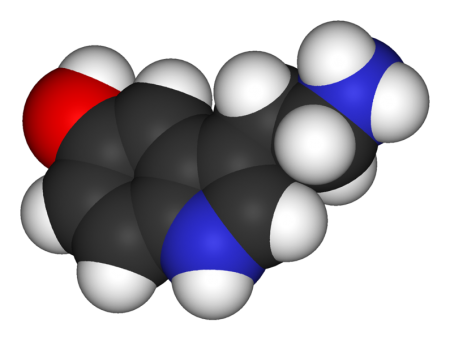
Serotonin 5-HT7 Receptors: Why Should We Care About Them?
5-HT7 is a type of receptor activated by the neurotransmitter serotonin. Some of the most potent effects of lurasidone (Latuda), an atypical antipsychotic with antidepressant effects in bipolar depression, and vortioxetine (Brintellix), a unique antidepressant for unipolar depression that also has positive effects on cognition, occur through the blockade of 5-HT7 receptors. The atypical antipsychotics aripiprazole and sulpiride also act on 5-HT7 receptors.
Researcher Agnieszka Nikiforuk summarized the research to date on 5-HT7 receptors in the journal CNS Drugs in 2015.
The receptors play a role in regulating sleep and circadian rhythms, which may explain why drugs that target them can be helpful in depression. Drugs that target 5-HT7 receptors have also improved learning and memory.
One subject of research into 5-HT7 receptors is whether better results come from blocking the receptors or stimulating them.
Blockade of 5-HT7 receptors has improved depression-like symptoms in animals and enhances the effects of sub-therapeutic doses of antidepressants. In other animal studies, stimulation of the receptors has appeared promising for the prevention of age-related cognitive decline.
More Evidence Vortioxetine Improves Depression and Cognitive Function
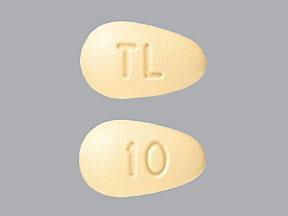 Vortioxetine (Brintellix) is a relatively new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), which work only on the serotonin transporter. In multiple studies, it has treated not only depression but also cognitive dysfunction. In a new study led by Atul Mahableshwarkar and published in the journal Neuropsychopharmacology, 10–20 mg/day of vortioxetine reduced symptoms of depression more than placebo and improved performance on tests of cognitive ability more than placebo and another antidepressant, duloxetine.
Vortioxetine (Brintellix) is a relatively new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), which work only on the serotonin transporter. In multiple studies, it has treated not only depression but also cognitive dysfunction. In a new study led by Atul Mahableshwarkar and published in the journal Neuropsychopharmacology, 10–20 mg/day of vortioxetine reduced symptoms of depression more than placebo and improved performance on tests of cognitive ability more than placebo and another antidepressant, duloxetine.
While depression is often accompanied by cognitive dysfunction, in this study vortioxetine seemed to directly treat the cognitive deficits rather than reducing them by alleviating the depression. The participants were aged 18–65.
Mental Illness Associated with 10 Years Lost Life Expectancy
Severe mental illness is one of the leading causes of death worldwide. Recently researchers led by E.R. Walker performed a meta-analysis of all cohort studies comparing people with mental illness to non-ill populations. They used five databases to find 203 eligible studies from 29 countries. Their findings, published in the journal JAMA Psychiatry in 2015, show that people with mental illness have a mortality rate 2.22 times higher than people without mental illness. People with mental illness lose a potential 10 years of life compared to those without severe mental disorders. The researchers estimated that 14.3% of deaths worldwide are attributable to mental illness.
Editor’s Note: Comorbid cardiovascular illness accounts for a large part of the disparity in life expectancy between people with and without mental illness. Those at risk for serious mental illness should pay close attention to their cardiovascular as well as psychiatric risk factors.
Lithium May Slow or Prevent Dementia
Lithium inhibits the enzyme glycogen synthase kinase 3, which has been implicated in dementia. To study whether lithium may prevent cognitive decline, researchers led by Tobias Gerhard looked at the medication histories of patients with bipolar disorder who were 50 years of age or older. In their article published in the British Journal of Psychiatry, those patients who had taken lithium 301–365 days out of the previous year had substantially lower risk of dementia than those who had not taken lithium during that time. Patients who had 300 or fewer days of lithium use did not have a significant reduction in dementia risk, nor did patients who were prescribed anticonvulsant drugs.
