Ziprasidone Improves Mood With Possible Weight Loss Side Effects
 In an open study of bipolar disorder treatment, Shefali Srivastava, Terence Ketter and colleagues at Stanford University evaluated ziprasidone as an aid to patients unresponsive to other medications. This study was part of the multi-center research program Systematic Treatment and Evaluation Program for Bipolar Disorder, or STEP-BD. During naturalistic treatment, ziprasidone was added to an average of 3.6 other psychotropic medications and 1.2 other nonpsychotropic medications patients had already been prescribed. The researchers found substantial improvement in mood with ziprasidone, particularly in the patients who had symptomatic levels of depression at baseline. The research team also observed a mean weight decrease from 195 + 50lbs at baseline to 183 + 47lbs at the final visit, with 34.3% of the patients achieving at least a 7% weight loss with ziprasidone.
In an open study of bipolar disorder treatment, Shefali Srivastava, Terence Ketter and colleagues at Stanford University evaluated ziprasidone as an aid to patients unresponsive to other medications. This study was part of the multi-center research program Systematic Treatment and Evaluation Program for Bipolar Disorder, or STEP-BD. During naturalistic treatment, ziprasidone was added to an average of 3.6 other psychotropic medications and 1.2 other nonpsychotropic medications patients had already been prescribed. The researchers found substantial improvement in mood with ziprasidone, particularly in the patients who had symptomatic levels of depression at baseline. The research team also observed a mean weight decrease from 195 + 50lbs at baseline to 183 + 47lbs at the final visit, with 34.3% of the patients achieving at least a 7% weight loss with ziprasidone.
Mean trial duration was 860 + 700 days, with no subsequent psychotropic agents added in 51.2% of the patients who had a mean trial duration of 221 + 272 days. Ziprasidone was discontinued in 57.3% of the 82 trials after a mean of 208 + 364 days. This was due to side effects in 26.8% of the participants and due to inefficacy for mood in 23.2%.
The investigators concluded that in bipolar patients treated naturalistically with complex pharmacotherapy, ziprasidone decreased overall bipolar illness severity, was helpful in patients with substantial depression at baseline, and also yielded clinically significant weight loss in about one-third of the patients.
Editor’s note: These data are notable because they support ziprasidone’s pattern of weight neutrality and because of the overall improvement in mood symptomatology the drug brought about. Read more
Long-Term Treatment with Lithium, Valproate, or Carbamazepine: Lithium Best for Most Patients
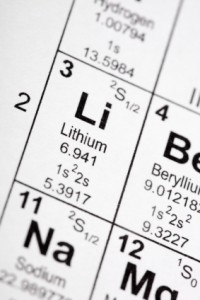 Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
The team followed 225 outpatients for up to 124 months, or until they had a manic or depressive episode or dropped out of the study during a well phase. Ninety-eight patients took lithium, 78 took valproate, and 50 took carbamazepine. Fifty-two percent of the participants dropped out of the study during a well phase.
One hundred three patients (45.8%) had either a manic or depressive episode during the study. This included 36.7% of the patients taking lithium, 55% of patients taking valproate, and 50% of patients taking carbamazepine. Median time until a first episode was 45 months for the entire sample, 36 months for those patients on valproate, 42 months for those on carbamazepine, and 81 months for those on lithium. A statistical analysis known as a Cox regression model indicated that patients taking valproate had a significantly higher risk of having a manic or depressive episode than those taking lithium.
Editor’s note: These naturalistic data are highly consistent with a number of more controlled clinical studies. In particular, the BALANCE study by Geddes et al. (2010) reported that lithium was superior to valproate on most outcome measures in a two-year randomized study, and that the combination of lithium and valproate was significantly better than valproate alone. Read more
Methylene Blue Successfully Augments Lamotrigine in the Treatment of Bipolar Disorder
 In a double-blind, placebo-controlled trial for patients with bipolar disorder, Martin Alda and colleagues from Dalhousie University in Halifax, Nova Scotia found that the compound methylene blue was an effective augmentation for mood stablizers. Methylene blue inhibits nitric oxide synthetase and guanylate cyclase, the overproduction of which might be associated with neuronal damage. Since bipolar disorder has consistently been associated with neuronal and glial cell dysfunction and loss, methylene blue could be a promising treatment.
