Children of Bipolar Parents Are At Risk for Depression and Bipolar Disorder
The Pittsburgh Bipolar Offspring study, led by Boris Birmaher of the University of Pittsburgh, investigated risk of illness in the offspring of parents with bipolar disorder. The study included 233 parents with bipolar disorder and 143 controls. In addition to bipolar disorder, parents in the study had many other disorders, including anxiety (70%), panic (40%), a disruptive behavior disorder (35%), attention-deficit hyperactivity disorder or ADHD (25%), and substance use disorder (35%).
The offspring averaged age 12 at entry in the study. Offspring of parents with bipolar disorder had more illness than those of control parents, including bipolar spectrum disorders (10.6% versus 0.8%), depression (10.6% versus 3.6%), anxiety disorder (25.8% versus 10.8%), oppositional defiant disorder or conduct disorder (19.1% versus 8.0%), and ADHD (24.5% versus 6.7%). Of these differences, only bipolar spectrum disorders and anxiety were statistically significant after correcting for differences in the parents’ other diagnoses.
Two factors predicted bipolar spectrum disorders in the offspring: younger age of a parent at birth of child and bipolar disorder in both parents. Older children and those with diagnoses of anxiety or oppositional defiant disorder were more likely to be diagnosed with bipolar disorder.
On long-term follow-up that continued on average until the offspring reached age 20, 23% of those participants who had a parent with bipolar disorder developed any type of bipolar disorder, versus only 1.2% of the children of controls. Of these 23%, about two-thirds had a depressive episode prior to the onset of their bipolar disorder.
Of the offspring of parents with bipolar disorder who developed a bipolar spectrum illness, 12.3% developed bipolar I or II disorders, while 10.7% were diagnosed with bipolar not otherwise specified (NOS). Of those with bipolar NOS, which some consider to be sub-threshold bipolar disorder, about 45% converted to a bipolar I or II diagnosis after several years of prospective follow-up. These data, along with the finding that children with bipolar NOS are highly impaired and take more than a year on average to remit, stress the importance of vigorously treating this subtype, even if it does not meet the full threshold for bipolar I or bipolar II.
Birmaher indicated that although about 50% of the offspring of a bipolar patient had no diagnosis, the high incidence of multiple psychiatric difficulties developing over childhood and adolescence spoke to the importance of attempts at early intervention and prevention. Studies of effective treatment and prevention strategies are desperately needed. So far only family focused therapy (FFT), an intervention developed by researcher David Miklowitz, has shown significant benefits over standard treatment in children with a positive family history of bipolar disorder who already have a diagnosis of anxiety, depression, or bipolar not otherwise specified.
Marijuana Addiction Associated with White Matter Loss and Brain Changes in Healthy People and Those with Schizophrenia
It has been established that cannabis use is associated with impairments in working memory, but researchers are still investigating how these impairments come about. A 2013 study by Matthew J. Smith et al. in the journal Schizophrenia Bulletin compared regular marijuana users both with and without schizophrenia with demographically similar people who did not use marijuana.
Using magnetic resonance imaging (MRI), the researchers were able to map each participant’s brain structures. Healthy people who were marijuana users showed deficits in white matter (axons of neurons that are wrapped in myelin) compared to healthy people who did not use the drug. Similarly, patients with schizophrenia who used marijuana regularly had less white matter than those patients with schizophrenia who did not use the drug. There were also differences in the shapes of brain structures, including the striatum, the globus pallidus, and the thalamus, between cannabis users and non-users.
Differences in the thalamus and striatum were linked to white matter deficits and to younger age of cannabis use disorder onset.
Differences between cannabis users and non-users were more dramatic across the populations with schizophrenia than across the healthy populations.
Editors note: Future research is needed to determine whether marijuana causes these brain changes, or whether the brain changes are a biomarker that shows a vulnerability to marijuana addiction (although the latter is less likely than the former).
