Early Cannabis Use and BDNF Gene Variant Increase Psychosis Risk
 Normal variations in genes can affect risk of mental illness. One gene that has been implicated in psychosis risk is known as BDNF. It controls production of brain-derived neurotrophic factor, a protein that protects neurons and is important for learning and memory. Another important gene is COMT, which controls production of the enzyme catechol-O-methyltransferase, which breaks down neurotransmitters such as dopamine in the brain.
Normal variations in genes can affect risk of mental illness. One gene that has been implicated in psychosis risk is known as BDNF. It controls production of brain-derived neurotrophic factor, a protein that protects neurons and is important for learning and memory. Another important gene is COMT, which controls production of the enzyme catechol-O-methyltransferase, which breaks down neurotransmitters such as dopamine in the brain.
Several forms of these genes appear in the population. These normal variations in genes are known as polymorphisms. Certain polymorphisms have been linked to disease risk. A study by Anna Mané and colleagues published in the Journal of Psychiatric Research in 2017 explored links between COMT and BDNF polymorphisms, cannabis use, and age at first episode of psychosis.
Mané and colleagues found that among 260 Caucasians being treated for a first episode of psychosis, the presence of a BDNF polymorphism known as val-66-met and a history of early cannabis use were associated with younger age at psychosis onset.
The val-66-met version of BDNF occurs in 25-35% of the population. It functions less efficiently than a version called val-66-val.
The researchers also found that males were more likely to have used cannabis at a young age.
Editor’s Note: In the general population, marijuana use doubles the risk of developing psychosis. Previous data had indicated that the risk was higher for those with a COMT polymorphism known as val-158-val that leads to more efficient metabolism of dopamine in the prefrontal cortex. The resulting deficits in dopamine increase vulnerability to psychosis compared to people with the val-158-met version of the COMT gene.
The new study by Mané and colleagues suggests that a common form of BDNF may be associated with an earlier onset of psychosis. Bottom line: Pot is dangerous for young users and can induce psychosis, particularly in people at genetic risk. Pot may be legal in many places, but heavy use in young people remains risky for mental health and cognitive functioning.
The company Genomind offers genetic testing for BDNF and COMT variants as part of a routine panel.
Cannabis Use May Cause Schizophrenia
 Cannabis use has been linked to schizophrenia risk, and new genetic research suggests a causal relationship between the two. In a 2017 article in the journal Molecular Psychiatry, researcher Julian Vaucher and colleagues reported that lifetime cannabis use was linked to schizophrenia even when the researchers controlled for 10 genotypes weakly associated with lifetime cannabis use. This makes it unlikely that the schizophrenia caused the cannabis use, suggesting instead that it is the cannabis use that leads to a schizophrenia diagnosis.
Cannabis use has been linked to schizophrenia risk, and new genetic research suggests a causal relationship between the two. In a 2017 article in the journal Molecular Psychiatry, researcher Julian Vaucher and colleagues reported that lifetime cannabis use was linked to schizophrenia even when the researchers controlled for 10 genotypes weakly associated with lifetime cannabis use. This makes it unlikely that the schizophrenia caused the cannabis use, suggesting instead that it is the cannabis use that leads to a schizophrenia diagnosis.
Vaucher and colleageus also controlled for genetic associations between cigarette smoking and cannabis use to eliminate cigarette use as a third variable causing the association between cannabis and schizophrenia.
The study by Vaucher and colleagues included 34,241 people with schizophrenia and 45,604 healthy controls.
In Population Near Uranium Plant, Headaches Predicted a Thyroid Problem
People with headache disorders may be at greater risk of developing hypothyroidism, a condition in which the thyroid does not produce enough thyroid hormone and various body processes start to slow down. A study by researcher Andrew Martin and colleagues in the Journal of Head and Face Pain is the largest to examine the likelihood that headache sufferers may be at risk for hypothyroidism.
About 2% of Americans develop hypothyroidism. The study by Martin and colleagues used data from a 20-year medical monitoring program for people who lived near a uranium processing plant in Ohio. The authors reported that people with pre-existing headache disorders had a 21% increased risk of new onset hypothyroidism during that period, while people who reported that they had migraines or regularly used headache medication had a 41% increased risk of hypothyroidism. People with migraines were most likely to develop hypothyroidism in the study. Female sex and age are additional risk factors for hypothyroidism. About 12% of the US population experiences migraines.