Editor’s Note: These data are consistent with those of Lars Kessing and colleagues, which suggest that patients in Denmark who renewed their lithium prescriptions were less likely to receive a diagnosis of dementia in old age.
In 2011, Orestes V. Forlenza and colleagues also reported in the British Journal of Psychiatry that compared to placebo, a very small dose of lithium, 150 mg/day, slowed the progression of mild cognitive impairment over one year.
Long-Term Lithium Treatment Has Risks for Kidney Function, Even with Precautions
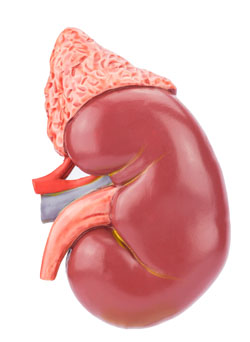 Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
The researchers, led by Harald Aiff, published the study in the Journal of Psychopharmacology in 2015. They identified 4,879 patients who had been prescribed lithium, and narrowed this list down to 630 adult patients who had taken lithium for at least 10 cumulative years, who had normal levels of creatinine when they began taking lithium, and on whom good data existed. About one-third of these patients had evidence of chronic renal impairment, and in 5% of these the impairment was severe or very severe.
Aiff and colleagues’ findings show that lithium treatment requires careful monitoring, especially over the long term. Patients must consider the risk/benefit ratio of lithium treatment. Since prevention of mood episodes can preserve an average ten years of life expectancy, and lithium has the best data for efficacy in preventing manic and depressive episodes, patients must weigh the risks of insufficiently treated bipolar illness against the possibility for long-term decreases in kidney function.
Vitamin B6 May Reduce Restless Legs in Patients Taking Antipsychotics
The atypical antipsychotic lurasidone (Latuda) is one of only a few drugs effective at treating bipolar depression. But 5–10% of patients who take lurasidone experience akathisia, or restless legs.
At a recent meeting, psychiatrist Cynthia Turner-Graham told this editor (Robert Post) of her success in treating a patient with lurasidone-related akathisia that had been resistant to all the standard treatments, including dose reduction, anticholinergic drugs, benzodiazepines, beta-blockers, etc. Vitamin B6 at a dose of 600mg twice a day gave the patient complete relief.
Dr. Turner-Graham was kind enough to direct me to a small double-blind study supporting this clinical observation in patients with schizophrenia who experienced akathisia from treatment with antipsychotics. The study by V. Lerner and colleagues was published in the Journal of Clinical Psychiatry in 2004.
Cognitive Behavioral Therapy an Effective Follow-up to ECT
While electroconvulsive therapy (ECT) is very effective treating acute depression, especially among patients who have not responded to antidepressants, relapse rates following ECT are high. Researchers have been exploring treatments that may extend the effectiveness of ECT and reduce relapses, including antidepressant medication and continuation ECT. A new study by Eva-Lotta Brakemeier and colleagues in the journal Biological Psychiatry finds that cognitive-behavioral therapy combined with medication was most effective at sustaining response to ECT.
In the study, 60 patients who responded well to three-times-per-week right unilateral ultra-brief ECT then were prescribed antidepressant medication following current guidelines for ECT followup. Of these patients, one-third were randomly assigned to receive the medications only. Another third were randomly assigned to receive the medications and continuation ECT, and the final third were randomly assigned to receive medication and participate in 15 weeks of cognitive-behavioral therapy in a group setting. Each group was observed at six months, and then at one year. The group who received medication and cognitive behavioral therapy had significantly higher response rates than the other groups at both follow-up evaluations.
After the initial treatment with ECT, 70% of the patients had responded and 47% had achieved remission. Following the six months of continuation treatment, 77% of the group that received medication and cognitive behavioral therapy responded, while only 40% of the group receiving medication and continuation ECT responded, and 44% of those receiving medication alone responded. After one year (six months following the end of treatment), response rates were 65% for those who had received medication and therapy, 28% for those who had received medication and ECT, and 33% for those who had received medication alone.
Editor’s Note: These results are striking for several reasons. As has been found in most studies, continuation ECT is not very effective at sustaining remission. Cognitive behavioral therapy with medication beats the other options hands-down. These results are in accord with others that show that cognitive behavioral therapy also helps prevent relapses in patients who responded well to medications. The take-home message is that people who respond well to antidepressant medication or ECT would do well to add cognitive behavioral therapy to their other preventive treatments.