Other data show that marijuana is associated with an increase in psychosis (with heavy use), cognitive deficits, and an earlier onset of both bipolar disorder and schizophrenia in users compared to non-users. These findings make pot begin to look like a real health hazard. With legalization of marijuana occurring in many states, ease of access will increase, possibly accompanied by more heavy use. The most consistent pharmacological effect of marijuana is to produce an amotivational syndrome, characterized by apathy or lack of interest in social activities. Particularly for those already struggling with depression, pot is not as benign a substance as it is often thought to be.
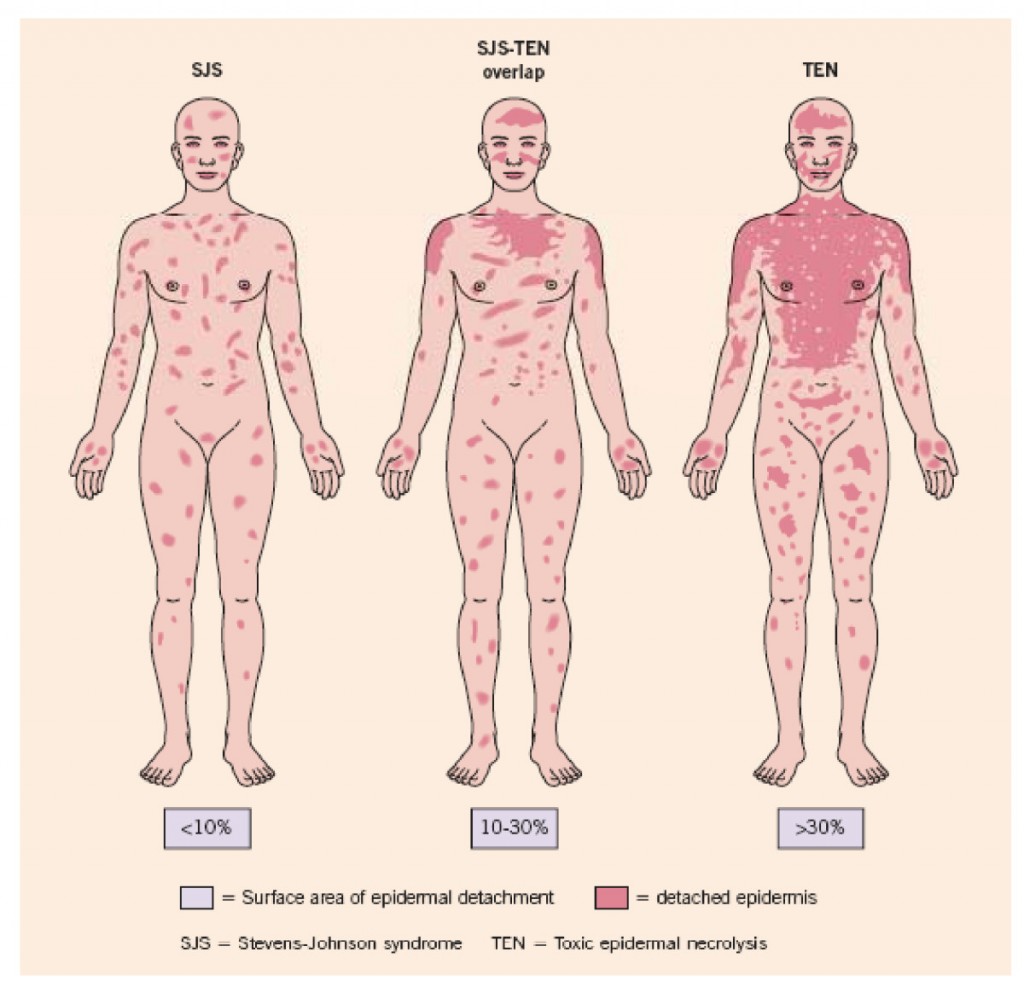
Genetic Test Predicts Risk of Severe Rash While Taking Carbamazepine
Carbamazepine (also known by its trade name Tegretol or, for extended release, Equetro) is one of the most widely used drugs for the treatment of epilepsy, and is relatively underutilized in the treatment of bipolar disorder. One of the reasons is fear of a rare serious rash or other side effects.
