Sunovion Drug in Development Targets 5HT7 and D2 Receptors to Treat Bipolar Depression

At a recent meeting, President and CEO of Sunovion Pharmaceuticals Antony Loebel presented the results of a recent double-blind, placebo controlled study of a drug in development for the treatment of bipolar depression, currently known as SEP-4199. The drug has a fixed ratio of 85% aramisulpride and 15% esamisulpride that target serotonin 5-HT7 receptors and dopamine D2 receptors, respectively. The drug was optimized to amplify the antidepressant effects that come from affecting 5-HT7 while minimizing D2-related side effects.
A total of 344 patients were randomized into three equal groups, in which patients received placebo or a fixed dose of SEP-4199, either 200mg/day or 400mg/day.
The results were promising. After 6 weeks, scores on the Montgomery Asberg Depression Rating Scale (MADRS) were higher among patients who received SEP-4199. The results were very close to statistical significance (p=0.054), with the placebo group showing a large improvement that may have contributed to the lack of difference across groups. In each dosage group, there was greater improvement in MADRS scores than was seen in the placebo group. There was also greater improvement on the Quick Inventory of Depression Symptomatology (QIDS-SR-16) and on the Hamilton Anxiety Rating Scale (HAM-A) in each dosage group compared to placebo.
Loebel concluded that the results showed proof of concept for the use of SEP-4199 to treat bipolar depression, and they plan to continue their research on the drug.
Lurasidone Effective Long-Term in Pediatric Bipolar Depression

At the 2020 meeting of the American Society of Clinical Psychopharmacology, researcher Manpreet Singh presented data showing that children aged 10–17 with bipolar depression had an excellent long-term response to the antipsychotic medication lurasidone (trade name Latuda).
Lurasidone has been approved by the US Food and Drug Administration as a monotherapy treatment of bipolar depression in children and adolescents since 2018. Following a six-week double-blind study comparing lurasidone with placebo in 305 children and adolescents, Singh and colleagues carried out an open-label extension study in which all of the young participants, including those in the placebo group, had the option of taking lurasidone for up to two more years.
Of those, 195 children completed one year of treatment, and 93 completed two years of treatment. Rates of response were 51.0% after the six-week preliminary study; 88.4% at one year; and 91.1% at two years. Rates of remission were 24.3% after the six-week study; 61.3% at one year, and 75.6% at two years, while rates of recovery were 17.7% after the preliminary study; 53.8% at one year; and 73.8% at two years.
This improvement in depression had a strong correlation with improvement in functioning, as measured by the Children’s Global Assessment score (CGAS). The results show progressive increases in rates of response, remission, and recovery with duration of treatment that are associated with improvement in functioning.
In Phase 3 Clinical Trials, Antipsychotic Treatment Lumateperone Is Found Effective in Bipolar Depression
Lumateperone is an antipsychotic medication that is currently approved by the US Food and Drug Administration for the treatment of schizophrenia (under the trade name Caplyta). New studies suggest that the drug is also effective in bipolar I and bipolar II depression.
Lumateperone modulates the activity of the neurotransmitters dopamine, serotonin, and glutamate. It modulates D1 and D2 dopamine receptors, partially activating presynaptic receptors while partially blocking postsynaptic receptors. Lumateperone acts as an antagonist blocking serotonin 5-HT2A receptors, and it augments activity at both NMDA and AMPA glutamate receptors.
Because of lumateperone’s complex pharmacology, it is not clear which of these activities are primarily responsible for its antidepressant and antipsychotic activities.
New research presented at the 2020 meeting of the International Society for Bipolar Disorders showed that lumateperone reduces bipolar depression.
Researcher Susan Kozauer presented research from a six-week study of 377 patients who were randomized to receive treatment with either 42mg of lumateperone (n=188), taken once daily in the evening, or placebo (n=189). The patients had been diagnosed with bipolar I or II disorder and were experiencing an episode of major depression.