More News About Genetic Risk for Bipolar Disorder
In a 2017 article in the Journal of Clinical Psychiatry, researcher Paul E. Croarkin and colleagues describe findings from their study of genetic risk factors for early-onset bipolar disorder. The researchers focused on single nucleotide polymorphisms (SNPs), which are variations in a single base pair of a DNA sequence. SNPs are normal variations or copying errors that occur when DNA is replicated. Croarkin and colleagues tracked 8 SNPs that had been linked to bipolar disorder in previous studies. They examined 69 patients from a study of early-onset mania, 732 adult patients with bipolar disorder (including 192 with early-onset illness), and 776 healthy controls. The researchers compared patients with early-onset illness to controls, and also looked for connections between specific SNPs and early-onset illness.
The SNPs analyzed in the study map to three genes that have repeatedly been associated with the risk for bipolar disorder in other studies. These include CACNA1C (one of several genes that create calcium channels), ANK3, and ODZ4. Croarkin and colleagues determined that the presence of these SNPs, particularly the ones that involved the CACNA1C gene, were associated with early-onset bipolar disorder.
Editor’s Note: These findings may lead to better treatment for early-onset bipolar disorder. The CACNA1C calcium influx gene that has repeatedly been connected to bipolar illness can be blocked by the calcium channel blocker nimodipine. Nimodipine has lithium-like effects in mania and depression in adults. One case report by Pablo A. Davanzo in the Journal of Child and Adolescent Psychopharmacology described success using nimodipine and the thyroid medication levothyroxine to treat a 13-year-old boy with very rapid cycling bipolar disorder that had previously failed to respond to multiple medications.
Nimodipine deserves further study in children showing symptoms of bipolar disorder. The company Genomind provides testing for the CACNA1C gene. We hope it will soon be determined whether the presence of this SNP predicts a good response to nimodipine.
Being able to predict who will get bipolar disorder is a long way off. However, there are some clear risk factors. Young people from families that have had several generations of bipolar disorder or related disorders are at increased risk for bipolar disorder. This risk increases for children who experience adversity in childhood, such as abuse or neglect. The presence of early mild symptoms of mania, depression, or disruptive behavior further increase this risk.
For doctors, a patient’s clinical history of these three types of risk factors can help identify whether they are at increased risk of developing bipolar disorder. Patients with several risk factors should be observed closely and treated with psychotherapy or medication as needed.
Parents of children between the ages of 2 and 12 who have shown some signs of mood or behavioral symptoms are encouraged to join our Child Network. We provide a secure online platform where parents record their children’s symptoms of anxiety, depression, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania on a weekly basis. Symptoms are charted over time in a graphical depiction that can be shared with the child’s doctor. For more information, see page 11 of this issue. To join, visit our website bipolarnews.org and click on the tab for the Child Network.
Parents’ History of Mood and Anxiety Disorders Increases Risk of These Disorders in Offspring
A 2016 article by researcher Petra J. Havinga and colleagues in the Journal of Clinical Psychiatry suggests that offspring of a parent with a mood or anxiety disorder are at higher risk for these disorders than offspring from non-ill parents. Havinga and colleagues studied 523 offspring of parents with one of these disorders. Among these offspring, 38.0% had had a mood or anxiety disorder by age 20, and 64.7% had had such a disorder by age 35. (Rates of these disorders in the general population are closer to 10%.)
The risk of offspring developing one of these disorders was even higher when both parents had a history of a mood or anxiety disorder, when a parent had an early onset of one of these illnesses, and when the offspring was female. The good news is that balanced family functioning had a protective effect, reducing the likelihood that the offspring would develop a mood or anxiety disorder.
Researcher David Axelson reported in a 2015 study published in the American Journal of Psychiatry that approximately 74% of the offspring of a parent with bipolar disorder went on to have a major psychiatric diagnosis over 6.7 years of followup. Similarly, researcher Myrna Weissman and colleagues reported in 2006 that the same high incidence of psychiatric diagnoses was true of the offspring of a parent with unipolar depression over 20 years of followup.
Editor’s Note: It is important to be vigilant for mood or behavioral disorders that may emerge in the offspring of a parent with a mood or anxiety disorder. Children at high risk should maintain a healthy diet and good sleep hygiene, exercise regularly, and perhaps try practicing mindfulness and meditation, as recommended by researcher Jim Hudziak. Family-focused therapy (developed by researcher David Miklowitz) can help when early symptoms appear in the offspring of a parent with bipolar disorder.
Another option is joining our Child Network, a secure online program that allows parents to track their children’s symptoms of anxiety, depression, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania. This may facilitate earlier recognition and treatment of dysfunctional symptoms, which can be treated with psychotherapy and medication.
Recent Birth Cohorts May Have More Depression and Bipolar Disorder
In medicine, the ‘cohort effect’ describes the idea that more recent birth cohorts have an increased incidence and younger age of onset of their illness. A 2016 article by this editor (Robert M. Post) and colleagues in the Journal of Clinical Psychiatry presented evidence that younger patients with bipolar disorder have an earlier age of onset of bipolar disorder and more relatives with mood disorders than older patients with bipolar disorder.