The risk of the serious rash ranges from about one in 5,000 to one in 10,000. Loss of white blood cells that fight infection (a condition called agranulocytosis) occurs in about one in 20,000 people taking carbamazepine, while a decrease in white blood cells, red blood cells, and platelets (aplastic anemia) occurs in about one in 100,000 patients.
There is no way of predicting who will develop the blood disorders in reaction to carbamazepine use. A patient should contact their doctor and get a white blood cell count if they develop some warning signs of these conditions, such as a fever or sore throat without other explanation or signs of bleeding or red spots under the skin (called petechiae) that could indicate low platelets.
Genetic Test for Risk of Rash
A genetic test is available that can help estimate the likelihood of the serious rash among certain populations. In those of Asian descent, particularly Han Chinese, Thai, Malaysian, and Indian populations, having a version of the gene HLA-B known as HLA-B*1502 is highly associated with developing the rash. (The odds ratio was 79.84 in a 2013 meta-analysis by Tangamornsuksan et al. in the journal JAMA Dermatology).
In those of northern European or Japanese descent, having a version of the gene HLA-A known as HLA-A*3101 is associated with the severe rash. (Odds ratio for developing the most severe rash was 25.93 in a study of Europeans published by McCormack et al. in the New England Journal of Medicine in 2011 and 10.8 in a study of Japanese published by Ozeki et al. in the journal Human Molecular Genetics in 2011). This HLA-A*3101 gene is present in about 2 to 5% of Europeans and 9% of Japanese.
A mild, non-serious rash with redness and itchiness occurs in about 5 to 10% of patients taking carbamazepine, and almost always goes away quickly upon stopping the drug. For patients taking carbamazepine who develop any rash, stopping the drug is the safest and most conservative thing to do. However, those who have taken the HLA test who know they do not have the risk genes and have only the benign rash might want to consider continuing to take the drug.
Benefits of Carbamazepine
There are a number of reasons why carbamazepine may be worthy of a treatment trial in patients with bipolar disorder who are not doing well on other agents. Carbamazepine works well in many patients with bipolar illness who have some of the common clinical predictors of a poor response to lithium. These include: having dysphoric (anxious, irritable) rather than euphoric mania, having an anxiety or substance disorder comorbidity, having had many prior episodes or rapid cycling (four or more episodes/year), not having distinct episodes with a period of wellness in between, having a sequential pattern of depression followed by mania followed by a well interval (D-M-I rather than M-D-I), having a schizoaffective disorder with delusions or hallucinations that persist after a manic or depressive episode has ended, and having no family history of mood disorders (especially bipolar disorder).
Some patients who do not respond to another anticonvulsant such as valproate do respond to carbamazepine. Patients with bipolar depression who have had a prior history of alcoholism may also do particularly well on carbamazepine. A benefit of the long-acting version of carbamazepine called Equetro is that it can be taken at bedtime and thus help with sleep and minimize daytime side effects.
Editor’s Note: Carbamazepine induces liver enzymes called CYP3A4 that increase the metabolism (breakdown) of carbamazepine and other drugs. Several drugs that inhibit 3A4 (such verapamil and erythromycin) prevent the breakdown of carbamazepine, causing blood levels of the drug to increase and produce side effects. If you are taking carbamazepine, tell your pharmacist so he or she can monitor any other drugs you are taking for potential interactions with carbamazepine.
Knowing about the rare skin and blood side effects of carbamazepine and some of the clinical predictors of a good response to the drug may be helpful in determining whether the potential benefits of carbamazepine outweigh the risks.
Immune Response in Mania
While the reasons why one person develops bipolar disorder and another does not remain mysterious, the current thinking is that genes contribute some risk while immunological abnormalities contribute other risks. Researchers have identified certain antibodies whose levels spike during an episode of mania, as if the patient is having an immune reaction. These are referred to as biomarkers or inflammatory markers.
