American Academy of Pediatrics Recommends Parents Avoid Spanking and Verbal Abuse
The American Academy of Pediatrics (AAP) has issued a policy statement calling for an end to corporal punishment, including spanking. These forms of punishment are tied to negative outcomes in every developmental area.
Children spanked regularly at age 3 had increased aggression risk by age 5. They also had more negative behaviors and lower vocabulary scores at age 9. Abusive behavior raises stress hormones and is associated with mental health struggles.
Verbal abuse should also be avoided. Verbal abuse includes punishment that shames, humiliates, threatens, frightens, or ridicules a child. Use of time outs, removal of privileges, and other forms of quiet discipline are recommended alternatives.
Editor’s Note: In our research network, the Bipolar Collaborative Network, we found that verbal abuse by itself (without the physical or sexual abuse that often accompany it) is associated with an earlier age of onset of bipolar disorder and a more difficult course of illness.
Family focused therapy (FFT) and other forms of family therapy are highly recommended for children of a parent with bipolar illness. These children are at high risk for a variety of psychiatric diagnoses, and those already experiencing depression, cyclothymia (mood swings between high and low) or a diagnosis of bipolar disorder not otherwise specified (BP-NOS) are much improved with FFT compared to treatment as usual. FFT teaches family members to recognize symptoms of illness for what they are rather than interpreting them as deliberate hostility, increases family communication and problem solving, and leads to good long-term outcomes.
Civil War Data Shows Father’s Trauma Can Affect Son’s Lifespan
An economist at the University of California Los Angeles (UCLA) has used Civil War data to determine that trauma experienced by a father can affect the lifespan of his son, but that a mother’s healthy diet during pregnancy can neutralize this risk.
Researcher Dora Costa used records from the National Archive to identify Union soldiers who were held as prisoners of war (POWs) by the Confederacy. She compared records of their children’s lifespans to the children of Union soldiers who were never held as POWs, finding that the sons of POWs were more likely to have died at any given age. (The study included only children who lived to be at least 45 years old.) Detailed records were kept because families of soldiers and POWs were eligible for generous pensions.
When looking at the data, Costa expected to find that socioeconomic status was the factor that explained discrepancies in lifespans among children of Civil War veterans. However, she noticed that the difference in lifespan only appeared in sons, and only to sons born after the war.
This pointed to an epigenetic explanation. Epigenetics is the idea that some aspects of a parent’s experiences (such as deprivation, drug use, etc.) can be passed on to their children during the gene transcription process. While a parent’s inherited genetic sequence doesn’t change, the structure of their DNA can be wound tightly or loosely depending on life experiences, and this affects how easily their genes are transcribed when passed on to their children.
The sons of POWs in the worst camp environments (typically during the later years of the war when prisoner exchanges were less frequent and overcrowding and malnutrition were common in camps) had even shorter lifespans than the sons of POWs who were imprisoned in less dire circumstances.
The research also looked at birth months to determine whether mothers would have had access to good nutrition while pregnant. Sons born to POW fathers in the later months of the year (whose mothers were likely to have had access to good nutrition) had lifespans comparable to the sons of non-POWs, while sons of POWs born earlier in the year fared worse.
The research was published in the journal Proceedings of National Academy of Sciences in 2018.
Editor’s Note: This is another example in humans of findings that have been clear-cut in animal studies. A father’s experiences, such as stressors or substance abuse, can influence the next generation even if the parent has no contact with the offspring. Epigenetic marks on DNA, histones (the structures around which DNA is wound), or microRNA of the sperm appear to carry these unexpected transgenerational effects.
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.
Inflammatory Marker IL-6 is Elevated in People with Depression and Those with a History of Childhood Trauma
In a 2018 article in the journal Psychiatry Research, researcher Ana Munjiza and colleagues reported that the inflammatory marker IL-6 was higher in 64 depressed people than in 53 non-depressed people, and that levels of IL-6 among people in the depressed group were significantly correlated with scores on a questionnaire in which participants reported traumas experienced in childhood. They reported more physical abuse, physical neglect, and emotional abuse.
Munjiza and colleagues indicate that trauma in childhood is a risk factor for depression in adulthood, as other researchers have suggested, and that inflammation could mediate the relationship between childhood adversity and depression.
Editor’s Note: IL-6 has been associated with antidepressant treatment resistance. IL-6 is secreted from white cells in the blood and from monocytes from the bone marrow in response to stress. It enters the brain and starts an inflammatory cascade that induces depressive behaviors. Animal studies have shown that if IL-6 secretion is blocked, depressive-like behaviors do not occur.