The current study did not replicate parameters for continuation ECT that were successful in a study by Axel Nordenskjöld and colleagues in the Journal of ECT in 2013. Nordenskjöld used weekly ECT for six weeks and every two weeks thereafter, for a total of 29 ECT treatments in one year, and found this more intense regimen was more effective at preventing relapse than medication alone.
Bipolar Disorder Is Often Overlooked in Primary Care
A 2014 study by Joseph M. Cerimele and colleagues in the journal Psychiatric Services found that primary care patients with bipolar disorder had severe depression and anxiety, symptoms of other psychiatric illnesses, and psychosocial problems such as housing difficulties, homelessness, or lack of support. Only 26% were referred to specialty mental health care despite the severity of these problems. These findings suggest the primary care setting, where many patients obtain their care, provides insufficient support for people with bipolar disorder.
Editor’s Note: There are several way to overcome the deficient recognition and treatment of bipolar disorder in primary care:
Record mood fluctuations
It is critical that patients keep a detailed longitudinal record of mood fluctuations in order to enhance the likelihood that their doctor can perform a well-informed evaluation and assessment of the effects of treatment. Several ways of doing this are available. We offer a variety of printable daily mood charts available on our website. Another option is What’s My M3, a free app that can be downloaded from the Itunes Store or Google Play. In a three-minute survey, it screens for depression, anxiety, OCD, PTSD, and mania. The ratings can be done longitudinally and printed out to assist a physician in the evaluation, assessment of course of symptoms, and response to treatment.
Parents of children aged 2–12 with mood or behavioral problems (or at risk for them because they have a parent with a diagnosis of depression or bipolar disorder) can rate their children each week as part of a new study. These ratings, which will help determine how children with symptoms of mental illness are being treated in the community, are done via a secure website and can be printed out to help a treating physician or other clinician to evaluate the children’s course of illness and responses to treatments. Access to informed consent documents and more information about participation in the study, known as the Child Network, is available here.
Learn about mood disorders
Patients should educate themselves about the signs and symptoms of mood disorders. Many books on this topic are available, and the BNN newsletter tries to update patients and clinicians about the latest findings about the treatment of depression and bipolar disorder.
Get extra help
Patients can seek out consultations with experts in bipolar disorder, who may be able to provide extra guidance to help primary care physicians arrive at the appropriate diagnosis or find an optimal treatment plan and back up approaches if the initial options do not bring about remission.
Finding a psychotherapist who can provide psychoeducation about bipolar disorder and cognitive behavioral or other specialized therapies may also be of great use, as more than a dozen randomized studies document the effectiveness of psychoeducation and/or psychotherapy compared to treatment as usual.
Talk about mood at every medical evaluation
Many medical problems such as heart disease and diabetes require careful monitoring, with patients as active participants. Likewise, careful monitoring of mood is a critical component of good treatment and should yield positive short-term and long-term results in recurrent depression and bipolar disorder.
Since depression can complicate many medical illnesses, patients should get in the habit of asking physicians not only about their blood sugar, blood pressure, or cholesterol, but also, “What about my low mood, anxiety, or insomnia?” It may be just the spark a physician needs to better attend to these equally important health issues.
Low Dose Quetiapine Promising In Borderline Personality Disorder
Borderline personality disorder is characterized by mood instability, cognitive symptoms, impulsive or risky behavior, and disturbed interpersonal relationships. There are no Federal Drug Administration–approved treatments, but several small open studies of the atypical antipsychotic quetiapine (trade name Seroquel) have been promising. Rapid mood shifts in borderline personality disorder resemble to some extent those in bipolar disorder, for which quetiapine is an approved treatment. The drug may also curb impulsivity and self-harm. A blind, placebo-controlled study by Donald W. Black and colleagues published in the American Journal of Psychiatry in 2014 compared a low dose of quetiapine (150mg/day) with a moderate dose (300mg/day) and with placebo for the treatment of borderline personality disorder. The low dose of quetiapine led to significant improvement over the other doses, particularly reducing verbal and physical aggression.
The study included 95 participants randomized to each of the three treatment groups. All met DSM-IV criteria for borderline personality disorder, and each participant received eight weeks of active treatment. (One week of 50mg/day followed by seven weeks of 150md/day for the low dose group, and one week of 50mg/day followed by 3 weeks of 150mg/day and 4 weeks of 300mg/day for the moderate dose group.)
