Inflammatory Markers of Bipolar Illness Course
 People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Ben Goldstein reported on a study that examined levels of TNF alpha, IL-6, and high sensitivity CRP (hsCRP) in 123 adolescents with an average age of 20.4 years, who had been ill for an average of 12.7 years.
CRP levels in adolescents with bipolar illness were equivalent to those with rheumatoid arthritis, and much higher than healthy controls. In children with bipolar disorder, higher levels of CRP were related to more time symptomatic. High hsCRP was related to lower socio-economic status and to substance abuse disorders.
Increases in IL-6 were linked to a longer time to achieve remission and more weeks depressed. High IL-6 was related to duration of illness, positive family history of substance use, and family conflict.
High TNF alpha was related to low socioeconomic status (SES), self-injury, suicidal ideation, and positive life events.
Goldstein said studies of these markers could eventually lead to therapeutic advances, but the process would be long and would require several steps: proof of concept studies, prospective validation studies in independent samples, and demonstration of clinical gains over standard predictive markers, culminating in enhanced patient care and outcome through better, faster prediction of response.
Editor’s Note: Ideally clinicians could jump ahead by immediately attempting to determine whether adding a medication with direct anti-inflammatory effects could enhance therapeutic effects in children with elevated inflammatory markers. Treating inflammation could also theoretically help prevent cognitive deterioration and decrease the considerable risk for cardiovascular dysfunction in patients with bipolar disorder.
High CRP Predicts Early Onset Of A Mood Episode
Barbara Gracious of Ohio State University became interested in the inflammatory marker CRP through studying vitamin D3 deficiency. Vitamin D is a neurosteroid, and low levels of it have been associated with risk of schizophrenia, cardiovascular disease (heart attack), diabetes, mood disorders, cognitive deficits, autoimmune disease, and obesity. High CRP levels are related to low vitamin D, to obesity, and to other inflammatory markers such as IL-6 and TNF alpha.
Gracious measured these levels of CRP in 621 children participating in the Longitudinal Study of Manic Symptoms (LAMS), who were followed up for many years. She found that those with higher levels of CRP developed a mood episode approximately two years earlier than those with normal levels. CRP binds phosphocholine, which activates complement, a kind of protein that induces inflammation. CRP is elevated in 14% to 53% of patients with depression and anxiety.
Copeland et al. reported in the American Journal of Psychiatry in 2012 that after a first depression, high CRP was associated with relapse. CRP also increases in adolescent females (who are at increased risk for depression).
Editor’s Note: These findings suggest the potential importance not only of using CRP as an indicator of depression risk, but also of targeting CRP levels in the hopes of reducing risk of a mood episode in children with elevated inflammatory markers. Supplementing vitamin D3 in those with low levels would be a good place to start, as would preventing or treating obesity and promoting good sleep hygiene and exercise. The potential role of medications with direct anti-inflammatory effects such as aspirin (acetylsalicylic acid) or minocycline deserves further study.
Balanced diet, exercise, and good sleep habits may be easier said (or recommended) than done. Such lifestyle advice must be delivered with motivational interviewing, and instilled through practice, positive feedback, encouragement, and more practice. In children in general, and especially in those at high risk for a mood episode due to a family history of a unipolar or bipolar mood disorder, starting things off right from the outset with good diet, exercise, and sleep routines would be highly recommended. The benefits for long-term health and wellbeing could be enormous.
The results of good health behaviors may be mediated through several pathways. They could lessen inflammation and obesity, increase brain-derived neurotrophic factor (BDNF, which is important for new synapses and long-term memory) and neurogenesis (both of which are increased by exercise), and even lengthen the telomeres that cap the ends of each strand of DNA (short ones are associated with a variety of medical and psychiatric illnesses).