Another indicator of inflammation is CRP, and elevations in CRP have been associated with poor response to selective serotonin reuptake inhibitor (SSRI) antidepressants, and better response to the noradrenergic tricyclic antidepressant nortriptyline and the dopamine active antidepressant bupropion.
Treatments for depressed people with histories of childhood trauma may include psychotherapy, somatic therapies such as repeated transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), and medication. More research is needed to determine the optimal treatment regimens for this subgroup of depression sufferers, including whether anti-inflammatory drugs could play a helpful role in preventing or treating depression. People with elevated inflammatory markers (such as IL-6, CRP, IL-1, or TNF-alpha) are likely to be better candidates for adjunctive anti-inflammatory treatments than those with normal or low baseline levels of inflammation.
Using Light to Improve Sleep and Depression
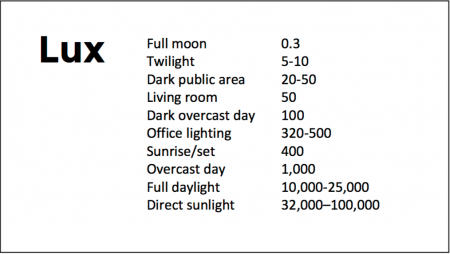
At the 2018 meeting of the North Carolina Psychiatric Association, researcher Chris Aiken described the phenomenon of sleep inertia, when people are awakened from deep sleep by an alarm, rather than waking at the end of a sleep cycle, and are groggy for 15 minutes. Depressed people may stay groggy for 4 hours. A dawn simulator may help. These lights turn on gradually over the course of 30 to 60 minutes, reaching 250 lux while the patient is still asleep. Dawn simulators have worked in eight out of ten controlled clinical trials to help people with seasonal affective disorder, adolescents, and normal adults wake up more easily. They range in cost from $25 to $90 and some brands include PER2LED or LightenUp. Aiken says dawn simulators can improve depression, sleep quality, and cognition.
Evening and nighttime light: Bright lights and blue light, like the light that comes from electronic screens, can shut down the body’s secretion of melatonin, making people awake and alert in the evening when they should be getting sleepy. Dim light or glasses that filter out blue light allow increases in melatonin secretion in the evening, while bright light suppresses it. Missing this early melatonin pulse creates “night owls” who have delayed sleep onset.
Because light still reaches our eyes through our eyelids as we sleep, even low-level light during the night impairs sleep, cognition, and learning, and increases the risk of depression by a hazard ratio of 1.8 (about double the risk). A 2017 study by Kenji Obayashi in the American Journal of Epidemiology found that bedroom light above 5 lux elevated rates of depression in older adults after two years of followup. Living room light averaged around 50 lux and increased depression further.
The treatment is turning off TVs, electronic screens, and cellphones in the evening or wearing blue-blocking glasses, which can be found for less than $10. Blue-blocking glasses can increase calmness and reduce anxiety, and even are effective in treating mania. Then, during sleep, wear an eye mask or get light-blocking blinds or curtains for windows. For a complete blackout, use blackout curtains, aluminum foil over windows, electric tape over LED lights, or try sleeping in the basement.
Aiken suggests that to re-instate healthy sleep patterns, people should institute virtual darkness from 6pm to 8am, including wearing blue-blocking glasses when out of bed. Then they should institute total darkness or wear an eye mask when in bed. When symptoms improve, this routine can gradually be shifted to begin later in the evening, such as two hours before bedtime.
Blue light filters are also available for smartphones and tablets including Apple Nightshift mode, Kindle BlueShade, and Android Twilight and Blue Light Filter.
Glasses that filter out blue light include Uvex Ultraspec 2000, 50360X ($7 on Amazon) and Uvex Skyper 351933X ($7-10 on Amazon). The website lowbluelights.com sells blue-blocking glasses from $45 and a variety of other blue-free lighting products such as lightbulbs and flashlights.
Bright light therapy for unipolar and bipolar depression: 30 minutes of bright light (7,500 to 10,000 lux) in the morning can help treat depression in unipolar and bipolar disorder and seasonal affective disorder. The effects usually take 3 to 7 days to set in, but they only last while a patient continues using the bright light in the morning. Researcher Dorothy K. Sit and colleagues found that bright light therapy in the morning sometimes caused hypomanic reactions in people with bipolar disorder, and reported in a 2018 article in the American Journal of Psychiatry that midday light therapy (from noon to 2:30pm) was also effective without this unwanted effect. However, a 2018 article by Ne?e Yorguner Küpeli and colleagues in the journal Psychiatry Research suggested that a half hour of morning light for two weeks was sufficient to bring about improvement in 81% of patients with bipolar disorder and did not cause serious side effects.