Eighty-eight percent of the participants experienced an adverse event during the study, including sedation, dry mouth, increased heart rate, or decrease in blood pressure. None were serious. Sedation was most common in the group receiving moderate doses of quetiapine.
All groups improved over the 8-week study, particularly during weeks 2–6. Response rates of participants who completed the study were 82% for the low dose group, 74% for the moderate dose group, and 48% for placebo. (Large benefits from placebo are common in studies of borderline personality.) Improvement in symptoms was greatest in the low dose quetiapine group, significantly higher than the moderate dose quetiapine group. Time to improvement was shorter on quetiapine than on placebo.
Subthreshold Episodes of Mania Best Predictor of Bipolar Disorder in Children
Relatively little attention has been paid to the children of a parent with bipolar disorder, who are at risk not only for the onset of bipolar disorder, but also anxiety, depression, and multiple other disorders. These children deserve a special focus, as on average 74.2% will receive a major (Axis 1) psychiatric diagnosis within seven years.
New research published by David Axelson and colleagues in the American Journal of Psychiatry describes a longitudinal study comparing children who have a parent with bipolar disorder to demographically matched children in the general public. Offspring at high risk for bipolar disorder because they have a parent with the disorder had significantly higher rates of subthreshold mania or hypomania (13.3% versus 1.2%) or what is known as bipolar disorder not otherwise specified (BP-NOS); manic, mixed, or hypomanic episodes (9.2% versus 0.8%); major depressive episodes (32.0% versus 14.9%); and anxiety disorders (39.9% versus 21.8%) than offspring of parents without bipolar disorder. Subthreshold episodes of mania or hypomania (those that resemble but do not meet the full requirements for bipolar disorder in terms of duration) were the best predictor of later manic episodes. This finding was observed prospectively, meaning that patients who were diagnosed with manic episodes during a follow-up assessment were likely to have been diagnosed with a subthreshold manic or hypomanic episode during a previous assessment.
The study included 391 children (aged 6–18) of at least one bipolar parent, and compared these to 248 children of parents without bipolar disorder in the community. The participants took part in follow-up assessments every 2.5 years on average, for a total of about 6.8 years. Each follow-up assessment included retrospective analysis of symptoms that had occurred since the previous assessment.
In addition to having more subthreshold manic or hypomanic episodes; manic, mixed, or hypomanic episodes; and major depressive episodes, the high-risk children also showed more non-mood-related axis 1 disorders, including attention deficit hyperactivity disorder (ADHD), disruptive behavior disorders, and anxiety disorders than the children of parents without bipolar disorder. Axelson suggested that monitoring for these symptoms may help with early identification and treatment.
Children with a bipolar parent were diagnosed with bipolar spectrum disorders at rates of 23% compared to 3.2% in the comparison offspring. Mean age of onset of mania or hypomania in the high-risk offspring was 13.4 years. Of those offspring who had a manic episode, more than half had the episode before age 12, with the earliest occurring at age 8.1.
Compared to previous studies of children of parents with bipolar disorder, this study found that the mean age of onset of manic or hypomanic episodes was younger, possibly because other studies did not include young children. Another new finding was that major depressive episodes were risk factors for mania and hypomania but did not always precede the onset of mania or hypomania in the high-risk offspring.
Parents of children who are at high risk for developing bipolar spectrum disorders should be aware of the common precursors to mania—subthreshold manic or hypomanic symptoms and non-mood disorders—and make sure that clinicians assess for these symptoms and differentiate them from the symptoms of depression or other disorders.
Editor’s Note: In Axelson’s study, 74.2% of the offspring of a bipolar parent suffered a major (Axis I) psychiatric disorder. However, 48.4% of the offspring from the comparison group of community controls also had an Axis 1 psychiatric disorder. These high rates of illness and dysfunction indicate the importance of monitoring a variety of symptom areas and getting appropriate evaluation and treatment in the face of symptoms that are associated with impairment in both high risk children and in the general population.
One way of doing this is for parents to join our new Child Network, a study collecting information about how children at risk for bipolar disorder or with symptoms of bipolar disorder are being treated in the community and how well they are doing. Parents rate their children on a weekly basis for depression, anxiety, ADHD, oppositionality, and mania-like symptoms. Parents will be able to produce a longitudinal chart of their children’s symptoms and response to treatment, which may assist their child’s physician with early detection of illness and with treatment. See here for more information and to access informed consent documents.