Lithium Treatment Reduces Inflammation, Mania-Like Behavior in Rats
Patients with bipolar disorder often show increases in signs of inflammation, including levels of the proteins IL-2, IL-4, Il-6, IL-10 and tumor necrosis factor in their blood. Lithium is the most effective treatment for bipolar disorder, but it is not yet clear how it works. A recent study by researcher Joao de Quevado and colleagues determined that lithium can reduce the same inflammatory markers in rats.
Rats were treated with amphetamine to induce mania-like behavior, which was accompanied by increases in some of the same inflammatory markers in the blood and brain that are increased in people with bipolar disorder. Lithium treatment reduced both the manic behavior and levels of these inflammatory proteins in the rats.
The researchers concluded that lithium may treat mania by reducing inflammation.
Low Vitamin D Linked to Small Hippocampus & Schizophrenia
Low levels of vitamin D have been linked to schizophrenia in several studies. In one, infants with low vitamin D were more likely to develop schizophrenia in adulthood, but supplementation reduced this risk. A 2015 article by Venkataram Shivakumar and colleagues in the journal Psychiatry Research: Neuroimaging found that among patients with schizophrenia who were not currently taking (or in some cases, had never taken) antipsychotic medication, low levels of vitamin D were linked to smaller gray matter volume in the right hippocampus, an area involved in schizophrenia.
Vitamin D has neuroprotective effects and is important to normal brain development and function. Vitamin D is essential to the production of brain-derived neurotrophic factor (BDNF), a protein that is important for learning and memory, and vitamin D also reduces oxidative stress. BDNF deficiency and oxidative stress have both been linked to schizophrenia, and they both can cause abnormalities in the hippocampus.
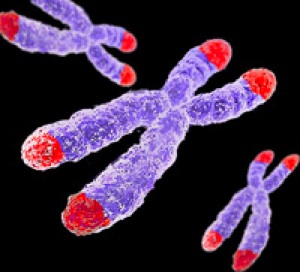
Crack Cocaine Use and Early Life Stressors Shorten Telomeres
Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Shorter telomeres are associated with aging and an increase in multiple medical and psychiatric disorders, while some healthy behaviors including exercising, eating healthy, meditating, and avoiding smoking can help maintain telomere length. Lithium treatment also increases telomere length.
Recent research by Mateus Levandowski and colleagues found that people who were dependent on crack cocaine had shorter telomeres than elderly women without psychiatric illnesses, particularly if the crack cocaine users had also experienced stress early in life, such as maltreatment or neglect.
Since short telomeres are associated with a variety of medical and psychiatric problems and premature aging, the combined effects of drug use and early life stressors are likely to have an adverse impact on people who have experienced both.
Thiamine (Vitamin B1) May Increase Effectiveness of Antidepressants
A new study suggests that the nutritional supplement vitamin B1, also known as thiamine, can improve symptoms of depression when taken with an antidepressant. Edith Holsboer-Trachsler and colleagues presented the research from their randomized, double-blind, placebo-controlled study at a recent scientific meeting. In a 12-week study, about 50 adults (averaging 35 years of age) with major depression were prescribed a selective-serotonin reuptake inhibitor (SSRI) antidepressant. In addition, half received thiamine supplements while the other half were given placebos. Starting at six weeks, those receiving thiamine with their antidepressant showed more improvement in their depressive symptoms than those receiving the antidepressant alone.
Thiamine is an essential nutrient for humans. It is found in foods such as yeast, pork, cereal grains, and certain vegetables. Thiamine deficiency has been linked to irritability and symptoms of depression, while thiamine supplementation can improve mood and reduce feelings of stress. No side effects were reported in the study.
Holsboer-Trachsler and colleagues hope that thiamine supplementation may help patients adhere to their antidepressant regimens by decreasing the time it takes until their moods begin to lift.
RTMS May Treat Cocaine Addictions
 In a pilot study, repeated transcranial magnetic stimulation (rTMS) reduced cocaine cravings and usage among people with cocaine addiction.