Patients taking lumateperone saw significantly greater improvement in depression than those in the placebo group. Among those taking lumateperone, 60% of those who were markedly ill or worse at baseline improved to mildly ill or better, compared to 43% of those taking placebo.
Researcher Suresh Durgam described improvements in specific symptoms that make up the Montgomery-Åsberg Depression Rating Scale (MADRS) in those patients who received lumateperone. The greatest improvements compared to placebo were in sadness, inner tension, and reduced sleep. By the 29th day of the study, 8 of 10 items on the scale had improved significantly compared to placebo, and all items had improved by day 43.
The side-effects profile of lumateperone was presented by researcher Lakshmi Yatham.
Among those taking lumateperone, 8.5% experienced sleepiness compared to 1.1% of those in the placebo group, while 6.4% of the lumateperone group experienced nausea compared to 2.1% of the placebo group. Most effects were mild or moderate in severity. Changes in weight, metabolic measures, extrapyramidal motor effects, and prolactin were minimal in both the lumateperone group and the placebo group.
Editor’s Note: Lumateperone (Caplyta) joins a list of other atypicals that are efficacious in bipolar depression. These include olanzapine-fluoxetine (Symbyax), quetiapine (Seroquel), lurasidone (Latuda), and cariprazine (Vraylar). Lumateperone is currently only FDA-approved for schizophrenia, but approval for bipolar depression should be rapidly forthcoming based on the data presented at the ISBD meeting.
Bipolar depression used to be an orphan diagnosis, with few efficacious treatments. This is now beginning to change, and treating patients with bipolar disorder using antidepressants designed to treat unipolar depression (for which there is little evidence of efficacy) should begin to recede.
Danish Population-Based Study Identifies New Drug Candidates for Bipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, Lars Kessing of the Psychiatric Center Copenhagen described a study that examined incidence of bipolar disorder among a total of 1,605,365 participants who purchased one of six common medications over a ten-year-period, with the goal of identifying drugs that might be repurposed to prevent or treat bipolar illness. The drugs were non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen), low-dose aspirin, high-dose aspirin, statins, allopurinol, and angiotensin.
Because Denmark has population-based healthcare data, the researchers were able to identify participants who purchased these medications between 2005 and 2015, and could also assess these participants for two outcome measures: 1) whether they had received a diagnosis of mania or bipolar disorder as an inpatient or outpatient at a psychiatric hospital, and 2) a combined measure of whether they had received a diagnosis for mania or bipolar disorder in any setting or initiated lithium use. The data on these participants were compared to a random sample of 30% of the population of Demark.
Kessing and colleagues found that among those with steady use of low-dose aspirin, statins (used to lower blood cholesterol), and angiotensin agents (which can lower blood pressure), there was a significant decreased incidence of mania/bipolar disorder on both outcome measures.
In contrast, among those taking non-aspirin NSAIDs and high-dose aspirin, there was an increased incidence of bipolar disorder. (There were no statistically significant findings with regard to allopurinol, which is used to treat gout and kidney stones.)
The researchers concluded that population-based studies such as these can be used to identify drugs that may have secondary benefits, in this case low-dose aspirin, statins, and angiotensin agents, which have already been identified as potentially therapeutic in other research.
Transcranial Direct Current Stimulation Improved OCD in Controlled Trial
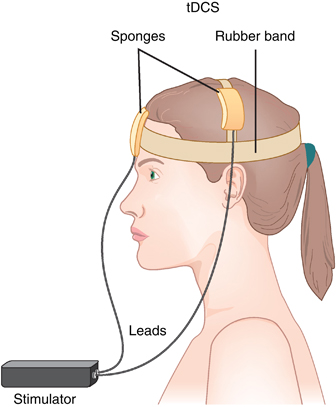
In an abstract of a paper that was to be presented at the 2020 meeting of the Society of Biological Psychiatry in May, researcher Roseli Gedanke Shavitt described a study of transcranial direct current stimulation (tDCS) in people with treatment-resistant obsessive-compulsive disorder (OCD). TDCS is a treatment in which electrodes applied to a patient’s scalp provide a constant low level of electricity that can modulate neuronal activity.
