Transcranial Direct Current Stimulation Reduces Depression Following Strokes
One-third of people who have strokes face depression afterward. New research is looking to expand the safe options for the treatment of depression following strokes. At the 2015 meeting of the Society of Biological Psychiatry, researchers led by Leandro Valiengo presented their successful randomized, sham-controlled double-blind study of transcranial direct current stimulation for post-stroke depression. Forty-eight people who had depression following a stroke were randomized to receive either a sham procedure or tDCS in twelve 30-minute sessions over a period of six weeks. After the six weeks, those who received tDCS had fewer symptoms of depression, more remission, and better response. There were no serious side effects.
TDCS is very low-level electrical current that has a positive (anode) or negative (cathode) electrode. Anodal stimulation of the cortex is usually associated with positive effects on mood and cognition. TDCS sessions in this study consisted of 2-mA anodal left/cathodal right dorsolateral prefrontal stimulation.
Editor’s Note: Placebo-controlled studies have repeatedly indicated that patients who have a stroke show better neurological and psychiatric response afterward when they are given an selective serotonin reuptake inhibitor (SSRI) antidepressant, whether or not they have depression or a prior history of depression. If a neurologist does not suggest treatment with an SSRI after a stroke, ask why not. Since antidepressants increase brain levels of brain-derived neurotrophic factor (BDNF) and increase neurogenesis, they could help with post-stroke recovery.
“De Novo” Mutations in Dozens of Genes Cause Autism
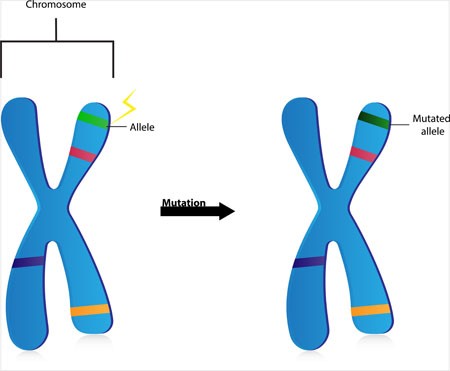
Two studies that incorporated data from more than 50 labs worldwide have linked mutations in more than 100 different genes to autism. Scientists have a high level of statistical confidence that mutations in about 60 of those genes are responsible for autism. So-called de novo mutations (Latin for “afresh”) do not appear in the genes of parents without autism, but arise newly in the affected child. The mutations can alter whether the genes get “turned on” or transcribed (or not), leading to disturbances in the brain’s communication networks.
The studies led by Stephan Sanders and Matthew W. State appeared in the journal Nature in late 2014. The identified genes fall into three categories. Some affect the formation and function of synapses, where messages between neurons are relayed. Others affect transcription, the process by which genes instruct cells to produce proteins. Genes in the third category affect chromatin, a sort of packaging for DNA in cells.
Before the new studies, only 11 genes had been linked to autism, and the researchers involved expect to find that hundreds more are related to the illness.
Editor’s Note: This new research explains how autism could be increasing in the general population even as most adults with autism do not have children. It should also put to rest the idea, now totally discredited, that ingredients in childhood immunizations cause autism. It is clearer than ever that kids who will be diagnosed with autism are born with these mutations.
With these genetic findings, the search for new medications to treat this devastating illness should accelerate even faster.
Bottom line: Childhood immunizations don’t cause autism, newly arising mutations in the DNA of parents’ eggs or sperm do. However, parental behavior could put their children and others at risk for the measles and other serious diseases if they do not allow immunizations. The original data linking autism to immunization were fraudulent, and these new data on the genetic origins of autism provides the best hope for future treatments or prevention.
Diabetes Drug Pioglitazone May Improve Bipolar Depression
The hypoglycemic drug pioglitazone is typically used to treat diabetes, but a 2015 study by A. Zeinoddini and colleagues shows that it may improve depressive symptoms in patients with bipolar disorder who do not have type 2 diabetes or the metabolic syndrome (characterized by high weight, cholesterol, triglycerides, and blood pressure).