Salt Implicated in Autoimmune Diseases
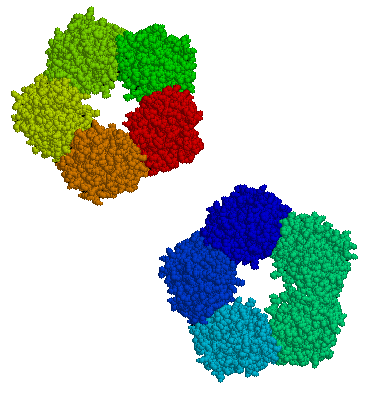
Autoimmune diseases, in which the body’s immune system begins to attack healthy tissue, have become much more common in recent decades. Some autoimmune problems are related to overproduction of TH17 cells, immune cells that produce a particular inflammatory protein (interleukin-17), but it is not clear why some people’s bodies start producing too many TH17 cells. Three studies published in the journal Nature in 2013 suggest that salt may play a role. They were recently summarized in Scientific American.
In the first study, researchers developed a model of how TH17 cells are controlled. In the second, they observed how immune cells are produced over a period of several days. The researchers noticed that a protein called serum glucocorticoid kinase 1 (SGK1), which is known to regulate salt in cells, seemed to act as a signal for TH17 production. Mouse cells in high-salt environments had more SGK1 and produced more TH17. The third study confirmed the connection with salt using both mouse cells and human cells.
While mice with multiple sclerosis (an autoimmune disease) worsen on a high-salt diet, it is not clear that salt in the diet is related to TH17 production. It is also not clear that slowing TH17 production is the answer to autoimmune diseases since autoimmunity differs across patients and disorders. However, in any event, low-salt diets are recommended for general health concerns, such as blood pressure.
Anti-inflammatory Celecoxib Improved Depression When Added to Escitalopram
Research has previously shown a link between stress, inflammation, and mood diorders. Anti-inflammatory treatments are now being explored for depression. In an abstract presented at the 2013 meeting of the Society of Biological Psychiatry, Nadia Alvi et al. reported that the commonly used anti-inflammatory COX-2 inhibitor celecoxib (Celebrex) showed better antidepressant effects than placebo when added to the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram (Lexapro) in an 8-week study.
While this research has not yet been peer-reviewed, it can be found in the 2013 convention supplement (9S) to the journal Biological Psychiatry as abstract #661.
Editor’s Note: These data are consistent with an emerging literature that shows there are increases in signs of inflammation in both unipolar and bipolar depression. It remains to be determined whether those patients whose blood shows markers of inflammation (such as increases in C-reactive protein (CRP), interleukins 1 and 6, and TNF-alpha) are more likely to respond to anti-inflammatory treatment than patients in general.
CRP in Blood Predicts Onset of New Episode in Childhood Mood Disorders
At the 2013 meeting of the International Society for Bipolar Disorders, researcher Barbara Gracious presented evidence that increased levels of high sensitivity c-reactive protein (hsCRP), a marker of inflammation, were associated with an increased risk for developing a full-blown mood episode in 71 youth (average age 13.8) participating in a study called Longitudinal Assessment of Manic Symptoms (LAMS-2). The children were selected for the study because they had manic symptoms that were not severe enough to meet criteria for a diagnosis of bipolar I or II disorder. This research has not yet been published in a peer-reviewed journal, but the abstract can be found in first 2013 supplement of the journal Bipolar Disorders (page 67).
CRP levels are also known to predict cardiovascular disease and Type II diabetes.
Levels of 25-OH vitamin D, TNF?, and IL-6 did not predict a later mood disorder.
Editor’s Note: These data suggest the importance of assessing CRP and other markers in youth who are either prodromal (having early symptoms of a mood disorder) or at high risk because of a family history of a mood disorder.
The next step for clinical research would be to determine what treatment might decrease CRP and whether it would also prevent the development of mood episodes.
Inflammatory Markers May Predict Antidepressant Response
There appears to be a link between inflammation and depression. In the journal Neuropsychopharmacology, Cattanes et al. reported in 2013 that compared to controls, depressed patients had significantly higher baseline levels of inflammatory cytokines, less glucocorticoid receptor function, less neuroplasticity, and fewer neuroprotective factors. Certain variables predicted response to treatment, others were seen only in responders, and still others changed in everyone with antidepressant treatment.
Higher baseline levels of inflammatory markers interleukin IB, macrophage inhibitory factor (MIF), and tumor necrosis factor TNF? were each associated with nonresponse to antidepressant treatment, and the three combined accounted for 50% of the variance in response—that is, they were the major predictor of whether a patient responded to treatment.
