived neurotrophic factor (BDNF), which protects neurons and is important for learning and memory. ALC decreases release of the neurotransmitter glutamate by increasing the production of the inhibitory metabotrophic glutamate receptor (mGluR-2) on presynaptic glutamate neurons . Another way ALC might work is by normalizing lipid metabolism. Or it could modulate neurotransmitters, increasing serotonin and dopamine and protecting against stress.
In the meta-analysis, ALC produced more improvement in older patients than in younger ones. The researchers stressed the need for better treatments for older people, which may experience falls, cardiovascular disease, or increased mortality from antidepressants.
ALC also seems to improve pain syndromes, making it a good option for patients with both depression and pain symptoms.
Veronese and colleagues cited another meta-analysis that found that taking ALC in addition to an antidepressant led to lower rates of adverse events than the antidepressants alone, which helped patients adhere to their drug regimen.
In Animals, Exposure to High Fat Diet During Pregnancy Can Affect Offspring’s Neurological Development
New research in non-human primates suggests that exposure to a high fat diet during pregnancy and in early development prior to weaning can increase the offspring’s propensity for anxiety later in life.
The new research echoes 2010 findings about rats. Researcher Staci D. Bilbo and colleagues reported in the journal of the Federation of American Societies for Experimental Biology that in rats, a high fat diet during pregnancy and lactation led to offspring with greater body weight, increased inflammation, and problems with anxiety and spatial learning. Switching to a standard diet after weaning did not eliminate these outcomes.
The recent research by Jacqueline R. Thompson and colleagues, published in the journal Frontiers in Endocrinology in July 2017, suggests that maternal nutrition in the primate during pregnancy and lactation can have long-lasting effects on offspring’s neurological development, altering the brain and endocrine system. These changes occurred even if the offspring began a normal diet after weaning.
65 female Japanese macaques were divided into two groups, one that received a high-fat diet and one that received a normal diet. In the offspring of mothers who ate a high-fat diet, the researchers found impaired development of neurons containing serotonin. The offspring of the high-fat diet group also showed behavioral alterations such as increased anxiety.
The high rates of obesity in the US and other developed nations make these findings particularly important. The researchers suggest that 64% of women in the US who are of reproductive age are overweight, and 35% are obese. Co-author Elinor Sullivan suggested that the findings from the study could motivate mothers to make healthy nutritional decisions, not only for themselves but for their children as well.