The research was carried out by the Bipolar Collaborative Network in four US cities (Dallas, Cincinatti, Los Angeles, and Bethesda) and three northern European ones (Utrecht, Freiburg, and Munich). On both continents, patients born more recently had an earlier age of onset of their bipolar disorder. Younger patients also had parents and grandparents with a greater incidence of depression, bipolar disorder, and alcohol and substance abuse compared to older patients.
Editor’s Note: Other researchers have found evidence of a cohort effect for unipolar depression, substance abuse, and attention-deficit hyperactivity disorder (ADHD). The data indicate that childhood onset of psychiatric illnesses may be becoming more common. Research aimed at earlier detection and treatment is needed to reverse these trends.
Inflammation Predicts Depression and Anxiety Four Years Later in Older Americans
A large study of retired Americans found that those with high levels of the inflammatory marker C-reactive protein in the blood had more depression and anxiety. Higher CRP also predicted severity of depression and anxiety four years later.
The study, by researchers Joy E. Lin and Aoife O’Donovan, included 18,603 people over age 50 from the Health and Retirement Study. It was presented at the 2016 meeting of the Society of Biological Psychiatry.
Lin and O’Donovan hope that treating or preventing inflammation may be the key to preventing symptoms of depression and anxiety.
Meta-Analysis Shows Inflammation is Common in Unipolar Depression, Bipolar Depression, and Schizophrenia
In a symposium at the 2016 meeting of the Society of Biological Psychiatry, Mark Hyman Rapaport described the results of his research group’s meta-analysis of studies comparing levels of inflammation in the blood of people with unipolar depression, bipolar depression, and schizophrenia. Rapaport and colleagues determined that people acutely ill with any of the three illnesses showed abnormally high levels of certain inflammatory proteins. These included: interleukin-1beta, interleukin-6, TNF alpha, and c-reactive protein. Those who were chronically ill showed elevations in interleukin-6.
These data are consistent with increasing evidence that inflammation also occurs in the brain. Brain inflammation can be observed by measuring translocator protein binding, a measure of brain microglial activation, using positron emission tomography (PET) scans.
Fluctuations in White Matter in Adolescents with Bipolar Disorder May Indicate Cardiovascular Risk
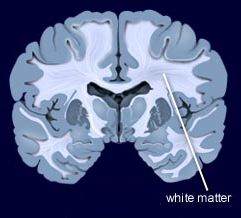 During functional magnetic resonance imaging (fMRI) of the brain, data on physiological fluctuations in white matter are collected. These fluctuations are caused by cardiac pulses, cerebrovascular dysfunction, and other factors. Increasing fluctuations have been linked to cognitive impairment with age.
During functional magnetic resonance imaging (fMRI) of the brain, data on physiological fluctuations in white matter are collected. These fluctuations are caused by cardiac pulses, cerebrovascular dysfunction, and other factors. Increasing fluctuations have been linked to cognitive impairment with age.
Vascular problems in adults with bipolar disorder have been linked to cerebrovascular disease, a group of conditions that affect bloodflow to the brain. In a recent study, researcher Arron W. S. Metcalfe and colleagues used data on physiological fluctuations in white matter (usually a nuisance variable) to assess the vascular health of teens with bipolar disorder. Compared to 32 age-, IQ-, and sex-matched controls, 32 adolescents with bipolar disorder had more fluctuations in white matter in three different clusters in the brain.
These white matter fluctuations are a possible early indicator of susceptibility to cerebrovascular disease in teens with bipolar disorder. Patients with depression and bipolar disorder are at increased risk for cardiovascular disease, so maintaining a good diet, exercising regularly, and assessing blood pressure, cholesterol, and lipid levels is recommended. See page __ where we describe research showing teens with bipolar disorder have stiffer artery walls.
Teens with Bipolar Disorder Have More Inflammation, Cardiovascular Risks
 Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Hatch and colleagues assessed the blood of 60 teens with bipolar I or II disorder and 20 healthy controls for a variety of biomarkers, including the inflammatory proteins interleukin 6, interleukin 10, and TNF alpha; VEGF, which is responsible for the production of new blood vessels; and brain-derived neurotrophic factor (BDNF), which protects neurons. The researchers also assessed the participants’ cardiovascular health, performing the carotid intima media thickness test to estimate how much plaque is in the arteries, and measuring how well the patients’ arteries dilate in response to changes in bloodflow.
Participants with bipolar disorder had higher levels of interleukin 6 than healthy controls, regardless of whether their bipolar illness was symptomatic. Low BDNF was linked to greater carotid intima thickness in participants with symptomatic bipolar disorder, and vascular measurements suggest a possible mechanism by which bipolar disorder increases cardiovascular risk.