In a double-blind, placebo-controlled trial for patients with bipolar disorder, Martin Alda and colleagues from Dalhousie University in Halifax, Nova Scotia found that the compound methylene blue was an effective augmentation for mood stablizers. Methylene blue inhibits nitric oxide synthetase and guanylate cyclase, the overproduction of which might be associated with neuronal damage. Since bipolar disorder has consistently been associated with neuronal and glial cell dysfunction and loss, methylene blue could be a promising treatment.
Methylene blue turns urine blue, so in place of a placebo the researchers used very low doses (15 mg daily) of methylene blue compared with the active dose of 195 mgs daily.
Thirty-seven patients were enrolled in the randomized 26-week trial, and all patients were treated with lamotrigine as their primary mood stabilizer and with any additional medications they were already taking. Patients entered in a well or euthymic state (n =20), mildly depressed (n=14), or while minimally cycling (n = 3).
Scores on both the Montgomery-Asberg Depression Rating Scale and the Hamilton Rating Scale for Depression improved significantly, with an effect size of 0.47 and 0.42, respectively. Hamilton Anxiety Rating Scale scores also improved significantly with an effect size of 0.46.
Methylene blue was well tolerated, with only transient and mild side effects observed. However, the FDA has issued a warning that using methylene blue with serotonin active agents can lead to a severe serotonin syndrome (because methylene blue is a potent inhibitor of MAO-A and will increase brain serotonin levels when used in conjunction with serotonin active antidepressants). Symptoms of serotonin syndrome can include confusion, hyperactivity, sweating, fever, shivering, diarrhea, trouble with coordination, and even seizures.
The researchers at Dalhousie University concluded that methylene blue used as an adjunctive medication to lamotrigine and other previously inadequately effective agents (only those which are NOT serotonin active) significantly improved depression and anxiety in patients with bipolar disorder. They proposed further exploration of the mechanisms involved in this change, with the possibility that other drugs with similar actions could also be effective in this disorder.
Dopamine D2 and D3 Agonist Pramipexole May Enhance Cognitive Function in Bipolar I Disorder
Anil Malhotra from the Zucker Hillside Hospital found that pramipexole (Mirapex), a dopamine D2 and D3 agonist used in the treatment of Parkinson’s disease, improved measures of processing speed and working memory in euthymic bipolar patients (whose average age was 42) when compared with placebo in an adjunctive clinical trial.
Editor’s Note: Bipolar patients in a euthymic phase have consistently been shown to have some degree of cognitive dysfunction that is typically correlated with the number of prior depressive and/or manic episodes they have experienced. This is one of the first studies to directly target this cognitive dysfunction with a pharmacotherapeutic agent.
Pramipexole may be of additional value among depressed patients, because in two small, placebo-controlled studies, one led by Carlos Zarate at the National Institute of Mental Health and one led by Joseph F. Goldberg in New York, pramipexole has been shown to exert acute antidepressant effects in bipolar patients in the depressive phase of the illness. The new data from Malhotra raise the possibility that there could be a two-for-one benefit when pramipexole is used in the depressive phase of bipolar illness—improvement in both depression and cognition.
Other approaches to improving cognition in patients with bipolar disorder
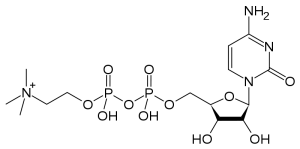
The Natural Substance Citicoline May Be Useful in Bipolar Disorder with Comorbid Stimulant Abuse
Sherwood Brown and colleagues from the University of Texas Southwestern Medical Center have completed a successful placebo-controlled trial of citicoline for bipolar and unipolar depression with comorbid methamphetamine dependence. Forty-eight participants with methamphetamine dependence and either unipolar or bipolar depression were randomized to either citicoline (2000 mg/day) or placebo for 12 weeks. Those receiving citicoline had significantly greater improvement in scores on the Inventory of Depressive Symptoms compared with those who received placebo, and patients receiving citicoline stayed in the study significantly longer, with completion rates of 41% on citicoline and 15% on placebo.
