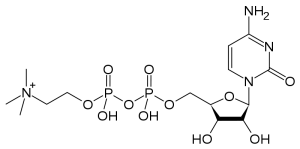
The Natural Substance Citicoline May Be Useful in Bipolar Disorder with Comorbid Stimulant Abuse
Sherwood Brown and colleagues from the University of Texas Southwestern Medical Center have completed a successful placebo-controlled trial of citicoline for bipolar and unipolar depression with comorbid methamphetamine dependence. Forty-eight participants with methamphetamine dependence and either unipolar or bipolar depression were randomized to either citicoline (2000 mg/day) or placebo for 12 weeks. Those receiving citicoline had significantly greater improvement in scores on the Inventory of Depressive Symptoms compared with those who received placebo, and patients receiving citicoline stayed in the study significantly longer, with completion rates of 41% on citicoline and 15% on placebo.
In 2007, the same team of investigators reported in the Journal of Clinical Psychopharmacology that citicoline had positive effects in bipolar patients with cocaine dependence, who experienced significant decreases in cocaine use and fewer cocaine-positive urine tests while taking citicoline.
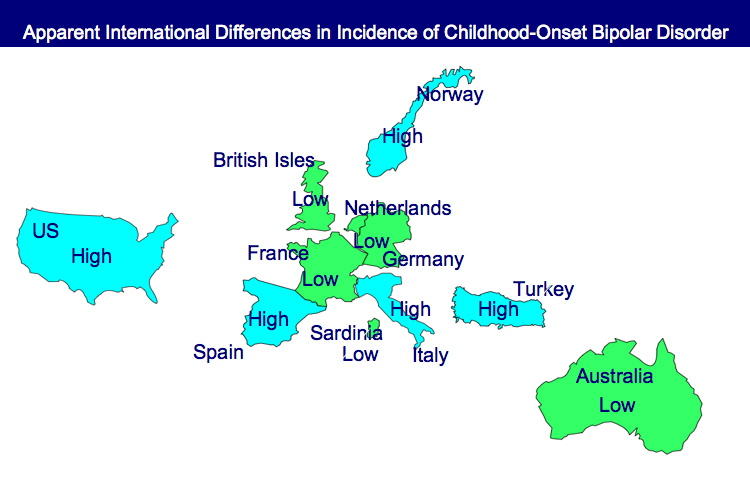
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more
Preventing Recurrent Mood Episodes
Psychotherapy and psychoeducational approaches, long-term psychopharmacology, and combination therapy all play a role in preventing recurrent mood episodes.
Psychotherapeutic and Psychoeducational Approaches Are Critical
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March indicated that cognitive-behavioral therapy (CBT) and individual and group psychoeducational approaches enhance both short- and long-term outcomes for patients with bipolar illness. These studies add to an already substantial literature that shows that focused psychotherapies (such as cognitive/behavioral, interpersonal, and social rhythms therapies) and psychoeducation are superior to treatment as usual.
These therapies can provide a variety of approaches to stress management and reduction, and can enhance family and interpersonal communication. Another way these focused psychotherapeutic approaches help patients is by demonstrating the benefits of effective long-term preventive treatment and encouraging its consistent use.
Without consistent prophylactic treatment, patients are at high risk for recurrences and their subsequent psychosocial and neurobiological consequences. Greater number of prior episodes is associated with an increased risk of psychosocial dysfunction, treatment resistance, cognitive dysfunction, medical comorbidities, and even dementia in old age.
After the jump: preventive psychopharmacology and combination therapy. Read more
Anticonvulsant Zonisamide (Zonegran) May Treat Alcohol Abuse
Albert Arias and collaborators from the University of Connecticut Health Center presented a study of zonisamide in which the drug provided significant benefits over placebo in patients with primary alcoholism (i.e., not with comorbid bipolar illness). Treatments began at 100 mg/day and increased to a maximum of 500 mg/day.
EDITOR’S NOTE: If replicated, this study would place zonisamide in a category with topiramate (Topamax), which has also been shown to decrease alcohol intake and craving. Both drugs also share the ability to cause minor weight loss as a potentially positive side effect, and both drugs have also proven effective in double-blind studies in the treatment of bulimia.
However, four double-blind, placebo-controlled studies found that topiramate did not have acute antimanic efficacy. Zonisamide has not been studied in a systematic fashion, but open studies suggest its potential utility in mania and, to a lesser degree, in depression.
Since zonisamide may have positive effects on mood in patients with bipolar disorder, and there is now placebo-controlled documentation of its efficacy in primary alcohol abuse disorders, its ultimate potential utility in patients with bipolar disorder and comorbid alcoholism deserves consideration.