Melatonin regimen for sleep onset delay: Melatonin can be used to treat severe night-owls with a very late onset of sleep (for example, going to bed at 2 or 3am and sleeping late into the morning). Melatonin can help with sleep onset to some extent when used at bedtime, but in those with an extreme phase shift, researcher Alfred J. Lewy recommends a regimen of low dose priming with 400–500 micrograms of melatonin at 4pm and then a full dose of 3 milligrams of melatonin at midnight. The 4pm priming dose helps pull back the delayed onset of the body’s secretion of melatonin toward a more normal schedule.
Recent Cannabis Use Linked to Greater Symptoms of Anxiety and Mood Disorders and Less Response to Treatment
 In a 2018 systematic literature review published in the Journal of Clinical Psychiatry, researcher George Mamman and colleagues reported that across 12 studies of people with anxiety and mood disorders, participants who had used cannabis in the previous six months had more symptoms than those who had used less cannabis or no cannabis during that period.
In a 2018 systematic literature review published in the Journal of Clinical Psychiatry, researcher George Mamman and colleagues reported that across 12 studies of people with anxiety and mood disorders, participants who had used cannabis in the previous six months had more symptoms than those who had used less cannabis or no cannabis during that period.
The 12 studies reviewed included a total of 11,959 participants. Four studies looked at post-traumatic stress disorder (PTSD), one at panic disorder, five at bipolar disorder, and 2 at depressive disorder. In addition to finding that recent cannabis use was associated with greater symptoms, the authors of the review also found that in 10 of the 12 studies, recent cannabis use was associated with less symptom improvement in response to treatment for bipolar disorder, depression, and PTSD; including both medication and psychotherapy.
In bipolar disorder, cannabis use was associated with greater symptom severity. Cannabis use for more than one year was linked to more recurrences of mania and shortened time to a recurrence. Compared to participants with no prior use of cannabis, those with a cannabis use disorder had more depressive symptoms, including sleep troubles and loss of interest in activities one had previously enjoyed.
In PTSD, any cannabis use at the beginning of the analysis period and sustained use of cannabis over time were both linked to greater symptom severity in the four months following the beginning of the analysis.
Mammen and colleagues cautioned that these results are limited based on the differences in measurements across the 12 studies, the inpatient populations under study, and the uncontrolled nature of the cannabis the participants accessed on their own time. However, the authors suggest that the findings may inform patients’ and doctors’ conversations about whether or not to use cannabis.
Marijuana Use in Early Adolescence Triples Risk of Psychosis At Age 18
 Hannah J. Jones and colleagues reported in the journal JAMA Psychiatry in 2018 that early- and late-onset marijuana use increased the risk of psychosis at age 18 (odds ratio 3.7 to 2.97). Interestingly, early-onset cigarette use also increased risk of psychosis, but much of the link between cigarette use and psychosis disappeared after correcting for confounding variables.
Hannah J. Jones and colleagues reported in the journal JAMA Psychiatry in 2018 that early- and late-onset marijuana use increased the risk of psychosis at age 18 (odds ratio 3.7 to 2.97). Interestingly, early-onset cigarette use also increased risk of psychosis, but much of the link between cigarette use and psychosis disappeared after correcting for confounding variables.
The data on 5,300 participants born from 1991 to 1992 came from the Avon Longitudinal Study of Parents and Children. Researchers followed up with the participants about their use of marijuana and cigarettes at least three times between the ages of 14 and 19.
Editor’s Note: These data add to a host of epidemiological data that smoking marijuana doubles the risk of psychosis. Risk is further increased among people with a common genetic variant (val/val) of the gene for COMT (catechol-O-methyltransferase), which metabolizes prefrontal dopamine. The variant, which includes two valine amino acids, functions better than other variants that include methionine amino acids. People with val/met or met/met COMT genes metabolize dopamine more slowly, making them relatively protected.
The data are also pretty strong that early heavy use of marijuana is a risk factor for new onset of both bipolar disorder and schizophrenia (and not just an earlier onset in those who might have been vulnerable otherwise).
While marijuana use has become more mainstream with its legalization in many states, its recreational use still carries risks of mental illness. In addition to increasing psychosis risk, marijuana use can also make bipolar disorder more difficult to treat.
A minor component of marijuana, cannabidiol, can have some positive effects, but what you get most of when consuming marijuana is tetrahydrocannabinol (THC), which produces symptoms that resemble psychosis.
Data in rats indicate that a father rat’s use of THC as an adult increases the risk that his offspring (with which he has no contact) will be prone to opiate addiction. The effect is an epigenetic one, conveyed by chemical changes in the father’s DNA that get passed on to the next generation via changes that persist in his sperm. We don’t know if this also happens with humans. So even if you are not worried about your own health, avoiding marijuana use might be good for your children.