While various biomarkers for mania have been identified, until recently their effects had only been examined independently. A 2013 article by Dickerson et al. published in the journal PLOS ONE examined four biomarkers in combination. Each was a type of antibody: to the NR peptide of the NMDA receptor, to gliadin (a protein derived from gluten), to Toxoplasma gondii (a parasitic protozoan), and to Mason-Pfizer Monkey Virus. Measures of these four types of antibodies made up a combined inflammation score for participants in the study.
The study compared 57 patients presenting with a manic episode with 207 non-psychiatric controls and 330 patients who had had recent onset of psychosis, schizophrenia, or bipolar depression. The combined inflammation score of the mania group was significantly higher than the other groups at the time of hospital admission and at the time of evaluation several days later. It had returned to normal (i.e. not different from the other groups) at followup six months later, although those with the highest combined inflammation scores were at risk for re-hospitalization during that period.
The findings of this study suggest that hospitalization for mania is associated with immune activation, and the level of this activation predicts subsequent re-hospitalization. Treatments for mania that target this inflammatory response should be investigated.
Diabetes Drug Metformin May Impair Cognition, But Vitamin B12 May Help
Metformin, one of the most popular drugs to treat type 2 diabetes, interferes with uptake of vitamin B12, which can in turn lead to some neuronal dysfunction resulting in cognitive dysfunction. Several studies have sought to clarify this link, which may affect up to 30% of patients taking the drug.
Most recently, an Australian analysis of 1354 aging patients found that those with type 2 diabetes performed less well on tests of cognitive abilities, and those diabetic patients with low vitamin B12 levels (below 250 pmol/L) scored lower than those diabetic patients with adequate levels.
Because of the malabsorption problem caused by metformin, patients taking the drug may not be able to get enough B12 from a balanced diet alone and may need supplemental B12. Those who follow a vegetarian diet, have had bowel surgery, have certain complications with the stomach, or who take other medications that depress stomach acid may be at special risk.
Physicians should carefully monitor B12 levels in patients taking metformin, particularly those who have been taking the drug for more than 3 years or those who already suffer from some sort of cognitive impairment.
Low Omega-3s in Children Associated with Poor Cognitive Performance
Omega-3 fatty acids (especially the type known as DHA) are essential for brain development and functioning, but most people eating a modern western diet consume low amounts of these compared to omega-6 fatty acids. Omega-3s are anti-inflammatory while omega-6s are pro-inflammatory. A large UK study published in the journal PLOS One in 2013 reported that healthy 7- to 9-year-olds with lower levels of omega-3 long-chain polyunsaturated fatty acids in their blood (including DHA, DPA, and EPA) had lower reading ability and working memory, and also had more behavior problems.
The oils in fish are the best source of omega-3 fatty acids, and most of the children with poor reading ability in the study fell short of the UK nutritional guideline that recommends eating two portions of fish per week.
Girls in the study had more dramatic deficits in omega-3 levels than boys. In adults, women tend to metabolize long chain polyunsaturated fatty acids more easily than men, but this difference is driven by hormones, and because the girls in the study had not yet reached child-bearing age, they did not reflect this benefit.
Omega-3 deficits in children have been connected with attention deficit hyperactivity disorder (ADHD), and supplementation with extra omega-3 fatty acids in the diet has led to improvements in ADHD.
Fatty Acids in Mood Disorders
Cultures where more omega-3 fatty acids (which have anti-inflammatory effects) and fewer omega-6 fatty acids (which have pro-inflammatory effects) are consumed have a lower incidence of depression and bipolar disorder. However, the exact role that each kind of fatty acid plays in the brain and whether dietary changes can improve mood disorders is still being investigated. A 2012 study in the Journal of Psychiatric Research examined the complete lipid profiles of participants with bipolar disorder to collect data on these questions.
The most significant results to come from the study were that levels of the long-chain omega-6 fatty acid dihomo-gamma-linolenic acid (DGLA) were positively correlated with neuroticism, depression severity, and decreased functioning. Depression severity was negatively correlated with the omega-6 fatty acid linolenic acid (LA) and the omega-3 fatty acid alpha-linolenic acid (ALA), and positively correlated with fatty acid desaturase 2 (FADS2), an enzyme that converts LA to the omega-6 fatty acid gamma-linolenic acid GLA.