In 2007, the same team of investigators reported in the Journal of Clinical Psychopharmacology that citicoline had positive effects in bipolar patients with cocaine dependence, who experienced significant decreases in cocaine use and fewer cocaine-positive urine tests while taking citicoline.
Depression More Likely Among Perimenopausal Women with Bipolar Disorder
Researchers found that among women with bipolar disorder, those in the menopausal transition period were significantly more likely to be depressed than premenopausal women in the sample, and that the increased proclivity for depression continued in post-menopausal women as well. Wendy Marsh, Terrence Ketter, Sybil Crawford, Julia Johnson and Anthony Rothschild studied 521 women of reproductive age, 107 women in the menopausal transition period, and 145 post-menopausal women in a multi-site treatment enhancement program for bipolar disorder (STEP-BD).
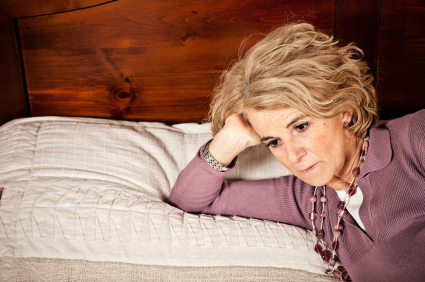
The women of reproductive age ranged from 28-38 years old, and the women in the menopausal transition period averaged 42 years old and 365 days past their last menstrual period.
Women in the menopausal transition were less likely to experience a manic episode compared with reproductive aged women, and those who were post-menopausal had the least likelihood of experiencing a manic episode. These data are consistent with others in the literature that suggest that the menopausal transition may be associated with an increased proclivity to depressive episodes.
These data also raise the question of whether hormone replacement therapy in the late menopausal transition phase may be a useful adjunct for treatment-resistant depression.
The Role of Calcium in Genetic Vulnerability, Pathophysiology, and Treatment Of Bipolar Illness
One of the most consistent findings in biological psychiatry is that levels of intracellular calcium in blood elements (platelets and white cells) are higher than normal in patients with mood disorders, particularly bipolar disorder. These data are now supported by genome-wide association studies that have identified a relationship between alterations in a calcium channel and vulnerability to bipolar illness. The specific alteration is in the alpha-IC subunit of the L-type calcium channels, otherwise referred to as CACNA1C. These findings were initially reported by one group funded by the Welcome Trust, a charitable organization that funds health research, in a series of studies that included thousands of patients and controls. Investigator Pamela Sklar later replicated these findings in another large independent sample.
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry, investigator Tyson Tragon reported that there were higher levels of CACNA1C in the cingulate cortex in autopsy specimens of those with bipolar illness than in controls. In a study of mice, some of which had the gene for the glutamate receptor subunit GLuR6 knocked out (i.e. production of the gene was artificially limited), the researchers found that the L-type dihydropyridine calcium channel blocker nimodipine decreased hyperactivity, amphetamine super-sensitivity, risk-taking behavior, and aggression in those with the gene removed. The dihydropyridine-type drugs like nimodipine also decreased stress-related immobilization in the wild type (the animal with normal genes) but not the knockout animals (the ones lacking GLuR6). These data suggest that alterations in a subunit of the dihydropyridine-responsive L-type calcium channel are a risk factor for bipolar illness, a brain abnormality in those who have the illness, and relevant to behavioral/pharmacological models.