In a pilot study, repeated transcranial magnetic stimulation (rTMS) reduced cocaine cravings and usage among people with cocaine addiction.
RTMS is a non-invasive treatment in which a magnetic coil placed near the skull transmits electrical signals to the brain. It is an effective treatment for depression, and there is growing evidence that it may also be able to treat addictions.
Participants in the pilot study by researcher Antonello Bonci and colleagues received rTMS directed at their dorsolateral prefrontal cortex or pharmacological treatments (including medications to manage depression, anxiety, and sleep problems) over a 29-day study period. Among the rTMS recipients, 69% remained cocaine-free during the study period, compared to only 19% of those treated with medications. Those who received rTMS also reported fewer cravings.
There were few side effects among those who received rTMS, and there was a 100% compliance rate among the 32 participants, meaning they all showed up for each of their sessions.
Bonci and colleagues are working on a larger study that will compare rTMS treatment to a sham procedure rather than to a medication regime.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
In Rats, Dad’s Cocaine Use Affects Son’s Spatial Memory
Evidence is mounting that certain behaviors by parents can leave marks on their sperm or eggs that are passed on to their offspring in a process called epigenetics. In a recent study by researcher Mathieu Wimmer and colleagues, male rats that were exposed to cocaine for 60 days (the time it takes for sperm to develop fully) had male offspring who showed diminished short- and long-term spatial memory compared to the offspring of male rats that were not exposed to cocaine. Female offspring were not affected in this way.
The spatial tasks the offspring rats completed depended heavily on the hippocampus. Wimmer and colleagues believe that cocaine use in the fathers decreased the amount of a brain chemical called d-serine in the offspring. D-serine plays a role in memory formation and the brain’s ability to form synaptic connections. Injecting the offspring of rats who were exposed to cocaine with d-serine before the spatial memory tasks normalized the rats’ performance.
Yoga Therapy Improves Depression and Inflammation
Drug treatment for major depression can produce remission in 35–50% or patients. The others may need additional interventions, and some mind-body techniques have been successful. A recent randomized study by Anup Sharma and colleagues found that Sudarshan Kriya Yoga (SKY) decreased depression at one and two months when added to participants’ regular treatments. Participants who received the yoga treatment also showed reductions in inflammation in the blood, including lower levels of the inflammatory proteins TNF-alpha, IL-10, and CRP.
Cognitive Behavioral Therapy Improves Depression, PTSD by Improving Brain Connectivity
A recent study clarified how cognitive behavioral therapy improves symptoms of depression and post-traumatic stress disorder (PTSD). The participants were 62 adult women. One group had depression, one had PTSD, and the third was made up of healthy volunteers. None were taking medication at the time of the study. The researchers, led by Yvette Shelive, used functional magnetic resonance imaging (fMRI) to analyze participants’ amygdala connectivity.
At the start of the study, participants with depression or PTSD showed diminished connectivity between the amygdala and brain areas related to cognitive control, the process by which the brain can vary behavior and how it processes information in the moment based on current goals. The lack of connectivity reflected the severity of the participants’ depression. Twelve weeks of cognitive behavioral therapy improved mood and connectivity between the amygdala and these control regions, including the dorsolateral prefrontal cortex and the inferior frontal cortex. These regions also allow for executive functioning, which includes planning, implementation, and focus.
Mindfulness Therapy Improves Anxiety in Youth with a Bipolar Parent
Children of parents with bipolar disorder are prone to anxiety and emotional dysregulation, but treating these symptoms with antidepressants can provoke symptoms of mania. Thus, non-pharmacological treatements for anxiety and depression are needed. A recent study by Melissa DelBello found that twelve weeks of mindfulness-based cognitive therapy improved symptoms of anxiety and mood dysregulation in 20 youth with a bipolar parent. DelBello used functional magnetic resonance imaging (fMRI) to observe that the therapy increased activation of brain structures related to emotion and sensing. Amygdala activation differed between those with anxiety and those with mood dysregulation, suggesting that the therapy’s effect was on regions that modulate the amygdala, including prefrontal and insular regions, rather than on the amygdala itself.