Levels of other factors changed in only those patients who responded well to antidepressants. The biggest changes were the normalization in levels of the neurotrophic factors BDNF and VEGF.
Several other markers normalized with antidepressant treatment regardless of whether the patients responded to treatment, and these included decreases in cytokines interleukin-IB and MIF and improved glucocorticoid receptor function.
The three different kinds of findings about these biomarkers were observed regardless of what type of antidepressant was used—SSRI versus tricyclic nortriptyline (which blocks norepinephrine reuptake).
Editor’s Note: This study replicates other studies in depression where signs of inflammation have been observed, including increases in inflammatory cytokines, decreases in glucocorticoid receptor function (needed to suppress high levels of the stress hormone cortisol) and lower levels of neuroplasticity and neuroprotection markers. This, however, is one of the first studies to show that levels of these markers at baseline may predict response to antidepressant treatment.
Also novel are the findings that while some high interleukin levels at baseline predicted antidepressant non-response, other ones normalized only in responders, and still others changed with treatment independent of whether the patients’ depression improved. These exciting findings require replication, but suggest the future possibility of personalized medicine, that is, choosing medications based on an individual biochemical marker profile. Eventually direct use of anti-inflammatory agents may be necessary in those with the highest levels of cytokines (predicting non-response to conventional antidepressant treatment). The same types of studies are needed in bipolar depression to determine the relationship between these inflammatory markers and treatment response.
Inflammation and Anti-Inflammatories in Depression
Depression is often associated with increases in markers of inflammation in blood, which include IL-1, IL-6, TNF-alpha, and CRP. Risk factors for increased inflammation include stress, obesity, a diet high in omega-6 fatty acids, sedentary lifestyle, social isolation, low socio-economic status, smoking, and being female. Treatments such as lithium, other mood stabilizers, and antidepressants can all have anti-inflammatory effects.
At the International Congress of Neuropsychopharmacology in 2012, researcher Michael Berk reviewed data on inflammation in depression. Berk shared prospective data that in the general population, people whose levels of CRP fall within the highest third have the highest risk for a new onset of depression over the next 9 years, while those with CRP values in the lowest third (indicating low inflammation) had the least likelihood of becoming depressed.
Drugs with more direct anti-inflammatory properties are beginning to be studied in unipolar depression with some success. In a trial by Abbasi et al. published in the Journal of Affective Disorders in 2012, the anti-inflammatory COX-2 inhibitor celecoxib (Celebrex) when added to the selective serotonin reuptake inhibit (SSRI) sertraline (Zoloft) had better antidepressant effects than the addition of placebo.
Sepaujnia et al. reported in Neuropsychopharmacology in 2012 that an anti-diabetes drug that also has anti-inflammatory properties, pioglitazone (Actos), also beat placebo in depression.
Laan et al. reported in the Journal of Clinical Psychiatry that the same was true of acetylsalicylic acid (ASA or aspirin).
Finally, Berk summarized data that the class of cholesterol-lowering drugs called statins are also able to decrease CRP and improve or prevent depression. Epidemiological data by Pasco et al. published in Psychotherapy and Psychosomatics showed that subjects without depression were less likely to develop a new onset of depression if they were treated with statins compared to those who were not. Stafford et al. reported in the Journal of Clinical Psychiatry in 2010 that patients taking statins had a 79% decreased likelihood of depression at 9 months of follow-up. A third study in Sweden showed that simvastatin, a lipophilic (fat-soluble) drug that can readily enter the brain, decreases the incidence of depression more than some of the non-lipophilic statins.
Moreover, a meta-analysis by O’Neil et al. reported that overall, statins had positive effects on mood.
Editor’s Note: All these data come from studies of unipolar depression, so one must consider how relevant they are to bipolar depression. They may be pertinent, since elevated inflammatory markers have consistently been reported in bipolar depression. However, this cannot be assumed until appropriate studies are performed. (As usual, research in bipolar depression lags far behind that in unipolar depression.)
Preliminary uncontrolled retrospective data from one study did suggest that those treated with lithium plus aspirin did better than those on lithium and no anti-inflammatory.