Several research groups have noted that treatment with the L-type calcium channel blocker nimodipine (Nimotop) can sometimes have positive effects in mania and depression in those poorly responsive to lithium carbonate. This has been documented by Pazzaglia and Post in double blind off-on-off-on clinical trials (i.e. during off trials patients received placebo and during on trials patients received nimodipine, but the raters were unaware which pill the patient had received). In several instances, a positive response continued when the patient was switched from nimodipine to another dihydropyridine, isradapine (DynaCirc), but not when patients were switched to a different L-type calcium channel blocker, the phenylalkylamine verapamil (sold under the names Calan, Covera, Isoptin, and Verelan), which acts at a slightly different site on the channel. Read more
Schizophrenia v. Bipolar Disorder: Different Risk Factors
 Robin Murray gave a plenary presentation at the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, in which he indicated that the genetic risk for schizophrenia and other major mental disorders may be overestimated. He suggested that even in identical twins there are considerable differences in incidence of major psychiatric illnesses, and sharing an environment could further inflate the appearance of genetic risk.
Robin Murray gave a plenary presentation at the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, in which he indicated that the genetic risk for schizophrenia and other major mental disorders may be overestimated. He suggested that even in identical twins there are considerable differences in incidence of major psychiatric illnesses, and sharing an environment could further inflate the appearance of genetic risk.
Evidence of some genetic vulnerability factors, such as neuregulin, disbindin, DISC-1, zinc finger transcription factors, and neurexin, has been replicated. However, these genes appear to contribute only about 1% of the vulnerability to schizophrenia or bipolar illness. Copy number variations (CNVs, extra or missing copies of a gene, which may alter its activity) and gene micro-deletions (in which small bits of DNA are missing) have been found in about 5% of patients with schizophrenia, in some patients with autism and mental disabilities, but not in those with bipolar illness.
Murray emphasized the importance of psychosocial and neuromotor markers of neural development in determining risk of subsequent major psychiatric illness, rather than the relatively weak genetic effects. He cited the work of MacCabe (2009), who collected information from 907,000 individuals in Sweden. Their scholastic achievement at age 15?16 was rated, and hospitalizations for psychosis were recorded from age 17?31. Of the 315,000 followed for the long term, 493 developed schizophrenia and 208 developed bipolar disorder.
Predictors of cognitive and motor development in these two major psychiatric illnesses appeared to differ. In those who went on to develop schizophrenia, there was a slower rate of motor development, receptive language, and overall IQ in adolescence, while in those who went on to develop bipolar disorder, there was a faster rate of motor development, more language facility, and higher IQ in adolescence.
Uric Acid Increases During Mania
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, Giacomo Salvadore reported that significantly higher levels of uric acid are found in patients with mania compared with normal controls.
Editor’s note: This study was particularly interesting because there was a highly significant difference between patients and controls, with very few values overlapping. The data suggest the possibility that uric acid may be a useful biological marker for mania, and is one that should be studied in childhood-onset bipolar illness to determine whether uric acid is a marker for mania in children as well.
Allopurinol, a widely used treatment for gout that reduces levels of uric acid in the blood, is an effective antimanic agent (based on data from two placebo-controlled studies, one by Machado-Vieira et al. and one by Akhondzadeh et al.). The new data on uric acid raise the possibility that high levels of uric acid may be a specific predictor of responsiveness to Allopurinol, although this hypothesis has not yet been explored.
In an article by Chung et al. just published in Psychiatry Research, it was reported that in a very large epidemiological study in Taiwan, patients with bipolar disorder have increased risk of gout.
Track Your Moods with Life Charting
If you have unipolar depression or bipolar disorder and are having trouble stabilizing your mood, we recommend nightly charting of mood, medications and side effects on the easy-to-use Monthly Mood Chart Personal Calendar (pictured below) or the National Institute of Mental Health Life Chart (NIMH-LCM), both of which are available for download.
Sample Mood Chart
Click on the Life Charts tab above to download the personal calendar, which includes space for rating mood, functioning, hours of sleep, life events, side effects, and other symptoms such as anxiety. Then bring the chart to each visit with your physician to help in the assessment of treatments.
Life charting can help determine which medications are working partially and need to be augmented further, and which need to be eliminated because of side effects. Since there are now many potential treatments for depression and bipolar disorder (some FDA-approved and some not), a careful assessment of how well each new treatment works for a particular patient is essential to finding the optimal treatment regimen.