Shavitt and colleagues gave 30 minutes of either active or sham tDCS for 20 days to patients with treatment-resistant OCD. They positioned the cathode over the supplementary motor area of the brain, and the anode over the left deltoid. Those patients who received active tDCS achieved significantly greater reductions in OCD symptoms than did those in the sham group.
New Type of Antipsychotic Drug for Schizophrenia Looks Promising
In a 2020 article in the New England Journal of Medicine, researcher Kenneth S. Koblan and colleagues described a new type of antipsychotic drug treatment for schizophrenia. Almost all other antipsychotic drugs block dopamine D2 receptors, while atypical antipsychotics also block the serotonin 5HT2 receptor. They are described as antagonists at these receptors.
In contrast, the new drug is an agonist or activator of two different receptors. The drug SEP-363856 (also called SEP-856) activates the trace amine–associated receptor 1 (TAAR1) and 5-hydroxytryptamine (or serotonin) type 1A (5-HT1A) receptors.
Blocking D2 receptors can cause Parkinson’s-like symptoms (such as tremor, masked faces, and impaired movement or speech) and other extrapyramidal side effects (such as slurred speech, slow movements, or restless legs.) In contrast, SEP-856 seems to have a better side effects profile than these types of drugs while also being highly effective.
Patients with an acute exacerbation of schizophrenia were assigned to receive either placebo or once-daily treatment with SEP-856 (either 50mg or 75mg) for four weeks. A total of 120 patients received SEP-856 while 125 received placebo.
Compared to the placebo group, the SEP-856 group showed significantly greater reductions on a scale of positive and negative symptoms of schizophrenia by the end of the four weeks. Side effects included some sleepiness and gastrointestinal symptoms, but the incidence of extrapyramidal symptoms and changes in the levels of lipids, glycated hemoglobin, and prolactin were similar in both groups. There was one sudden death from cardiac causes in the SEP-856 group, which was not thought to be drug-related.
Editor’s Note: This drug acting on trace amine–associated receptor 1 (TAAR1) and 5HT1A receptors could herald a new and better tolerated type of antipsychotic. It is also being studied for psychosis in Parkinson’s disease. Since all of the antipsychotics that treat schizophrenia have also shown antimanic efficacy, we look forward to future studies of this unique drug in patients with mania.
AiTBS Superior to ECT in Small Study

Researchers Erica Jensen and Nolan Williams reported in abstracts of a paper that they were to present at the 2020 meeting of the Society of Biological Psychiatry in May that daily sessions of accelerated intermittent theta burst transcranial stimulation (aiTBS) over five or more days produced better results in 15 patients hospitalized for depression and suicidality than in matched patients who received electro-convulsive therapy.
AiTBS is a form of repeated transcranial magnetic stimulation (rTMS), in which a magnetic coil is applied to a patient’s scalp, producing electrical changes in the brain.
The aiTBS treatment was delivered to the left dorsolateral prefrontal cortex. It consisted of 1800 pulses per session, at 80% of a patient’s resting motor threshold with a 50-minute inter-session interval.
The patients in the study were matched (for age, gender, and treatment resistance) to patients who were hospitalized and given ECT. Among patients who received aiTBS and were discharged after an average of 8.4 days, there was an 86% response rate and a 73% remission rate. Among the patients who received ECT, who were discharged after an average of 22.3 days, there was a 53% response rate and a 40% remission rate. With further ECT, response and remission rates increased to 73% and 67%. Time to remission was 3.5 days with aiTBS and 31.3 days for ECT. The investigators concluded conservatively, “Our results suggest that aiTBS could have comparable efficacy to ECT, with potentially faster resolution of acute severe depression.”
Editor’s Note: ECT has been the gold standard treatment for severe depression and suicidality and now we may have a platinum comparator. If these findings are replicated, they could represent a paradigm shift in the treatment of severe depression. Hopefully, this novel form of rTMS will be fast-tracked for approval by the Food and Drug Administration (FDA).