Forty-four patients with bipolar disorder and a major depressive episode were randomized to receive either 30 mg/day of pioglitazone or placebo as an adjunctive treatment to lithium. Depressive symptoms were lower in the pioglitazone group at weeks 2, 4, and 6 of the six-week study.
No serious side effect occurred in the study, but pioglitazone use is associated with some risks in those using it for diabetes treatment. People taking pioglitazone for longer than a year have shown increased rates of bladder cancer. There is an increased risk of fractures of the upper arms, hands, and feet in female patients. The drug lowers blood sugar, but not enough to be a problem in people not taking other drugs that lower blood sugar. Pioglitazone can also cause fluid retention, worsening congestive heart failure. It can also cause mild weight gain, anemia, and sinus problems.
Clozapine-Induced Myocarditis More Common Than Thought
 New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
In 2010 Ronaldson and colleagues reported in the Journal of Clinical Psychiatry that tachycardia (rapid resting heart rate) and elevated levels of a group of proteins knows as troponin in the blood are almost always present during the first 45 days of treatment in patients who develop myocarditis. The researchers found that the time to onset of myocarditis was 14 to 22 days in almost all cases. Eosinophilia (high levels of a certain type of white blood cell) may occur in the week after peak troponin levels, and high levels of the inflammatory protein CRP (above 100mg/L) occurred in 79% of cases.
Ronaldson and colleagues suggest that patients who are prescribed clozapine be monitored for myocarditis during the first four weeks of treatment, particularly during the third week.
Genetic Variation Predicts Which Type of Antidepressant Will Be Effective
 In a six-month study of Caucasian patients, normal variations in the gene that is responsible for brain-derived neurotrophic factor (BDNF) predicted whether patients would respond better to a selective serotonin reuptake inhibitor (SSRI) antidepressant versus a serotonin and norepinephrine reuptake inhibitor (SNRI) or a tricycle antidepressant. There are several common variants of the BDNF gene, depending on which types of amino acids appear in its coding—valine or methionine. Patients with the most common version, two valines (or Val66Val), responded better to SSRIs. About two-thirds of the population has this version of the gene, which functions most efficiently. The remaining third have at least one methionine in the BDNF gene. Patients with a Met variation responded better to SNRIs and tricyclic antidepressants.
In a six-month study of Caucasian patients, normal variations in the gene that is responsible for brain-derived neurotrophic factor (BDNF) predicted whether patients would respond better to a selective serotonin reuptake inhibitor (SSRI) antidepressant versus a serotonin and norepinephrine reuptake inhibitor (SNRI) or a tricycle antidepressant. There are several common variants of the BDNF gene, depending on which types of amino acids appear in its coding—valine or methionine. Patients with the most common version, two valines (or Val66Val), responded better to SSRIs. About two-thirds of the population has this version of the gene, which functions most efficiently. The remaining third have at least one methionine in the BDNF gene. Patients with a Met variation responded better to SNRIs and tricyclic antidepressants.
The study by R. Colle and colleagues was published in the Journal of Affective Disorders in 2015. Of the patients who were prescribed SSRIs, 68.1% of patients with the Val/Val version responded to the medication after three months, compared to 44% of the patients with a Met version. Of patients prescribed SNRIs or tricyclics, 60.9% of the Met patients reached remission by six months, compared to only 33.3% of the Val/Val patients.
Editor’s Note: In an earlier BNN we reported that according to research published by Gonzalo Laje and colleagues in the journal Biological Psychiatry in 2012, depressed patients with the better functioning Val66Val allele of BDNF respond best to ketamine, while those with the intermediate functioning Val66Met allele respond less well.
More Evidence N-Acetylcysteine Added to Risperidone Improves Irritability in Autism
We reported in 2014 that researchers Ahmad Ghanizadeh and Ebrahim Moghimi-Sarani had found that the over-the-counter nutritional supplement n-acetylcysteine (NAC) added to the atypical antipsychotic risperidone reduced irritability in autism more than placebo added to risperidone.