Longer Periods of Untreated Depression Linked to More Brain Inflammation
 A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
The study published in the journal The Lancet Psychiatry used positron emission tomography (PET scan) to examines levels of translocator protein in the brain. Higher levels of translocator protein indicate activation of microglia, the brain’s immune cells, which can respond to trauma or injury.
The study included 80 participants between the ages of 18 and 75. Ten had a history of more than 10 years of depression, ten had experienced fewer than 10 years of depression, and 30 comprised a healthy comparison group.
The best predictors of high levels of translocator protein were duration of untreated major depressive disorder, total illness duration, and duration of antidepressant exposure. These three factors explained about half of the variation in translocator protein levels. Those participants whose depression went untreated for 10 years or longer had inflammation levels 29–33% higher than those whose depression was untreated for 9 years or less.
Participants who had received antidepressant treatment appeared to avoid an average yearly increase in the extent of their microglial activation.
The study took place at Canada’s Centre for Addiction and Mental Health.
Editor’s Note: Since inflammation is a predictor of poorer response to antidepressants, these data add a further neurochemical rationale to the already strong clinical rationale for earlier and more sustained antidepressant treatment and prevention. Virtually all treatment guidelines suggest that after two or three prior unipolar depressions, patients should receive long-term (lifelong) antidepressant treatment.
There is now a large body of data, including a 2012 article by this editor Robert M. Post and colleagues in the Journal of Psychiatric Research that too many episodes can hurt the brain, and the current study adds to this perspective. Avoiding preventive treatment for too long may actually foster the development of more episodes and more treatment resistance. A good mantra is “prevent episodes, protect the brain.”
Consensus is now also building that comprehensive long-term treatment is indicated after a first manic episode. A 2013 article by Lars Kessing and colleagues in the British Journal of Psychiatry suggested that high quality initial treatment can improve the long-term course of illness. Moreover, a 2016 article by Jan-Marie Kozicky and colleagues and a 2017 article by Christine Demmo and colleagues, both in the journal Bipolar Disorders, suggest that after a first mania, cognition recovers over the next year only if no further episodes occur in that time.
Playing Tackle Football Before Age 12 May Be Bad for the Brain
A 2017 study found that men who began playing American tackle football before age 12 were more likely to have depression, apathy, problems with executive functioning, and behavioral issues in adulthood than their peers who began playing football after age 12. Duration of football play did not seem to matter—those men who stopped playing football after high school were just as likely to be affected in adulthood as those who went on to play football in college or professionally.
The study by Michael L. Alosco and colleagues was published in the journal Translational Psychiatry. It included 214 men (average age 51) who had played football in their youth, but not other contact sports. The men reported their own experiences with depression, apathy, cognitive function, and behavioral regulation. Those who began football before age 12 were twice as likely to report impairment in behavioral regulation, apathy, and executive function than those who began playing later. Those who started younger were also three times more likely to have clinical depression in adulthood than those who started older.
According to Alosco and colleagues, between ages 9 and 12, the brain reaches peak maturation of gray and white matter volume, and synapse and neurotransmitter density also increases. The repeated head injuries that can occur during youth football play during this time may disrupt neurodevelopment, with lasting negative effects.
One drawback to the study was that recruitment was not random—men who volunteered for the study might have done so due to a recognition of their own cognitive problems. However, the results suggest more study is needed, and caution is encouraged when making decisions about youth football participation. Some youth football leagues have begun placing greater limits on the type of contact allowed during play.
Children Who Are Bullied Have Poorer Mental Health
A 2017 study of twins between the ages of 11 and 16 found that being bullied around age 11 caused anxiety, depression, hyperactivity and impulsivity, inattention, and conduct problems, some of which lasted for years. Participants recorded their experiences with physical or verbal bullying, social manipulation, and property attacks (trying to break one’s belongings, for example).
The effects of bullying decreased over time. The bullied children were still significantly more anxious than their non-bullied twins two years later, but this difference faded by the five-year mark. However, paranoid thoughts and cognitive disorganization did persist for 5 years.
The twin study design helped researchers zone in on the causal effect bullying might have on the children’s mental health, rather than other factors the twins shared, such as genetics or family environment. The study included 11,108 twins born in England and Wales.
The research by Timothy Singham and colleagues was published in the journal JAMA Psychiatry. Interestingly, the researchers found that prior mental health difficulties increased children’s likelihood of being bullied, such that being bullied could be considered a symptom of preexisting vulnerabilities. Singham and colleagues suggest that in addition to interventions to reduce bullying and address familial factors that might make children susceptible to bullying, children should also be taught resilience skills.