Fish Oil Monotherapy on Depression in Adolescents at High Risk for Bipolar I Disorder: Ambiguity Persists

Researcher Robert K. McNamara and colleagues reported in the Journal of Child and Adolescent Psychopharmacology in a 2020 article that 12 weeks of treatment with omega-3 fatty acids in the form of fish oil did not reduce depression symptoms in adolescents at risk for bipolar disorder when compared to placebo. The primary outcome measured was the results of the Childhood Depression Rating Scale-Revised (CDRS-R).
Fish oil did perform better than placebo on two parts of the rating scale: symptom severity and symptom improvement, especially in weeks 11 and 12 of the study. Omega-3 fatty acids increased creatine and choline in the anterior cingulate, and also increased polyunsaturated fatty acids in red blood cells. The treatment was safe and well-tolerated.
A total of 42 patients between the ages of 9 and 21 who had been diagnosed with depression and had at least one parent with bipolar I disorder received either placebo or 3 fish oil capsules per day. Each capsule contained 450?mg EPA, 40?mg docosapentaenoic acid (DPA), and 260?mg DHA for a total daily dose of 2130?mg EPA + DHA.
Editor’s Note: Ambiguity persists about whether omega-3 fatty acids can improve unipolar or bipolar depression, attention-deficit hyperactivity disorder (ADHD), or prevent the progression of schizophrenia symptoms to the full syndrome. Given the lack of side effects, and the documented effects on red blood cells and brain choline, clinical use of these compounds could be considered in some circumstances.
Gabapentin is Effective in Alcohol Use Disorder in Patients with Alcohol Withdrawal Symptoms

Researcher Raymond F. Anton and colleagues reported in the journal JAMA Internal Medicine that compared with placebo, the anticonvulsant medication gabapentin helped people with alcohol use disorders reduce their drinking or abstain from drinking, especially those who had more withdrawal symptoms before treatment.
Ninety-six participants were randomized to receive either placebo or 1200mg/day of gabapentin for 16 weeks.
In the study, 27% of participants who took gabapentin had no heavy drinking days (compared to 9% among those who took placebo) and 18% achieved total abstinence (compared to 4% among those who took placebo). Gabapentin was most effective in those with a history of alcohol withdrawal symptoms. An impressive 41% of participants with high alcohol withdrawal symptoms who took gabapentin achieved total abstinence compared with 1% of participants in the placebo group.
Gabapentin, which is used to treat epilepsy, influences GABA and glutamate transmitters and inhibits the alpha 2gamma-1 voltage sensitive calcium channel, which is upregulated in chronic alcohol exposure.
Better One-Year Clinical Outcomes After Four Weeks of Theta Burst Stimulation for PTSD Than After Two Weeks

In a 2019 article in the journal Neuropsychopharmacology, Nicholas J. Petrosino and colleagues described findings from one year of follow-up with veterans suffering from post-traumatic stress disorder (PTSD) who received intermittent theta burst transcranial magnetic stimulation (iTBS) in a four-week crossover study.
In the first two weeks of the study, half of the 50 participants (who were mostly male and had an average age of 51) received iTBS while the others were given a sham procedure. Then all the participants received iTBS on an open (non-blind) basis for two more weeks.
At one month, those who had received four total weeks of iTBS had better outcomes than those who had received only two weeks of active iTBS. These results were published in the American Journal of Psychiatry in 2019 in an article by Noah S. Philip and colleagues.
The researchers went on to look at longer-term outcomes, namely time until relapse (a major event such as a re-hospitalization or suicide). After one year, those who received four weeks of iTBS went 9 to 11 months without relapsing (296.0 days ± 22.1), while those who received only two weeks of iTBS went 5 to 7 months before relapsing (182.0 days ± 31.9).
It seems that more iTBS may be better than less iTBS for PTSD in both the short and long term.