A randomized, double-blind, placebo-controlled clinical trial published by M. Nikoo and colleagues in Clinical Neuropharmacology in 2015 replicated these results. Forty children with autism disorders aged 4–12 years were randomized to receive either risperidone plus NAC or risperidone plus placebo. Risperidone doses were between 1 and 2 mg/day, and NAC doses were 600 to 900 mg/day. By the end of the 10-week study, those children who received NAC had significantly greater reductions in irritability and hyperactivity/noncompliance than those who received placebo.
Editor’s Note: Three placebo-controlled studies have supported the efficacy of NAC in autism. One 2012 study, by A.Y. Hardan in Biological Psychiatry, evaluated monotherapy with oral NAC. In the other two, NAC was added to treatment with risperidone.
Inability to Balance on One Leg May Indicate Stroke Risk
A balance test may indicate declining cognitive health and risk for stroke. Researchers led by Yasuharu Tabara had previously found that balancing on one leg became more difficult for people with age. Now the same team has found that this type of postural instability is associated with decreases in cognitive functioning and with risk of stroke. Fourteen hundred participants with an average age of 67 were challenged to balance on one leg for up to 60 seconds. They also completed computer surveys, magnetic resonance imaging (MRI) scans, and a procedure to measure the thickness of their carotid artery. Those who could not balance on one leg for 20 seconds or longer were more likely to have cerebral small vessel disease.
Editor’s Note: Whether exercise would reverse this vulnerability remains to be seen, but lots of other data suggest the benefit of regular (even light) exercise on general health.
No Evidence Chelation Therapy Can Treat Autism
Some children with autism have been subjected to chelation therapy, which is used to remove heavy metals from the blood after poisoning. The rationale for using this therapy in autism was the discredited theory that autism resulted from mercury poisoning. A recent review of research on chelation therapy for autism by the Cochrane Collaboration, a nonprofit health research organization, found only one randomized controlled trial of chelation therapy, which had a flawed methodology and also found no evidence of a reduction in autism symptoms. This means there is no evidence that chelation therapy, which can lead to kidney failure or death, has any effect on autism symptoms. Based on the lack of evidence that the therapy has benefits for children with autism spectrum disorders, its great expense, and the dangers it poses, chelation therapy should not be prescribed as a treatment for autism.
Deep Transcranial Magnetic Stimulation Safe and Effective in Major Depression
Repeated transcranial magnetic stimulation is a non-invasive procedure that has been approved for the treatment of severe depression since 2008. In rTMS treatment, a figure-8–shaped electromagnetic coil is placed against the forehead and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain up to 1.5 cm deep. More recently, in 2013, the Federal Drug Administration approved a device with an H-shaped coil that delivers deep transcranial magnetic stimulation (dTMS). It can stimulate a wider area, and up to 8 cm deep.
Y. Levkovitz and colleagues have published the first double-blind randomized controlled multicenter trial of dTMS, reporting in the journal World Psychiatry that the intervention was effective and safe in patients who had not responded to antidepressant medication.
The study included 212 patients aged 22–68 years. All participants had failed to respond to one to four antidepressants or had not been able to tolerate the side effects of at least two antidepressants during their current episode of depression. The patients were randomized to receive either a sham treatment or 18 Hz dTMS over the prefrontal cortex acutely for four weeks and biweekly for 12 weeks for a total of 20 sessions.
The patients who received dTMS showed significantly greater improvement in symptoms than those who received the sham treatment, with a moderately large effect size of 0.76. Response and remission rates were also better in those who received dTMS. Response rates were 38.4% for the dTMS group versus 21.4% in the sham group. Remission rates were 32.6% for the dTMS group and 14.6% for the sham group. These difference in response remained stable during the three months of the study.
Side effects were minor except for a seizure that occurred when the protocol for the treatment was breached.
Inflammation Can Differentiate Apathy From Depression in Older Patients
In a new study by ESM Eurelings and colleague in the journal International Psychogeriatrics, the inflammatory marker C-reactive protein differentiated between older people with symptoms of apathy versus symptoms of depression. Higher levels of C-reactive protein were found in those with symptoms of apathy. The researchers concluded that apathy may be a manifestation of mild inflammation in elderly people.