Thus it may make sense for unipolar and bipolar depressed patients with risk factors for heart disease such as a positive family history of heart disease and elevated cholesterol and triglycerides to discuss with their doctors the possibility of starting statin treatment earlier rather than later. This is because depression itself is a major risk factor for heart disease, so statins might lower risk both by their approved indication of lowering cholesterol and by their apparent ability to help fend off new episodes of depression.
A more complicated issue would be the question of when, if at all, to use primary anti-inflammatory drugs in the adjunctive treatment of unipolar or bipolar depression. Read more
Immune Mechanisms Are Important to the Emergence of Defeat Stress–Induced Depressive Behaviors
At a recent scientific meeting, researcher Georgia E. Hodes presented evidence that in mice, the immune system may play a role in behaviors that resemble human depression. Repeated social defeat stress (when an intruder mouse is threatened by a larger mouse defending its territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit social avoidance and lose interest in sucrose. Hodes et al. determined that interleukin 6 (IL-6), an inflammatory cytokine, or signaling molecule, secreted into the blood was crucial to these behaviors. When the researchers injected mice with antibodies that block the effects of IL-6, or when they irradiated the mice’s peripheral immune system to prevent the formation of IL-6, the depressive behaviors did not emerge following defeat stress.
Editor’s Note: There are increasing data that immunological and inflammatory mechanisms play a role in human affective disorders, and these preliminary data raise the possibility that blocking some immune mechanisms more directly in humans could be a novel therapeutic approach to explore in the future.
Aspirin added to Regular Treatment Reduces Symptoms of Schizophrenia
Most drugs used to treat schizophrenia target dopamine and serotonin receptors in the brain. While these are effective in many patients, relapse is common and side effects can be severe. Researchers are looking for ways to target other mechanisms that cause schizophrenia, and inflammation seems to be one of these. There is evidence that a treatment as simple as aspirin, when added to regular treatment with antipsychotics, can improve schizophrenia by targeting inflammation.
In a 2010 study by Laan et al. published in the Journal of Clinical Psychiatry, patients with moderate or severe schizophrenia were given either placebo or aspirin (acetylsalicylic acid, 1000mg) in addition to their regular treatments every day for three months. The patients who received aspirin showed a significant reduction in the positive symptoms of schizophrenia, and to a lesser extent the negative symptoms, compared to those who received placebo. Cognitive function was not improved. The effect size (Cohen d) for the total scale score was 0.5, which is considered a “medium” effect and one that is clinically relevant.
The reductions in symptoms were greater in those patients who had more altered immune function.
Depressive Symptoms Negate Effects of Heart-Healthy Behaviors
Physical activity and light to moderate drinking (as is often associated with the Mediterranean diet) are recommended as ways to reduce risk for heart disease and type 2 diabetes. New research shows that among healthy people, symptoms of depression can counteract the anti-inflammatory benefits of both exercise and light to moderate alcohol consumption.
C-reactive protein (CRP) is a cardiometabolic risk marker. High measures of CRP are a sign of inflammation. Leisure-time physical activity and light to moderate alcohol intake (defined as about half a drink per day for women and one drink per day for men) are associated with lower levels of CRP. Depression is associated with higher levels.
A study by Edward C. Suarez et al. published recently in the journal Brain, Behavior, and Immunity examined 222 nonsmoking men and women aged 18-65 years. These participants were physically healthy and had no history or diagnosis of psychiatric conditions. Participants recorded the amount of alcohol they consumed and the amount of physical activity in which they participated. CRP levels in their fasting blood samples were measured, and they also completed an inventory of depressive symptoms.
Those people who were physically active had lower levels of CRP, but the 4.5% of participants with depressive symptoms did not see any anti-inflammatory benefits from physical activity. Similarly, light to moderate drinking was associated with lower levels of CRP only in men who were not depressed.
Depression did not seem to affect other markers of physical health in this study, such as levels of triglycerides or cholesterol.
Editor’s Note: This study suggests that treating depressive symptoms should be a part of any plan to reduce cardiovascular risk. It seems that depression has effects that go beyond psychological distress and may prevent patients from reaping the benefits of their healthy behaviors. The effect of depression in preventing heart healthy changes in CRP could be one of many factors mediating the high levels of cardiovascular risk in depression. People with depression are twice as likely to have a heart attack than those without depression.