Lithium Increases the Volume of the Prefrontal Cortex in Responders
 Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
This study reported that patients whose illness failed to respond to lithium had smaller right amygdalas than euthymic bipolar I patients or healthy controls. After treatment with lithium, those who responded well to the drug showed significant enlargement of the left prefrontal cortex and the left dorsolateral prefrontal cortex, while those who responded poorly to lithium showed decreases in the volume of their left hippocampus and right anterior cingulate cortex.
Editor’s Note: This is one of several studies that suggest a relationship between volume of brain regions and degree of response to lithium. These data add to the remarkably consistent literature suggesting that lithium may have neurotrophic and neuro-protective effects, potentially because of the drug’s ability to increase neuroprotective factors such as BDNF and Bcl-2 while decreasing cell death factors such as BAX and p53.
Amygdala Size Linked to Manic Symptom Severity
 In two posters presented at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, a research group led by Kiki Chang reported that increased severity of manic symptoms is associated with increased size of the amygdala (especially the right amygdala) in adolescents who are at high risk for developing bipolar disorder.
In two posters presented at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, a research group led by Kiki Chang reported that increased severity of manic symptoms is associated with increased size of the amygdala (especially the right amygdala) in adolescents who are at high risk for developing bipolar disorder.
The amygdala is a crucial area for emotion regulation. The increasing size, either with more manic symptoms or as patients with bipolar disorder age into adulthood compared to normal volunteer controls (as we describe in the article on brain imaging at far left) could reflect increased use of the amygdala in bipolar disorder.
The increased amygdala size could be linked to increased emotion dysregulation, or it could be a compensatory mechanism in which the amygdala works harder to exert better emotion control.
Experience-dependent neuroplasticity describes a phenomenon in which the volume of a brain area increases as it gets more use (like a muscle that grows when it gets more exercise). One interesting example in which this may occur is London taxi drivers, who have larger hippocampi than the general public. (The hippocampus is responsible for some of the brain’s spatial recognition abilities.) This could be explained in two different ways. The discrepancy in size between the hippocampi of taxi drivers and of the general population may exist because the taxi drivers’ brains change over the course of their careers via experience-dependent neuroplasticity, or it may exist because those with excellent spatial recognition abilities and bigger hippocampi choose to become taxi drivers.
White Matter Abnormalities in the Brain Predict Onset of Psychosis
 At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
Bearden found that the degree of white matter abnormality seen during magnetic resonance imaging (MRI) was proportional to the degree of cognitive deficit in patients who subsequently developed a first episode of psychosis. The white matter abnormalities were seen particularly in the superior longitudinal fasciculus (SLF) and were associated with increased severity of symptomatology. The overall degree of white matter alteration was also significantly related to clinical outcome 15 months later.
Editor’s Note: The SLF is a major neuronal conduit between prefrontal cortical systems, which are responsible for cognition and planning, and the parietal cortex, which is responsible for spatial abilities. Disruption of this fiber track has been related to difficulties in social cognition and “theory of mind” concepts, like inferring what others might be thinking.
Brain Imaging Finds Abnormalities that Appear Over the Course of Childhood-Onset Bipolar Illness
 There is considerable evidence that children with bipolar disorder have smaller amygdalas, and the amygdala also appears to be hyper-reactive when these children perform facial emotion recognition tasks. A symposium on longitudinal imaging studies in pediatric bipolar disorder was held at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry to shed light on other brain abnormalities in these children.
There is considerable evidence that children with bipolar disorder have smaller amygdalas, and the amygdala also appears to be hyper-reactive when these children perform facial emotion recognition tasks. A symposium on longitudinal imaging studies in pediatric bipolar disorder was held at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry to shed light on other brain abnormalities in these children.
Researcher Nancy Aldeman reported that there is some evidence children with bipolar disorder have decreased gray matter volume in parts of the brain including the subgenual cingulate gyrus, the orbital frontal cortex, and the superior temporal gyrus, as well as the left dorsolateral prefrontal cortex and amygdala. At the same time there is evidence of increased size of the basal ganglia. These abnormalities do not appear to precede the onset of the illness.
Some changes occur over the course of the illness. The basal ganglia seem to increase in volume in patients with bipolar disorder, but decrease in volume in those with severe mood dysregulation and comorbid ADHD. Moreover, parietal cortex and precuneus cortex volumes appeared to increase in children with bipolar disorder while decreasing or staying the same in normal volunteer controls.
A meta-analysis of brain imaging studies indicated that in general, the size of the amygdala appears to increase from childhood to adulthood in bipolar patients, starting out smaller than that of similarly-aged normal volunteers, but becoming larger than that of adult normal volunteers as the patients age into adulthood.
Lithium treatment increases gray matter volume in a variety of cortical areas and in the hippocampus in multiple studies. In contrast, treatment with valproate for 6 weeks appears to decrease hippocampal volume.
Cortex Shrinks and Amygdala Grows in Childhood Bipolar Disorder
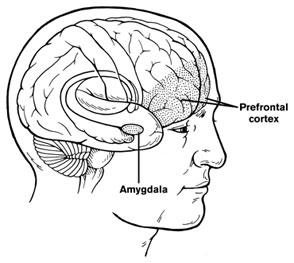 At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
Chang cited the study of Singh et al. (2010) who found that the subgenual anterior cingulate volume early in the course of illness was smaller in adolescent-onset bipolar disorder compared to controls. Given this evidence of prefrontal cortical and anterior cingulate deficits, Dr. Chang raised the possibility that treatment with lithium and other agents with potential neurotrophic and neuroprotective effects might be able to prevent these neurobiological aspects of illness progression in young patients.