The data suggest that particular omega-6 fatty acids and the enzymes that lead to their production may be used as biomarkers that can indicate depression.
Editor’s Note: Levels of specific omega-6 fatty acids and their related enzymes were found to correlate with depression severity in this study. Since omega-6 fatty acids are pro-inflammatory, diets higher in omega-6 fatty acids are associated with more cardiovascular problems, and a 2012 article by Chang et al. in the Journal of Psychiatric Research reported that completed suicides in bipolar patients with cardiovascular disorders were significantly higher than in those with bipolar disorder without cardiovascular illness, it seems a healthy diet can have multiple benefits, including potentially reducing depressive burden, cardiovascular risk, and suicide risk.
Iron Deficiency Linked to Psychiatric Disorders in Children
Iron deficiency is the most prevalent nutritional deficiency in industrialized countries and can cause problems with cognitive and intellectual development. New research published in the journal BMC Psychiatry shows that it has psychiatric ramifications as well. Children and adolescents with iron deficiency anemia are at greater risk for psychiatric disorders, including depression, bipolar disorder, anxiety, and autism.
Iron supplementation should be implemented in children with iron deficiency anemia in order to prevent any possible psychiatric repercussions, and similarly, psychiatrists should check iron levels in young patients with psychiatric disorders.
Iron provides myelin for white matter in the brain and plays a role in the function of neurotransmitters.
Lithium Increases Parathormone and Reduces Vitamin D Levels
Lithium treatment is associated with a moderate incidence of hyperparathyroidism, usually observed as an elevated concentration of calcium in the blood in addition to elevated parathormone levels, and often associated with the development of a tumor (adenoma) of the parathyroid gland.
In a recent study by Van Melick et al. published in the International Journal of Geriatric Psychiatry, among 111 patients with an average age of 75 years, 24-hour calcium excretion was elevated in only 3% of the patients, but levels of parathormone were elevated in 48%. Duration of lithium treatment was associated with lower vitamin 25OH D. Vitamin D is important for healthy bones and good cognitive functioning.
Editor’s Note: Lithium-induced hyperparathyroid should be investigated in those with elevated calcium levels, and if found, surgical removal of the parathyroid gland may be indicated. Low vitamin D is common in the US population. It is also particularly low in patients with mania and elderly patients on who have been on lithium for more than ten years. (Levels are below normal in 77% of these elderly individuals.) Assessment of vitamin D levels in those on long-term lithium is advisable, in addition to monitoring the thyroid, kidney function, and calcium metabolism.
Inflammatory and Metabolic Abnormalities Predict Poor Response to Antidepressants
 There is mounting evidence that inflammation and metabolic problems are related to depression. A recent study by Vogelzangs et al. in the journal Neuropsychopharmacology examined 313 patients being treated for depression to see whether levels of inflammatory markers in the blood and metabolic factors such as cholesterol, blood pressure, and waist circumference predicted whether those patients would still (or again) be diagnosable with depression two years later.
There is mounting evidence that inflammation and metabolic problems are related to depression. A recent study by Vogelzangs et al. in the journal Neuropsychopharmacology examined 313 patients being treated for depression to see whether levels of inflammatory markers in the blood and metabolic factors such as cholesterol, blood pressure, and waist circumference predicted whether those patients would still (or again) be diagnosable with depression two years later.
Several factors predicted later depression, including high levels of the inflammatory marker interleukin-6, low HDL (“good”) cholesterol, higher than normal triglycerides, and high blood glucose (hyperglycemia).
People who had four or more types of inflammatory or metabolic abnormalities had almost twice the odds of having chronic depression. Among those study participants who had only recently begun taking antidepressant medication, having four or more of these risk factors made them almost 7 times more likely to be depressed during follow-up.
One explanation for the connection between inflammatory and metabolic dysregulation and depression is that inflammation and metabolic problems worsen and complicate a patient’s depression and reduce the patient’s responsiveness to traditional antidepressants. Alternative ways of treating these patients aimed at their inflammation and metabolism may be necessary.